(Press-News.org) Using more sensitive and frequent repeat testing of a blood test that indicates heart injury to guide the treatment of low-risk patients with symptoms of a possible heart attack resulted in patients being discharged earlier and receiving fewer cardiac stress tests but did not improve patient outcomes after one year, according to research presented at the American College of Cardiology's 70th Annual Scientific Session. In fact, a subset of patients receiving this more sensitive and frequent blood testing protocol were more likely to have a heart attack or to die during the one-year follow-up period compared with patients whose treatment was informed by the results of conventional blood testing procedures.
Troponins are proteins found in heart muscle that are released into the bloodstream when the heart muscle is damaged. Clinicians test for troponin in the blood when a patient visits a hospital emergency room with chest pain or other symptoms. While the detection of troponin in the blood may signal that a patient is having a heart attack, other heart problems, including heart failure or atrial fibrillation, or conditions such as a blood clot in the lungs or kidney disease can also cause elevated troponin levels.
"We wanted to know whether giving physicians greater information about troponin levels within a zero/one-hour repeat-testing protocol would change how they managed patients and whether such changes would lead to improvements in outcomes," said Derek Chew, MBBS, MPH, PhD, professor of cardiology at Flinders University in Adelaide, Australia, and principal investigator of the study. "We found that using high-sensitivity troponin in a rapid repeat-testing protocol, with recommendations for subsequent patient management, may have changed how physicians managed patients, but this did not lead to better outcomes."
Newer, highly sensitive laboratory assays are now routinely used to measure two types of troponin, known as troponin T and troponin I, in the blood. This randomized clinical trial used an assay that can detect levels of troponin T as low as five nanograms per liter (ng/L). By contrast, older, less-sensitive troponin tests accurately detected troponin levels only down to 29 ng/L. Few randomized controlled trials have looked at whether using the newer, more-sensitive troponin tests leads to better outcomes for patients, Chew said.
The study involved 3,378 patients (median age 59 years, 53% male) who visited emergency rooms at four metropolitan centers across South Australia with chest pain or other symptoms of a possible heart attack. Patients were eligible for the study if the results of their initial electrocardiogram, which measures electrical signals in the heart, did not show clear signs that they were experiencing inadequate blood supply to the heart muscle.
The participants were randomly assigned to one of two groups. Participants in the standard-care group received a troponin test on arrival at the emergency department and a second test three hours later. Treating physicians were blinded to the test results below 29 ng/L (i.e., the less-sensitive troponin assay level), in accordance with standards of practice at the time, and subsequent care was at the treating physician's discretion.
In the intervention group, participants also received a troponin test on arrival at the emergency department, but they received a second test sooner--just one hour after the first. The results provided to physicians were unblinded, allowing them to see the troponin result down to a level of 5 ng/L (i.e., the high-sensitivity troponin assay level). Based on the initial high-sensitivity troponin test result and the change in the troponin level over one hour, participants were categorized as "rule out," "rule in" or "further observation" for a heart attack, with guidance for subsequent care provided based on their category. The study's primary endpoint was time to a heart attack or death from any cause during the 12-month follow-up period.
Follow-up data were available for 3,270 participants (108 withdrew from the study by 12 months). For 92% of participants, both initial troponin T tests showed levels below 29 ng/L. Patients in the intervention group were discharged earlier than those in the standard-care group and underwent fewer stress tests (which evaluate how well the heart performs during exercise) and slightly more angiograms (which use X-rays to assess blood flow through the arteries in the heart).
Overall, the researchers found no statistically significant differences in the number of heart attacks or deaths between the two groups during the 12-month follow-up period. However, in the subset of patients whose initial troponin levels were below 29 ng/L, 3.7% of those in the intervention group had a heart attack or died within the follow-up period, compared with 2.3% in the standard-care group. This difference amounted to a 60% increase in the risk of a heart attack or death for this subset of patients.
"This finding may imply that the practice changes observed with the use of a zero/one-hour, high-sensitivity troponin T testing protocol--fewer stress tests and slightly more angiograms--may be associated with an increase in the risk of death or a heart attack within 12 months," Chew said. "However, it is possible that this finding occurred by chance, and therefore it should be interpreted with caution. Overall, the finding may signal the continued utility of functional testing, such as stress tests, and a need for reconsideration of downstream investigations and therapies in the large presenting population with low-level troponin elevations."
INFORMATION:
This study was funded by the National Health and Medical Research Council of Australia, with supporting funding from Roche Diagnostics.
This study was simultaneously published online in the journal Circulation at the time of presentation.
Chew will be available to the media in a virtual press conference on Sunday, May 16, at 12:15 p.m. ET / 16:15 UTC.
Chew will present the study, "The Late Outcomes Of A 1-hour High Sensitivity Troponin T Protocol In Suspected Acute Coronary Syndromes: A Randomized Clinical Trial," on Sunday, May 16, at 10:45 a.m. ET / 14:45 UTC, virtually.
ACC.21 will take place May 15-17 virtually, bringing together cardiologists and cardiovascular specialists from around the world to share the newest discoveries in treatment and prevention. Follow @ACCinTouch, @ACCMediaCenter and #ACC21 for the latest news from the meeting.
The American College of Cardiology envisions a world where innovation and knowledge optimize cardiovascular care and outcomes. As the professional home for the entire cardiovascular care team, the mission of the College and its 54,000 members is to transform cardiovascular care and to improve heart health. The ACC bestows credentials upon cardiovascular professionals who meet stringent qualifications and leads in the formation of health policy, standards and guidelines. The College also provides professional medical education, disseminates cardiovascular research through its world-renowned JACC Journals, operates national registries to measure and improve care, and offers cardiovascular accreditation to hospitals and institutions. For more, visit ACC.org.
Media Contacts
Nicole Napoli
202-669-1465
nnapoli@acc.org
Thy-Ann Nguyen
703-479-3642
thyann.nguyen@curastrategies.com
Among patients who had a cardiac stent inserted after a heart attack, switching to less-potent dual antiplatelet therapy (DAPT) after 30 days was safer and more effective in preventing adverse events a year later than continuing on a high-potency DAPT regimen, according to data presented at the American College of Cardiology's 70th Annual Scientific Session.
"We have shown that, in patients who have had a heart attack and who've been treated with newer-generation stents and guideline-recommended medical therapy, de-escalation of DAPT by switching from ticagrelor to clopidogrel is completely safe and more effective than continuing to treat patients with ticagrelor," said Kiyuk Chang, MD, professor of Cardiology, Division of Internal Medicine at the Catholic University of ...
People with extremely high levels of triglycerides (a type of fat in the blood) and a specific genetic profile saw a substantial reduction in triglycerides after taking the human monoclonal antibody evinacumab compared with those taking a placebo, in a study presented at the American College of Cardiology's 70th Annual Scientific Session.
Severe hypertriglyceridemia is a rare disorder that causes extremely high levels of triglycerides, an accumulation of fat in the blood that can lead to heart, liver and pancreatic disease. People with severe hypertriglyceridemia commonly have triglyceride levels of 1,000 mg/dL ...
Patients at high risk for cardiovascular events who had the highest levels of eicosapentaenoic acid (EPA) in their blood one year after taking daily omega-3 carboxylic acid, a prescription-grade fish oil, had similar rates of major cardiovascular events as people taking a corn oil placebo, according to a secondary analysis of the STRENGTH trial presented at the American College of Cardiology's 70th Annual Scientific Session. Researchers also found no increase in cardiovascular events among patients with the highest levels of docosahexaenoic acid (DHA) compared to placebo.
The impetus for this post-hoc analysis was to further examine the strikingly divergent results between STRENGTH and REDUCE-IT, another large, randomized clinical trial that used a ...
Dapagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, did not significantly reduce the risk of organ failure or death or improve recovery in patients hospitalized with COVID-19 who are at high risk of developing serious complications compared to placebo, according to data presented at the American College of Cardiology's 70th Annual Scientific Session. The researchers, while acknowledging the results were not statistically significant, said they were encouraged by the lower numbers of organ failure and deaths observed in patients treated with dapagliflozin and by favorable safety ...
Older patients hospitalized with acute heart failure who participated in a novel 12-week physical rehabilitation (rehab) program tailored to address their specific physical impairments had significant gains not only in physical functioning but also quality of life and depression compared with those receiving usual care, regardless of their heart's ejection fraction, according to a new study presented at the American College of Cardiology's 70th Annual Scientific Session. Participation in the program, however, did not significantly reduce rehospitalizations during the six-month follow up.
Heart failure, which ...
Taking medications to protect the heart from damage associated with adjuvant breast cancer therapy--medications that are administered in addition to surgery to remove a tumor--did not significantly improve markers of heart health two years after breast cancer treatment, according to a study presented at the American College of Cardiology's 70th Annual Scientific Session.
The researchers reported no significant differences between patients who took an angiotensin receptor blocker (candesartan cilexetil) or a beta-blocker (metoprolol succinate) compared with placebos in terms of left ventricular ejection fraction (LVEF), a measure of the heart's ability to effectively pump ...
Rivaroxaban, in addition to low-dose aspirin, significantly reduced the occurrence of total severe events of the heart, limb or brain and issues related to other vascular complications in patients with symptomatic peripheral artery disease (PAD) who underwent lower extremity revascularization, a procedure to open blocked arteries in the leg. The findings, presented at the American College of Cardiology's 70th Annual Scientific Session, expand on earlier data and underscore the broad absolute benefits of this strategy in this high-risk patient population, researchers said.
"To our knowledge, this is the first time that the addition of low-dose rivaroxaban to aspirin has been clearly shown to reduce ...
In patients who had a coronary stent inserted after experiencing the most severe type of heart attack, the use of a technique that measures blood flow and pressure through a partially blocked artery to determine if a second stenting procedure is needed did not improve outcomes and was more costly than using angiography, or a heart X-ray, alone to guide the procedure, according to research presented at the American College of Cardiology's 70th Annual Scientific Session.
"The strategy of using fractional flow reserve (FFR) to guide the stenting procedure is not superior to the standard technique of using angiography to treat additional partially blocked arteries," said Etienne Puymirat, MD, professor of cardiology at the University of Paris, director of intensive care at the Georges ...
HOUSTON - (May 17, 2021) - In an important step toward the clinical application of synthetic biology, Rice University researchers have engineered a bacterium with the necessary capabilities for diagnosing a human disease.
The engineered strain of the gut bacteria E. coli senses pH and glows when it encounters acidosis, an acidic condition that often occurs during flareups of inflammatory bowel diseases like colitis, ileitis and Crohn's disease.
Researchers at the University of Colorado (CU) School of Medicine used the Rice-created organism in a mouse model of Crohn's disease to show acidosis activates a signature set of genes. The corresponding ...
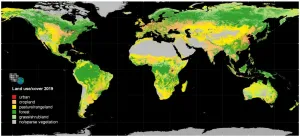
Humans leave their "footprints" on the land area all around the globe. These land-use changes play an important role for nutrition, climate, and biodiversity. Scientists at the Karlsruhe Institute of Technology (KIT) combined satellite data with statistics from the past 60 years and found that global land-use changes affect about 32 percent of the land area. This means that they are about four times as extensive as previously estimated. The researchers publish their findings in the scientific journal Nature Communications.
Whether it is deforestation, urban growth, agricultural expansion, or reforestation - land-use changes are diverse and have ...