(Press-News.org) The heightened risk of death after admission to hospital at the weekend--the so-called 'weekend effect'--is a feature of several developed countries' healthcare systems, and not just a problem for hospitals in England, reveals research published online in BMJ Quality & Safety.
The international nature of the findings suggests that this is a systematic phenomenon that not only crosses time, but also space, say the researchers.
In a bid to look in more detail at the evidence for the link between higher rates of death for patients admitted to hospital at weekends compared with other days of the week, the researchers drew on international data from the Global Comparators project.
This is a database to which more than 50 different hospitals in the UK, USA, Australia, The Netherlands, Italy, Spain, Belgium, Finland, Norway and Denmark now contribute outcomes data on admissions.
For the current study, the researchers looked at data on almost 3 million admissions between 2009 and 2012 from 28 metropolitan teaching hospitals in England, Australia, USA and The Netherlands.
They focused on deaths occurring in hospital within 30 days of an emergency admission or planned (elective) surgery.
They found that, after taking account of influential factors, the risk of dying within 30 days was higher for emergency admissions at weekends at hospitals in three out of the four countries.
This risk was 8% higher in 11 hospitals in England, 13% higher in five of the US hospitals, and 20% higher in six Dutch hospitals.
There was no significant daily variation in the heightened risk of death within 30 days for emergency admissions at weekends in the Australian hospitals, and these hospitals between them had the largest proportion of emergency admissions. But a weekend effect became apparent for deaths within 7 days.
And, across the board, all patients admitted at the weekend for planned surgery were more likely to die within 30 days than those admitted on other days of the week, the findings showed.
Furthermore, the data indicated a 'Friday effect' for patients undergoing planned surgery in the hospitals in The Netherlands: their risk of death was 33% higher if admitted on a Friday than on a Monday.
The researchers acknowledge that the number of participating hospitals in this study was small, but these hospitals represent varying models of service delivery, they say.
"Although these results are limited to the small number of participating hospitals, the international nature of our database suggests that this is a systematic phenomenon affecting healthcare providers across borders," they write.
The researchers speculate on the reasons for the findings, pointing out that no one single factor is going to be responsible.
They suggest that certain diagnoses and procedures may be particularly sensitive to reduced access to test results and diagnostics at weekends. Similarly, weekend staff may be fewer in number and less experienced, while patients requiring urgent care may have to wait longer, which might affect the success of any treatment and interventions.
In a linked editorial, Professor Richard Lilford and Dr Yen-Fu Chen of Warwick Medical School, caution against rushing to conclusions, on the grounds that the data are unlikely to be nationally representative.
They suggest that the time has come to focus more on shedding light on the causes behind the 'weekend effect' rather than just proving its existence across time and space.
"Understanding the weekend effect is an extremely important task since it is large, at about 10% in relative risk terms and 0.4% in percentage point terms. This amounts to about 160 additional deaths in a hospital with 40,000 discharges per year," they write.
"But how much of the observed increase results from service failure? And here is the rub, for while a 0.4 percentage point represents a large, potentially scandalous, number of deaths, it is quite a small proportional change," they add.
INFORMATION:
A new smartphone app warns drinkers if they go over the recommended maximum daily/weekly units of alcohol, to help them better manage their intake, reveals a commentary published in the online journal BMJ Innovations.
The Alcohol Tracker, which has been developed by doctors and based on the clinical evidence of what works best, also provides built-in psychological therapies and helpline links for users to help steer them away from hazardous drinking.
Excess alcohol kills millions worldwide every year, but many available smartphone apps to manage drinking are not informed ...
1. For patients with no history of stroke, even very small brain lesions increase risk for death
Free abstract: http://www.annals.org/article.aspx?doi=10.7326/M14-2057
URL goes live when embargo lifts
For asymptomatic patients with no history of clinical stroke, having even very small brain lesions (less than 3 mm) detected by magnetic resonance imaging (MRI) triples their risk for stroke and death, according to a study published in Annals of Internal Medicine. Having both very small and larger lesions increases the risk to eight-fold.
Subclinical brain infarctions ...
Scientists with the University of Mississippi Medical Center (UMMC) and colleagues found that very small brain lesions noted on brain imaging that would typically be disregarded by clinicians are associated with a heightened risk of stroke and death. The findings are in today's (July 7, 2015) Annals of Internal Medicine.
The discovery about these tiny lesions -- areas of the brain where tissue may have been damaged by injury or disease -- may help physicians identify people at risk of stroke and death as early as middle age, even when they are displaying no symptoms of ...
A study in the online edition of Annals of Internal Medicine suggests that coronary artery calcification (CAC) scans could help physicians identify patients at risk for premature death.
According to the National Institutes of Health, a CAC is an x-ray test that looks for specks of calcium in the walls of the coronary arteries. These specks of calcium are called calcifications and are an early sign of coronary artery disease.
Researchers from Emory University School of Medicine, led by Leslee Shaw, PhD, professor of cardiology, collected and assessed CAC scores and ...
In a first-of-its-kind study, researchers have investigated the impact of different walking aids on patients with chronic obstructive disease (COPD).
Walking with the help of a rollator (a frame with wheels, handlebars, and a built-in seat) resulted in the longest distance walked and most time spent walking. The use of walking with assistance of a draisine (a bicycle without pedals) improved walking speed with fewer strides but did not improve the time spent walking by COPD patients to cover a longer distance. "Patients with COPD walked significantly further and longer ...
In a study of 1159 males who illicitly used amphetamines, half of participants said drug use had no impact on their sexual functions, while the other half reported impacts such as reduced erectile rigidity and sexual satisfaction, enhanced orgasmic intensity, and delayed ejaculation.
"Compared with 211 matched controls, amphetamine users were twice as likely to experience erectile dysfunction," said Dr. Bang-Ping Jiann, senior author of The Journal of Sexual Medicine study.
Amphetamines are a group of drugs that stimulate the central nervous system and contain ingredients ...
Researchers have long had reason to hope that blocking the flow of calcium into the mitochondria of heart and brain cells could be one way to prevent damage caused by heart attacks and strokes. But in a study of mice engineered to lack a key calcium channel in their heart cells, Johns Hopkins scientists appear to have cast a shadow of doubt on that theory. A report on their study is published online this week in Proceedings of the National Academy of Sciences.
"We confirmed that this calcium channel is important for heart function," says senior investigator Mark Anderson, ...
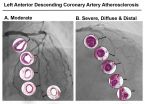
July 6, 2015 CHAPEL HILL, NC - Insulin resistance affects tens of millions of Americans and is a big risk factor for heart disease. Yet, some people with the condition never develop heart disease, while some experience moderate coronary blockages. Others, though, get severe atherosclerosis - multiple blockages and deterioration of coronary arteries characterized by thick, hard, plaque-ridden arterial walls. Researchers at the UNC School of Medicine created a first-of-its-kind animal model to pinpoint two biomarkers that are elevated in the most severe form of coronary disease.
The ...
Researchers have found several key differences among people who receive hospice care--which maintains or improves the quality of life for someone whose condition is unlikely to be cured--in assisted-living facilities (ALFs) compared with people who receive hospice care at home.
People receiving hospice care in ALFs were more likely to be older and female than people who received hospice care at home. Also, people living in ALFs enrolled in hospice care much earlier than patients living in home settings. This allowed them to receive more help from the hospice team before ...
Lyme disease is currently estimated to affect 300,000 people in the U.S. every year, and blacklegged ticks, the disease's main vector, have recently flourished in areas previously thought to be devoid of this arachnid.
A new study finds that the newly detected tick populations likely arose mainly from southern populations that migrated to nearby northern locations.
"The fine temporal and spatial scale of the samples analyzed allowed for precise estimates of the rate, timing, and direction of individual migratory events," said Dr. Camilo Khatchikian, lead author of the ...