(Press-News.org) A national screening programme targeted at those men who are genetically pre-disposed to prostate cancer, and involving a blood test and MRI scan before an invasive biopsy, could prevent one in six prostate cancer deaths and significantly reduce over-diagnosis, finds a new study led by UCL researchers.
Prostate cancer is the most common form of cancer in men with around 130 new cases diagnosed in the UK every day and more than 10,000 men a year dying as a result of the disease. However, unlike breast and cervical cancer there is currently no national screening programme for this disease in the UK.
Currently, men suspected of having prostate cancer have a blood test that detects raised levels of the prostate-specific antigen (PSA)*. Following the UCL-led PRECISION trial, the National Institute of Clinical Excellence (NICE) guidelines**, also now advises that all men with a positive PSA result have an MRI scan prior to biopsy - as this has been shown to better distinguish and increase detection of aggressive cancers whilst reducing over-diagnosis and unnecessary treatment of insignificant cancers.
Building on this, researchers say recently discovered genetic markers that predict prostate cancer risk could also complement a PSA test and MRI scan. A polygenic test*** - not yet widely available - can identify individuals with high-risk prostate cancer genes (biomarkers) and help predict when an individual is likely to start to benefit from screening.
Explaining the study, lead author Dr Tom Callender (UCL Division of Medicine) said: "Prostate cancer is a leading cause of death from cancer amongst men, but there is no screening programme because the harms of screening are considered to outweigh the benefits.
"However those at higher genetic risk are more likely to benefit from screening and less likely to be harmed.
"For this benefit-harm and cost-effectiveness analysis, we asked how effective a four-yearly PSA screening for all men aged 55 to 69 would be versus more targeted checks for those at higher risk of the disease based on their age and genetic profile.
"We also asked, what the impact would be of those with a positive PSA blood test having an MRI scan before a biopsy, in the context of a prostate cancer screening programme."
In this modelling study, published in JAMA Network Open, researchers created a hypothetical cohort of 4.5 million men, representing the number of men aged 55 to 69 in England, and simulated the health outcomes of introducing either 'age-based' and 'risk-tailored' screening programmes into this population.
The age-based diagnostic pathway modelled a screening programme in which all men aged between 55 and 69 would receive a PSA test every four years, and if the test was positive this would be followed by MRI and, if required, a biopsy.
The risk-tailored pathway modelled a screening programme in which men would get a PSA test (followed by MRI and biopsy if required) if and when their risk - determined by their age and polygenic risk score (genetic profile) - reached a certain threshold.
Health outcomes, including prostate cancer deaths prevented and unnecessary diagnoses averted, along with screening costs (i.e the cost effectiveness measure) were compared for no screening, universal age-based screening and more targeted risk-based screening using a range of risk thresholds, both with and without the use of an MRI scan before biopsy in those with a positive PSA blood test.
The scenario generating the most benefits, the researchers concluded, would be to screen men with a 3.5% risk of getting prostate cancer over the next 10 years - that is, roughly half of all men aged 55 to 69. Such a programme could prevent up to 16% of prostate cancer deaths - nearly one in six deaths and reduce overdiagnosis by 27%. Screening men at this threshold (3.5%) would also be more cost-effective than screening all men aged 55 to 69.
Screening all men in that age group (the age-based screening pathway) would result in the most prostate cancer deaths prevented (20%). However, targeted risk-based screening prevents a similar number of deaths whilst reducing the number of over-diagnosed cancers (those cancers that end up being harmless) by up to 70% (depending on the risk threshold used) and the number of biopsies needed by approximately one-third.
Senior author, Professor Nora Pashayan, (UCL Applied Health Research), said: "In men with a positive screening blood test, we found that using an individual's genetic profile alongside a diagnostic pathway that uses MRI scanning before biopsy, could reduce unnecessary diagnoses whilst preventing deaths from prostate cancer by detecting the cancers at an early, curable stage."
Co-author, Professor Mark Emberton, UCL Dean of the Faculty of Medical Sciences: "Our study shows that screening for prostate cancer - which could save between 16% and 20% of prostate cancer deaths - might be possible with targeted screening using genetic risk and MRI as part of the diagnostic pathway. This paves the way for further clinical trials to study the real-world implementation of such a screening programme."
INFORMATION:
This study was carried out with researchers from the University of Cambridge.
*The PSA test was previously the only test men would have to detect the presence of prostate cancer. However, this test is not a reliable indicator as it does not accurately distinguish between dangerous cancers from harmless ones - leading to both unnecessary operations and missed cancers that are harmful.
**NICE guidelines introduced in 2019 meant patients received an MRI scan following a positive PSA test. This followed the UCL-Precision trial, which found that MRI scans and targeted biopsies are better at making a positive prostate cancer diagnosis than standard biopsies.
*** A polygenic test uses a sample (blood or mouth swab) to assess numerous genetic variants. Together, these can be used to derive a polygenic risk score which can contribute to predicting an individual's risk of developing certain diseases.
What The Study Did: Experiences of Latinx patients who were hospitalized with and survived COVID-19 are described in this study.
Authors: Lilia Cervantes, M.D., of Denver Health in Colorado, is the corresponding author.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamanetworkopen.2021.0684)
Editor's Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflict of interest and financial disclosures, and funding and support.
INFORMATION:
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide ...
What The Study Did: This randomized clinical trial evaluated the effect on patient perceptions of communication, trust and empathy of surgeons who wore clear masks that showed their faces versus standard masks that obscured them during outpatient clinic visits.
Authors: Muneera R. Kapadia, M.D., M.M.E., of the University of North Carolina at Chapel Hill, is the corresponding author.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamasurg.2021.0836)
Editor's Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflict of interest and financial disclosures, and funding and support.
INFORMATION:
Media advisory: The full ...
What The Study Did: Researchers sought to quantify cancer surgical backlog and determine whether there were differences in sociodemographic and hospital characteristics among patients undergoing cancer surgery before and during the COVID-19 pandemic.
Authors: Antoine Eskander, M.D., Sc.M., of Sunnybrook Health Sciences Centre in Toronto, Canada, is the corresponding author.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamanetworkopen.2021.1104)
Editor's Note: The article includes ...
What The Study Did: In this study of face mask fit among people in China, although most people used face masks in public places, compromised protection due to suboptimal airtightness was common. The simple approach of sealing the upper edge of the face mask with an adhesive tape strip was associated with substantially improved its airtightness.
Authors: Lin Duo, Ph.D., of Fuwai Yunnan Cardiovascular Hospital in Kunming, China, and Chengye Sun, Ph.D., of the National Institute of Occupational Health and Poison Control, Chinese Center for Disease ...
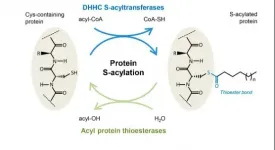
S-acylation is the process of chemically linking a lipid to protein via a thioester bond. It is an important process of the cell that regulates the localization and function of numerous proteins. It promotes lipid membrane association of the protein, for instance to the plasma membrane, Golgi apparatus, or inner nuclear membrane.
Like most biochemical processes in the cell, protein S-acylation is reversible to regulate the functions of acylated proteins. S-acylation is reversed by the enzymes acyl protein thioesterases (APTs).
To do their work, APTs have to interact with the lipid membranes that their target proteins are bound to. But even though APTs are central to the important acylation deacylation process little is known about how APTs carry ...
Every year, a new growth layer is added to the narwhal's spiralled tusk. The individual layers act as an archive of data that reveals what and where the animal has eaten, providing a glimpse of how the ice and environmental conditions have changed over its long life span (up to 50 years).
Same as rings in a tree trunk, every year a new growth layer is added to the narwhal's tusk, which grows longer and thicker throughout the animals life. Because the tusk is connected to the rest of body through blood, each new growth layer records aspects of animal physiology during the year it was formed.
An international team of researchers ...
Philadelphia, March 11, 2021--Researchers at Children's Hospital of Philadelphia (CHOP) have identified genes responsible for hematopoietic stem cell (HSC) regeneration via the assembly of the ribosome, the protein factories in cells that translate mRNA sequences into amino acid sequences. The findings, which were published in Cell Stem Cell, highlight the importance of proper ribosome assembly in stem cell regeneration and identify possible targets for future therapies for ribosomopathies, childhood disorders that lead to bone marrow failure (BMF).
"Although previous research showed that ...
BOSTON - In the last two decades, immunotherapy has emerged as a leading treatment for advanced renal carcinoma cancer (more commonly known as kidney cancer). This therapy is now part of the standard of care, but it doesn't work for all patients, and almost all patients, no matter how they respond initially, become more resistant to treatment over time. The immune system plays a critical role in kidney cancer disease progression and in response to therapies, and so a fundamental challenge in the field is to understand the underlying "immune circuitry" of this disease.
In two new studies published today in Cancer Cell, researchers from Dana-Farber Cancer Institute and the Broad Institute of MIT and Harvard used the emerging ...
For decades, researchers assumed the cosmic rays that regularly bombard Earth from the far reaches of the galaxy are born when stars go supernova -- when they grow too massive to support the fusion occurring at their cores and explode.
Those gigantic explosions do indeed propel atomic particles at the speed of light great distances. However, new research suggests even supernovae -- capable of devouring entire solar systems -- are not strong enough to imbue particles with the sustained energies needed to reach petaelectronvolts (PeVs), the amount of kinetic energy attained by very high-energy cosmic rays.
And yet cosmic rays have been observed striking Earth's atmosphere at exactly those velocities, their passage marked, for example, by the detection ...
CHAPEL HILL, NC - A first-of-its-kind study out today in JAMA Surgery suggests that patients have a more difficult time understanding and building trust with their surgeons when they cannot see the surgeon's entire face due to masking requirements. These findings have major implications for not only how surgeons are viewed and rated by their patients, but also how well a patient does during and after a surgical procedure.
"At beginning of pandemic I had a patient say, 'Dr. Kapadia, it's odd you've taken out a big part of my colon and I don't even know what you look like,'" Muneera Kapadia, MD, the study's senior author said. "It made me realize we don't have much information ...