(Press-News.org) Insomnia is a common problem in patients with schizophrenia, and a new study reinforces a close association between insomnia, more suicidal thoughts and actions and increased problems like anxiety and depression in these patients.
It also provides more evidence that keeping tabs on how patients are sleeping -- and intervening when needed -- is important to their overall care.
"We are now aware that significant insomnia is putting our patients at even higher risk for suicide, so if they are having changes in sleep patterns, if they are having significant insomnia, then we really need to hone in on those questions even more related to suicidal thinking and do what we can to help," says Dr. Brian Miller, psychiatrist and schizophrenia expert at the Medical College of Georgia at Augusta University.
Schizophrenia is clearly associated with an increased risk of suicide, with a 5-10% lifetime risk of death by suicide, that is likely the greatest within the first year of diagnosis, Miller says.
The new study in The Journal of Clinical Psychiatry looked at associations between insomnia, suicidal thoughts and attempts and disease severity in a large group of patients, 1,494 individuals diagnosed at 57 sites in the country, and enrolled in a comparative study of five different antipsychotics.
Miller and his colleagues looked at patient reports of insomnia and suicidal thoughts within the most recent two weeks, suicide attempts in the past six months and the state of their psychiatric illness when they enrolled in the study.
Nearly half of patients reported problems falling asleep or broken sleep, termed initial and middle insomnia, and 27% reported terminal insomnia where they wake up too early and cannot get back asleep.
They found insomnia a common symptom in patients with schizophrenia, with waking up too early particularly associated with current suicidal thoughts, and trouble falling and staying asleep significantly increasing the odds of a suicide attempt in the past six months.
Waking up too early was also most associated with more severe schizophrenia, including symptoms like anxiety and depression. But no matter which type of insomnia, it's bad for patients' overall health and disease, Miller says.
Studies indicate that 23-44% of patients with schizophrenia -- both those taking and not taking medications-- report problems with insomnia. Sleep architecture is a pattern of normal sleep, and sleep disturbances and abnormal sleep architecture have been found early in the schizophrenia disease process, findings which may correlate with disease severity. Disturbances in the natural body clocks, or circadian rhythms that help regulate sleep and wakefulness and other essential body functions, are known to be present in schizophrenia and are suspected to be a factor in patients' related sleep problems. A generally heightened state of arousal in patients who are hearing voices and/or paranoid also is likely a factor. Insomnia has been implicated as a predictor of hallucinations in patients, and there seems to be a bidirectional relationship between insomnia and paranoia, the investigators write.
"If you are hearing voices that are constantly saying negative, horrible things, berating you, interfering with your thinking and your activities, it can be hard to fall asleep," he says.
Miller says insomnia in his patients cuts across all ages, sexes and races.
While he has always been diligent asking patients at each visit about their sleep and counseling them on how to improve their sleep, the increasing evidence of the association with suicide and disease severity has heightened his diligence. While Miller says his colleagues across the country also tend to be diligent in regularly talking with patients about sleep, surveys have indicated that while patients with schizophrenia commonly report problems with insomnia, less than 20% of clinicians formally evaluate patients for it.
The new study suggests that insomnia is an important treatment target in schizophrenia. Interventions Miller offers include ensuring habits like avoiding caffeine as well as blue light from commons sources like televisions and smartphones, particularly in the hours before bedtime, as well as prescription and over-the-counter sleep aids.
Adjustments also can be made to the antipsychotic medication used to treat their schizophrenia since some, like clozapine, also have sedative effects. In fact, there is some evidence that insomnia and suicidal thoughts and actions are less likely in patients taking antipsychotics known to also have a sedative effect, they write, but just how needs exploration.
While he has not yet done a formal study, Miller has noted anecdotally that when his patients' sleep improves, generally their schizophrenia does as well.
"I can't think of anyone who says I am sleeping better and now my illness is worse. When you get a bad night's sleep, the world just isn't quite the same place the next day," Miller says. "It affects the way we think about things, the judgements we make, it affects our emotions." In fact, insomnia and increased suicide risk are associated with a variety of mental health issues, including depression.
The current study is the third group of patients in which Miller and his colleagues have found an association between insomnia and suicidal thoughts and actions.
Other investigators have associated sleep disturbances with suicidal thoughts in these patients but not actual suicide; others have shown, for example, nearly five times the risk of suicide attempts in patients experiencing insomnia at least three times a week.
INFORMATION:
Read the full study.
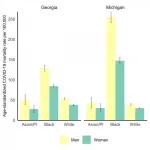
A new paper in the Journal of General Internal Medicine published by the GenderSci Lab at Harvard University shows that Black women are dying at significantly higher rates than white men, and that disparities in mortality rates among women of all races are greater than those between white women and white men.
The study is the first to quantify the inequities in COVID-19 mortality looking at both race and sex group.
"This analysis complicates the simple narrative that men are dying at greater rates of COVID-19 than women," said lead author Tamara Rushovich, Harvard Ph.D. candidate in population health sciences and lab member ...
The adult human body produces hundreds of billions of blood cells every day. This essential process unavoidably leads to the appearance of mutations in the DNA of the progenitor cells. These are known as somatic mutations because they are acquired, not inherited. While most of these mutations are innocuous, occasionally a mutation gives affected cells a competitive advantage that allows them to expand progressively, generating clonal populations of blood cells. This phenomenon is known as clonal hematopoiesis.
Now, a team of scientists at the Centro Nacional de Investigaciones Cardiovasculares (CNIC) and the Hospital Universitario Virgen de Arrixaca in Murcia has discovered that the presence of these acquired mutations in blood cells increases ...
Below please find summaries of new articles that will be published in the next issue of Annals of Internal Medicine. The summaries are not intended to substitute for the full articles as a source of information. This information is under strict embargo and by taking it into possession, media representatives are committing to the terms of the embargo not only on their own behalf, but also on behalf of the organization they represent.
1. ACP Best Practice Advice: Shorter course of antibiotics may be appropriate for some common infections
HD video soundbites of ACP's president discussing the paper are available to download at http://www.dssimon.com/MM/ACP-antibiotics-paper.
Abstract: https://www.acpjournals.org/doi/10.7326/M20-7355
Free ...
Researchers at the Human Genome and Stem Cell Research Center (HUG-CELL), hosted by the University of São Paulo's Institute of Biosciences (IB-USP) in Brazil, have developed a technique to reconstruct and produce livers in the laboratory.
The proof-of-concept study was conducted with rat livers. In the next stage of their research, the scientists will adapt the technique for the production of human livers in order in future to increase the supply of these organs for transplantation.
The study was supported by FAPESP and is reported in an article published in Materials Science and Engineering: ...
PITTSBURGH, April 5, 2021 - "Near-poor" Americans--people just above the federal poverty level but still well below the average U.S. income--who rely on Medicare for health insurance face high medical bills and may forgo essential health care, according to new research led by health policy scientists at the University of Pittsburgh Graduate School of Public Health. This is due to a coverage "cliff" in Medicaid, which supplements Medicare for people with incomes below poverty but excludes individuals above the federal poverty threshold, including the near-poor.
In a report published today in the April issue of the journal Health Affairs, the authors describe the effects of this cliff and propose solutions to fix it, with the aim of lessening barriers to care among near-poor people ...
PHILADELPHIA-- Approximately 6.5 million people are under correctional supervision in the United States on any given day. Justice-involved individuals (people currently or recently in prison or jail, on probation or parole, or arrested) experience higher rates of substance use disorders than the general population. In fact, among people with opioid use disorder (OUD), more than half have reported contact with the criminal justice system.
Numerous clinical studies have shown that medications for OUD -- specifically, methadone or buprenorphine -- lead to superior outcomes for retention in treatment, reduced illicit opioid use, and decreased opioid-related overdose rates and serious acute care compared with treatments that ...
PHILADELPHIA-- While the emergency department (ED) functions as an integral part of the United States healthcare safety net by handling all medical complaints regardless of insurance status, ED visits are expensive, and many are for lower-acuity conditions that may be amenable to care in other settings. Previous research has suggested that greater availability of urgent care centers - freestanding facilities with extended hours that staff emergency physicians, primary care physicians, or nurse practitioners, and focus on a broad range of lower acuity complaints, like rash, muscle strain, bronchitis, and urinary tract infection - helps decrease ED visits, but whether the centers reduce or increase net spending for patients ...
Even before the pandemic made telehealth a hot topic, people with minor urgent health needs had started to turn to companies that offer on-demand video chats with physicians that they don't normally see.
Insurers and employers even started buying access to this direct-to-consumer form of virtual care, hoping it might reduce in-person care, including emergency department visits.
But a new University of Michigan study casts some doubt on whether that will actually happen.
Published in the April issue of Health Affairs, the study finds that patients who had an on-demand ...
In a new study, researchers found nearly half of those who share explicit images of others without permission feel remorse after the fact and 24% try to deflect blame onto victims. Amy Hasinoff, a researcher at the University of Colorado Denver, joined Danish researcher Sidsel K. Harder, to take a deeper dive into the issue of sexual abuse and image sharing.
Hasinoff and Harder looked at how people who shared explicit images online spoke to police officers about the harmful acts they committed. While looking over cases where the image-sharer was caught and convicted, ...
People with ovarian cancer frequently receive aggressive end-of-life care despite industry guidelines that emphasize quality of life for those with advanced disease, according to a recent study.
In fact, by 2016, ICU stays and emergency department visits in the last month of life had become more common for people with ovarian cancer than they were in 2007, the earliest year from which researchers analyzed data.
The proportion of non-Hispanic Black people who turned to the emergency department for care was even higher -- double that of non-Hispanic whites. Black people were also nearly twice as likely to undergo intensive treatment, including ...