(Press-News.org) Some 16 million Americans are believed to have alcohol use disorder, and an estimated 93,000 people in the U.S. die from alcohol-related causes each year. Both of those numbers are expected to grow as a result of heavier drinking during the COVID-19 pandemic.
Yet, in a new study involving data from more than 200,000 people with and without alcohol problems, researchers at Washington University School of Medicine in St. Louis found that although the vast majority of those with alcohol use disorder see their doctors regularly for a range of issues, fewer than one in 10 ever get treatment for drinking.
The findings are published in the June issue of the journal Alcoholism: Clinical & Experimental Research.
Analyzing data gathered from 2015 through 2019 via the National Survey on Drug Use and Health, the researchers found that about 8% of those surveyed met the current criteria for alcohol use disorder, the medical diagnosis for those with an addiction to alcohol. Of these people who met the criteria, 81% had received medical care in a doctor's office or spent time in a hospital or clinic during the previous year. But only 12% reported they had been advised to cut down on their drinking, 5% were offered information about treatment, and 6% received treatment, some of whom were not referred by their doctors but sought out treatment on their own.
"It's not that these people aren't in the health-care system," said first author Carrie M. Mintz, MD, an assistant professor of psychiatry. "But although they see doctors regularly, the vast majority aren't getting the help they need."
Mintz and her colleagues evaluated data from 214,505 people. The researchers first wanted to learn whether people with alcohol use disorder had access to health care and if they did, whether they had been screened about their alcohol use; they were considered to have been screened if their doctors simply had asked how much they drink. The researchers also evaluated whether people with drinking problems had been advised to cut down on drinking, had received additional information about treatment, or had received treatment or counseling.
The researchers found that although most people with alcohol use disorder had access to health care and although 70% reported they had been asked about alcohol use, that's where the care stopped.
"Some primary care doctors may not feel comfortable telling patients they should cut down on drinking, prescribing medication to help them cut back or referring them to treatment because they don't specialize in treating alcohol misuse; but the result is that many people who need treatment aren't getting it," said senior author Laura Jean Bierut, MD, the Alumni Endowed Professor of Psychiatry. "We used to see the same thing with smoking, but when physicians became educated about smoking and learned that many of their patients wanted to quit or cut back, doctors began offering more treatment, and more people were able to quit. We think the same thing may be possible with alcohol."
Among treatments that could be prescribed are the FDA-approved medications naltrexone, acamprosate and disulfiram, as well as psychotherapy and mutual-aid approaches, such as the 12-step program used by Alcoholics Anonymous.
"Alcohol use disorder is a chronic disease, but compared to other chronic diseases, it's wildly untreated," Bierut said. "For example, two-thirds of patients with HIV and 94% of patients with diabetes receive treatment, compared with only 6% of people with alcohol use disorder."
The researchers noted that during the pandemic, alcohol sales in the U.S. increased by 34%. Consequently, they expect that as the country emerges from COVID-19 and returns to normal, the number of people with alcohol use disorder will have climbed.
"We know alcohol use and misuse have increased during the pandemic," Mintz said. "It seems there has been a shift toward heavier drinking. Plus, many doctor's offices, AA groups and other support groups were shut down for a period of time, so we would hypothesize that even the relatively small percentage of people in treatment may have declined during the past year."
INFORMATION:
Mintz, C, Hartz S, Fisher S, Ramsey A, Geng E, Grucza R, Bierut L. A cascade of care for alcohol use disorder: using 2015-2019 National Survey on Drug Use and Health data to identify gaps in past 12-month care. Alcoholism: Clinical & Experimental Research, published online May 16, 2021.
This work was supported by the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, the National Institute of Allergy and Infectious Diseases and the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH), grant numbers K12 DA041449, R21 DA044744, R21 AA025689, R01 AA029308, K24 AI134413 and Ul1 TR002345. Additional support from the Substance Abuse and Mental Health Services Administration, grant number H79TI082566.
Washington University School of Medicine's 1,500 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children's hospitals. The School of Medicine is a leader in medical research, teaching and patient care, consistently ranking among the top medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children's hospitals, the School of Medicine is linked to BJC HealthCare.
In a world that's changing fast, the Long Term Ecological Research (LTER) Network can seem almost an anachronism. Yet the patience and persistence that have generated 40 years of careful, reliable science about the Earth's changing ecosystems may prove to be just what's needed in this rapidly shifting world. We can't wait for a crystal ball -- and we don't have to. By harnessing decades of rich data, scientists are beginning to forecast future conditions and plan ways to manage, mitigate, or adapt to likely changes in ecosystems that will impact human economies, health and wellbeing.
The National Science Foundation established the LTER Network more than 40 years ago to provide an alternative to funding models that favored constant innovation over continuity. The model has proven to be extraordinarily ...
An international study has found that four out of five women in prison in Scotland have a history of head injury, mostly sustained through domestic violence. Published recently in The Lancet, researchers, including SFU psychology graduate student Hira Aslam, say the study has important implications for the female prison population more broadly and could help to inform mental health and criminal justice policy development.
"The findings are incredibly sobering," says Aslam. "While we anticipated that the incidence of head injuries among women who are involved in the criminal justice system would be high, these estimates exceeded our expectations."
Researchers also found that violent criminal behaviour was three times more likely among women who had a history of significant head injury, ...
ATS 2021, New York, NY - Air quality standards recommended by the American Thoracic Society (ATS) have the potential to prevent more illness and death than standards adopted by the U.S. Environmental Protection Agency (EPA), according to research presented at the ATS 2021 International Conference.
Laura Gladson, MS, a research scholar with the Air Quality Program at the Marron Institute of Urban Management, New York University (NYU) and colleagues from NYU and the ATS assessed differences between the potential public health protections provided by EPA air quality standards and the more stringent standards proposed by the ATS. Comparing real-world ...
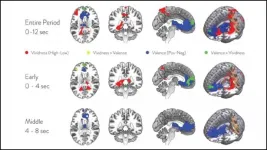
Two components of imagination -- constructing and evaluating imagined scenarios -- rely on separate subnetworks in the default mode network, according to research recently published in JNeurosci.
Even when you aren't doing anything, your brain is hard at work. The default mode network (DMN) activates during the brain's resting state and has been linked to daydreaming, planning, and imagining the future. In previous studies, scientists noticed the DMN could be divided into two subnetworks, ventral and dorsal, but their different roles were debated.
Lee et al. used fMRI to measure participants' brain activity while they imagined scenarios listed on prompts, like "Imagine you win the lottery." The scenarios ...
KINGSTON, R.I. - May 17, 2021 - An article recently published in the prestigious journal Nature Communications, written by University of Rhode Island END ...
Clinicians and surgeons are increasingly using medical devices based on artificial intelligence. These AI devices, which rely on data-driven algorithms to inform health care decisions, presently aid in diagnosing cancers, heart conditions and diseases of the eye, with many more applications on the way.
Given this surge in AI, two Stanford University faculty members are calling for efforts to ensure that this technology does not exacerbate existing heath care disparities.
In a new perspective paper, Stanford faculty discuss sex, gender and race bias in medicine and how these biases could be perpetuated by AI devices. The authors suggest several short- and long-term approaches to prevent AI-related ...
BOSTON - Peripheral artery disease (PAD), or blockages in the arteries outside of the heart, affects more than 200 million people worldwide and 12.5 million people in the United States. Patients with this circulatory disorder may develop severe leg pain or unhealing wounds that require a minimally invasive revascularization procedure to open the blood vessels to improve blood flow.
For nearly a decade, proceduralists and surgeons have depended on devices coated with a drug called paclitaxel -- which reduces the need for another procedure by up to 50 percent -- during procedures to open the arteries of the leg. However, in the wake of a 2018 study that found a potential link between ...
COLUMBUS, Ohio - Up to 38.6% of people with colon cancer who have a hereditary cancer syndrome--including 6.3% of those with Lynch syndrome--could have their conditions remain undetected with current universal tumor-screening methods, and at least 7.1% of people with colorectal cancer have an identifiable inherited genetic mutation, according to new data published by scientists at The Ohio State University Comprehensive Cancer Center - Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC - James).
Experts say their data, which was gathered from a cohort of more than 3,300 colorectal cancer patients treated at 51 hospitals across Ohio, makes a strong scientific argument for implementing multi-gene panel ...
A team of Welsh academics has developed a new method of supporting health professionals to make clinical decisions about people who may be at risk of taking their own lives.
While the UK may have one of the lowest rates of suicide in the world, it is still the biggest cause of death in men under 45, so being able to make a Structured Professional Judgement about who might attempt suicide and knowing how to intervene is vitally important.
Researchers at Swansea and Cardiff universities have put together the Risk of Suicide Protocol (RoSP) which guides a professional to look at 20 aspects of a person's life known ...
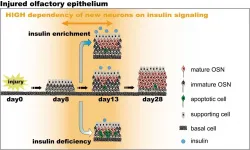
PHILADELPHIA (May 17, 2021) - Researchers have known for some time that insulin plays a vital role in regeneration and growth in some types of neurons that relay environmental sensory information to our brains, such as sight. However, they know relatively little about the role of insulin in the sense of smell. Now, investigators at the Monell Chemical Senses Center have shown that insulin plays a critical role in the maturation, after injury, of immature olfactory sensory neurons (OSNs). The team published their findings in eNeuro earlier this month.
"Our findings suggest ...