While patient survival has been extended by modern drugs that block the production or action of male hormones that fuel prostate cancer -- androgen receptor inhibitors such as enzalutamide, apalutamide, darolutamide, and abiraterone -- eventually these drugs stop working. At that point, a patient's disease is considered incurable, or what doctors call metastatic, castration-resistant prostate cancer.
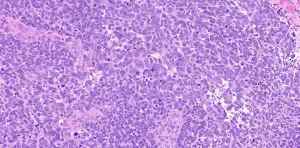
In a new study, a team of researchers led by Joshi Alumkal, M.D., who leads the prostate and genitourinary medical oncology section at the University of Michigan Rogel Cancer Center, uncovered new mechanisms underlying an important type of resistance called lineage plasticity. That's when castration-resistant prostate cancers undergo a deadly identity switch -- shifting from resembling glandular cells to neuroendocrine cells, which can behave more like small cell lung cancer.
The findings using human and mouse cell models and tissue biopsies from patients appear in Clinical Cancer Research and outline a promising path to overcoming this form of resistance: BET bromodomain inhibitors. These compounds work against bromodomain and extra-terminal (BET) proteins, which are involved in regulating gene activation.
"We know that treatment-emergent neuroendocrine prostate cancer is becoming more frequent as we use more newer and more potent androgen receptor inhibitors," Alumkal said. "Our prior work examining patients progressing on these newer androgen receptor inhibitors demonstrated that neuroendocrine prostate cancer was found in 17% of cases. By comparison, we find it in less than 1% of patients who have not undergone any form of androgen receptor inhibition. This strongly suggests that interference with androgen receptor function contributes to the increased numbers of treatment-emergent neuroendocrine prostate cancers we now see clinically."
Patients diagnosed with treatment-emergent neuroendocrine prostate cancer fare much worse than patients whose tumors remain adenocarcinomas -- glandular tumors -- surviving for only about one-third as long. Furthermore, there are very limited treatment options for patients with treatment-emergent neuroendocrine prostate cancer.
"We set out to understand how tumors shift their program to become neuroendocrine, the influence of androgen receptor inhibition on this process, and ways to block the switch to neuroendocrine prostate cancer," said Alumkal, who also co-leads of the translational and clinical research program at the U-M Rogel Cancer Center.
This line of investigation began when Alumkal was at the Knight Cancer Institute at Oregon Health & Science University and continued after his move to the U-M in 2019. The effort included a host of collaborators at other institutions, including scientists from the Dana-Farber Cancer Institute at Harvard University, the University of Washington, the Fred Hutchison Cancer Research Center, the Helen Diller Family Comprehensive Cancer Center at the University of California, San Francisco and the Memorial Sloan Kettering Cancer Center.
A promising countermeasure The major question the researchers sought to answer was whether modern prostate cancer drugs -- the new and more potent androgen receptor inhibitors -- might be so effective in shutting down the androgen receptor in some tumors that these drugs could actually promote the tumors' switch to become neuroendocrine tumors.
And the answer appears to be yes.
Through a series of experiments using laboratory cell models that were either sensitive to newer androgen receptor inhibitors or their counterpart cell models with acquired resistance, the research team found that androgen receptor inhibition was accentuating a neuroendocrine prostate cancer lineage plasticity program in the resistant cells -- an effect not achievable in the sensitive cells.
"Ultimately, we found that a critical difference that may allow the resistant cells to react differently and become more neuroendocrine is due to the way their DNA is organized and packaged," Alumkal said. "In the treatment-resistant cells, the chromatin is organized in a way that's more conducive to turning on that neuroendocrine program when the androgen receptor is blocked. It is as though the resistant cells have evolved to develop a rabbit hole through which they can change their identity and escape androgen receptor inhibition. We also found that high levels of a transcription factor called E2F1, which is involved in stemness and cell differentiation, is important for the resistant cells' ability to switch identities."
And it was this work to uncover the mechanisms giving rise to treatment-emergent neuroendocrine cancer that also pointed toward a potential solution: BET inhibitors.
Though E2F1 is not targetable directly, Alumkal's team determined that E2F1 cooperates with BET bromodomain proteins to turn on a neuroendocrine prostate cancer lineage plasticity program. Blocking BET bromodomain proteins in cell models stopped the activation of this program that drives the development of neuroendocrine prostate tumors, the research team found.
"When we treated a variety of treatment-emergent neuroendocrine prostate cancer cell lines with BET inhibitors, we greatly reduced the viability of these tumors, including tumors derived from patients," Alumkal said.
The study builds on a previous clinical trial by Alumkal and colleagues, which found a BET bromodomain inhibitor compound developed by Zenith Epigenetics, ZEN-3694, looked most active in castration-resistant prostate tumors from patients who had the lowest androgen receptor activity. Additionally, patients in the trial whose tumors didn't respond well to androgen receptor inhibitors prior to study enrollment appeared to have the most durable control with ZEN-3694, suggesting the most aggressive tumors may be particularly susceptible to BET bromodomain inhibition.
"We went back and determined that several patients from that ZEN-3694 clinical trial had treatment-emergent neuroendocrine prostate cancer," Alumkal said. "When we looked at the subset of those patients who did the best, they had the highest expression of E2F1 and the BET bromodomain protein BRD4, and the lowest expression of the androgen receptor."
"When we examined the neuroendocrine prostate cancer lineage plasticity program we identified in our cellular models, we found these same genes were highly turned on in the tumors from patients with treatment-emergent neuroendocrine prostate cancer who responded best to treatment with ZEN-3694," he added.
Ultimately, Alumkal said, the research points toward BET bromodomain inhibitors as potentially most beneficial for patients whose prostate cancer is no longer as dependent on the androgen receptor, and those with subsets of treatment-emergent neuroendocrine prostate cancer, particularly tumors in which transcription factor E2F1 may be playing an important role.
Building on the findings in the current study, a larger, international, randomized clinical trial is being planned to evaluate the effectiveness of ZEN-3694 with a particular focus on men whose tumors responded poorly to androgen receptor inhibitors -- tumors that may be less dependent on the androgen receptor.
INFORMATION:
Additional authors include Dae-Hwan Kim and Duanchen Sun, Chelsea Jenkins, Daniel J. Coleman, David Sampson, Xiangnan Guan, Joshua A. Urrutia, Jacob A. Schwartzman and Zheng Xia of the Knight Cancer Institute; William K. Storck, Katherine Welker Leng, Anbarasu Kumaraswamy, Eva S. Rodansky, Chao Zhang, Samuel K. Handelman, Jonathan Z. Sexton, Rahul Aggarwal, Armand Bankhead III, Arvind Rao and Joel A. Yates of U-M; Daniel E. Spratt of U-M and Case Western Reserve University; Himisha Beltran of the Dana-Farber Cancer Institute; Mark P. Labrecque, Colm Morrissey and Eva Corey of the University of Washington; Jared M. Lucas, Ilsa M. Coleman and Peter S. Nelson of the Fred Hutchinson Cancer Research Center; Wassim Abida of Memorial Sloan Kettering Cancer Center; Felix Y. Feng, Eric J. Small of the Helen Diller Family Comprehensive Cancer Center; and Emily M. Gesner, Sarah Attwell, Sanjay Lakhotia and Eric Campeau of Zenith Epigenetics.
Funding for the work includes the National Cancer Institute (R01CA251245, R01CA234715), the NCI Pacific Northwest Prostate Cancer SPORE (P50 CA097186); the NCI Michigan Prostate SPORE (P50 CA186786); the NCI Drug Resistance and Sensitivity Network (P50 CA186786-07S1, U54CA224079); Department of Defense Impact Award (W81XWH-16-1-0597) and Department of Defense Prostate Cancer Research Program Physician Research Award (W81XWH-17-1-0124), a Prostate Cancer Foundation Young Investigator Award, the Wayne D. Kuni and Joan E. Kuni Foundation; a U-M Rogel Scholars Award and Rogel Innovation Award/NCI (P30 CA046592); and a Sheppard Family Fund Sheppard Scholar Award. OHSU, UCSF and MSKCC received research funding from Zenith Epigenetics to conduct the industry-sponsored ZEN-3694 clinical trial.
Disclosures: Several members of the research team have received consulting income, honoraria and speakers' fees from pharmaceutical companies. OHSU, UCSF, and MSKCC have received research funding from Zenith Epigenetics to conduct the ZEN-3694 clinical trial. Co-authors Gesner, Attwell, Lakhotia and Campeau are employees of Zenith Epigenetics, which makes the study compound ZEN-3694.
Paper cited: "BET Bromodomain Inhibition Blocks an AR-Repressed, E2F1-Activated Treatment-Emergent Neuroendocrine Prostate Cancer Lineage Plasticity Program," Clinical Cancer Research. DOI: 10.1158/1078-0432.CCR-20-4968