Eczema is an inflammatory skin condition that often affects infants as young as one to two months. Among the various types of eczema seen in infants, early-onset atopic dermatitis (AD), characterized by psychological stress and sleep disorders, is particularly concerning. Studies have, in fact, identified that if left untreated, AD can increase the risk of allergic diseases such as food allergies and asthma—a progression also known as the “atopic march”. Early diagnosis and intervention of early-onset AD is needed to ensure the infant’s psychological and physical health.
However, it can be difficult to make a diagnosis of AD in infants as young as one or two months. Besides parents’ reluctance to seek medical advice and the infant’s inability to express their symptoms, the diagnosis of AD may be influenced by the doctor’s subjectivity and experience. Moreover, the use of accurate yet invasive diagnostic procedures for AD, such as skin biopsies, is difficult in infants. There is, thus, a need for new methods of diagnosing AD that are objective and non-invasive.
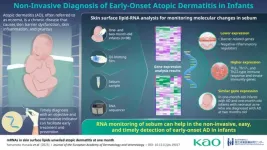
In an earlier study led by Project Leader Takayoshi Inoue from the Biological Science Research division at Kao Corporation, some of these researchers had identified that sebum contains measurable levels of human mRNA molecules. They hypothesized that analyzing the genetic expression of such RNA-containing sebum samples could reveal the molecular features of AD, and its underlying pathogenesis. Based on this discovery, the researchers developed a novel analytical method called “RNA monitoring” that enables human skin transcriptome analysis of the mRNA in sebum (skin surface lipids) collected from the skin using a simple oil-blotting film.
In this study published in the Journal of the European Academy of Dermatology and Venereology on March 10, 2023, the researchers verified the usefulness of this novel RNA monitoring method. This study was conducted in collaboration with Kiwako Yamamoto-Hanada and Yukihiro Ohya of the National Center for Allergy Research at the National Center for Child Health and Development, Japan. The main objective of this study was to determine if sebum RNA could provide reliable biomarkers for the detection of early-onset AD in infants.
The study population comprised a prospective cohort of 98 one- and two-month-old infants. In some of these infants, a diagnosis of AD was made according to the United Kingdom Working Party’s criteria. The researchers first collected sebum from the facial skin of all participating infants using a single oil-blotting film, in a non-invasive and easy procedure. Next, mRNA in skin surface lipids (SSLs) were extracted for performing transcriptome analysis, and lastly, subjected to data analysis for identifying their underlying molecular features of early-onset AD in infants.
The analysis revealed several genes with different expression between infants with and without AD. Specifically, the researchers observed that one-month-old infants with AD had lower expression of genes related to lipid metabolism and synthesis, tight junctions, antimicrobial peptides, and keratinization, and higher expression of genes related to Th2-, Th17- and Th22-type immune responses. These molecular changes in barrier function and inflammatory markers characterizing AD were not reported in earlier literature, especially in one-month old infants, largely owing to the invasiveness of common diagnostic procedures.
Most importantly, the team observed that via changes in the levels of these markers, sebum RNA could be used to detect the onset of AD well in advance. Explains Dr. Yamamoto-Hanada, Chief of the Allergy Center, “Our results confirm that the RNA monitoring method is useful for the early detection of AD in infants and may also be used for their treatment monitoring in the future.”
Hopefully, the availability of this simple, objective, and non-invasive diagnostic option for AD will encourage parents of infants with AD to opt for early consultation and therapeutical intervention of the condition. “Infants often have multiple eczemas and experience repeated exacerbations and remissions. With our method, the timely treatment of early-onset AD can be realized, enabling an improvement in the quality of life for infants with AD and their families,” says Dr. Yamamoto-Hanada.
We can only hope that the results of this research lessen the suffering of infants and their families and bring our society one step closer to being allergy-free!
About Kao
Kao creates high-value-added products and services that provide care and enrichment for the life of all people and the planet. Through its portfolio of over 20 leading brands such as Attack, Bioré, Goldwell, Jergens, John Frieda, Kanebo, Laurier, Merries, and Molton Brown, Kao is part of the everyday lives of people in Asia, Oceania, North America, and Europe. Combined with its chemical business, which contributes to a wide range of industries, Kao generates about 1,550 billion yen in annual sales. Kao employs about 35,400 people worldwide and has 136 years of history in innovation. Please visit the Kao Group website for updated information.
About the Allergy Center at the National Center for Child Health and Development
The Allergy Center at the National Center for Child Health and Development was established in June 2018. As the national core hospital for allergic diseases, the Allergy Center provides high quality clinical management of allergic disorders and promotes clinical research in allergology, operating through the Division of General Allergy, Division of Dermatological Allergy, and the Division of Gastrointestinal Allergy. It provides personalized treatment based on clinical guidelines and highly reliable medical evidence on areas such as food allergies, atopic dermatitis, bronchial asthma and associated diseases, and allergic rhinitis, to name a few.
END