Francis Crick Institute press release
Under strict embargo: 14:00 BST / 09:00hrs ET Wednesday 4 October 2023
Peer reviewed
Observational and experimental studies
People and cells
A research team at the Francis Crick Institute and Great Ormond Street Hospital (GOSH)/UCL Great Ormond Street Institute of Child Health have identified new potential treatments for children with rare genetic conditions of blood vessels, which cause severe, lifelong, and disabling symptoms like seizures and impaired development.
Through two papers published today in the Journal of Investigative Dermatology, the researchers showed that problems with calcium underlie these diseases. Stabilising calcium levels in the brain could therefore be a target for new treatments, to protect the brain from damage over time.
‘Mosaic mutations’ – genetic changes which appear in some cells in the body but not all – in two genes, GNAQ or GNA11, cause a spectrum of conditions including Sturge-Weber syndrome and Phakomatosis Pigmentovascularis with Dermal Melanocytosis (PPV-DM).
These mutations affect the skin, brain and eyes, leading to seizures, impaired development, severe headaches, blindness, and birthmarks on the face. Although children are born with the conditions, the brain symptoms get progressively worse over the first years of life. People can have a normal life expectancy, but many will experience serious and disabling symptoms throughout their lives.
Calcium deposits were known to build up in the brain in these conditions. They form parallel lines in the blood vessels, called ‘tramlining’, which can be seen on X-rays. Doctors believed the calcium deposits were non-specific signs of brain damage, but this research challenges this view.
The researchers examined 42 children with either Sturge-Weber syndrome or PPV-DM at GOSH. They found that 74% of the children had at least one abnormal measurement of calcium in the blood, and their calcium brain deposits were getting worse over time. Surgery for epilepsy in five patients revealed calcium deposits inside brain cells and tiny blood vessels in the brain.
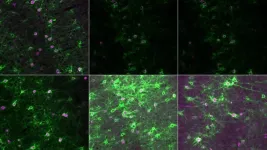
The researchers then studied patient samples in the lab at the Crick, as well as blood vessel cells engineered with and without the mutations. This approach clarified exactly what was happening in the cells with the mutations, identifying that too much calcium was being released inside cells all the time. This effect was so strong that it led to the cells pulling in even more calcium from outside to keep up with the demand, through transporters on the cell called CRAC channels. The team concluded that this chronic calcium imbalance could underpin the clinical symptoms.
To try and treat the cells in the lab, the team tested a new genetic therapy to silence the overactive gene and a drug to block the CRAC channels. Both treatments were able to improve the calcium problems, but the genetic therapy was the most effective.
The researchers hope early intervention with the genetic therapy or with a drug that targets the calcium pathway will prevent the calcium deposits building up in the brain cells and contributing to seizures.
Veronica Kinsler, Principal Group Leader of the Mosaicism and Precision Medicine Laboratory at the Crick, Professor of Paediatric Dermatology and Dermatogenetics at GOSH/UCL, and NIHR Research Professor, said, “It’s always such a shock for the family if a child is born with Sturge-Weber syndrome or PPV-DM as these rare conditions aren’t picked up on ultrasound screening, and they don’t run in families so they can happen to anyone.
“By using the power of science to work out exactly what is going on in this disease, we have finally been able to understand the calcium deposits in the brain that doctors have seen in the clinic for years. With the support of all the patients who have participated and the funders, we’ve been able to use this new insight to design potential treatments. We think there’s a window of opportunity where we can now try to make a difference for children diagnosed with these severe diseases.”
The researchers were funded by the National Institute for Health and Care Research (NIHR), and the research was supported by the US Sturge-Weber Foundation, Associazione Sindrome di Sturge Weber Italia, and by GOSH Charity via the Livingstone Skin Research Centre.
Antonella Perini, president of the Associazione Sindrome di Sturge Weber Italia, which funded the study, said: “For our organization, which gathers together patients affected by a rare disease and their families, scientific research stands as our paramount ally and hope. Thus, a research project yielding such significant and potentially impactful results fills us with satisfaction and a sense of confidence in the future.”
-ENDS-
For further information, contact: press@crick.ac.uk or +44 (0)20 3796 5252
Notes to Editors
Reference: Zecchin, D. et al. (2023). GNAQ/GNA11 mosaicism causes aberrant calcium signalling susceptible to targeted therapeutics. Journal of Investigative Dermatology. 10.1016/j.jid.2023.08.028.
Knöpfel, N. et al. (2023). GNAQ/GNA11 mosaicism is associated with abnormal serum calcium indices and microvascular neurocalcification. Journal of Investigative Dermatology. 10.1016/j.jid.2023.09.008.
About the Francis Crick Institute
The Francis Crick Institute is a biomedical discovery institute dedicated to understanding the fundamental biology underlying health and disease. Its work is helping to understand why disease develops and to translate discoveries into new ways to prevent, diagnose and treat illnesses such as cancer, heart disease, stroke, infections, and neurodegenerative diseases.
An independent organisation, its founding partners are the Medical Research Council (MRC), Cancer Research UK, Wellcome, UCL (University College London), Imperial College London and King’s College London.
The Crick was formed in 2015, and in 2016 it moved into a brand new state-of-the-art building in central London which brings together 1500 scientists and support staff working collaboratively across disciplines, making it the biggest biomedical research facility under a single roof in Europe.
http://crick.ac.uk/
About Great Ormond Street Hospital for Children NHS Foundation Trust
Great Ormond Street Hospital is one of the world’s leading children’s hospitals with the broadest range of dedicated, children’s healthcare specialists under one roof in the UK. The hospital’s pioneering research and treatment gives hope to children from across the UK with the rarest, most complex and often life-threatening conditions. Our patients and families are central to everything we do – from the moment they come through the door and for as long as they need us.
Media contact for Great Ormond Street Hospital for Children: Madeleine Smith; media@gosh.nhs.uk
About NIHR
The mission of the National Institute for Health and Care Research (NIHR) is to improve the health and wealth of the nation through research. We do this by:
Funding high quality, timely research that benefits the NHS, public health and social care;
Investing in world-class expertise, facilities and a skilled delivery workforce to translate discoveries into improved treatments and services;
Partnering with patients, service users, carers and communities, improving the relevance, quality and impact of our research;
Attracting, training and supporting the best researchers to tackle complex health and social care challenges;
Collaborating with other public funders, charities and industry to help shape a cohesive and globally competitive research system;
Funding applied global health research and training to meet the needs of the poorest people in low and middle income countries.
NIHR is funded by the Department of Health and Social Care. Its work in low and middle income countries is principally funded through UK Aid from the UK government.
END