Revolutionary chronic wound treatment could help millions
A team of international scientists has developed an effective treatment for preventing infection in chronic wounds that does not involve antibiotics
The treatment involves the plasma (electrical gas) activation of hydrogel dressings to produce a unique mix of different chemical oxidants that applied to the wound are effective in decontaminating and aiding healing in chronic wounds
The new method is a significant advance that could revolutionise the treatment of diabetic foot ulcers and internal wounds
More than 540 million people are living with diabetes worldwide, of which 30 per cent will develop a foot ulcer during their lifetime
An effective treatment for chronic wounds that does not involve antibiotics, but an ionised gas to activate a wound dressing, has been developed by a team of international scientists.
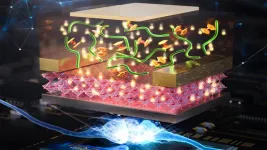
The treatment involves the plasma activation of hydrogel dressings (that are commonly used in wound dressings) with a unique mix of different chemical oxidants that are effective in decontaminating and aid healing in chronic wounds.
Researchers from the University of Sheffield and University of South Australia, who led the study, believe the new method is a significant advance in tackling antibiotic resistance pathogens and has the potential to change the treatment of diabetic foot ulcers and internal wounds.
Professor Rob Short, Professor of Chemistry at the University of Sheffield who co-authored the study, said: “More than 540 million people are living with diabetes worldwide, of which 30 per cent will develop a foot ulcer during their lifetime. This is a neglected global pandemic which is set to increase further in the coming years due to a rise in obesity and lack of exercise.
“In England alone between 60,000 and 75,000 people are being treated for diabetic foot ulcers per week. Infection is one of the major risks. Increasingly, many infections do not respond to normal antibiotic treatment due to resistant bacteria which results in 7,000 amputations per year.
“There is an urgent need for innovation in wound management and treatment and it is a real privilege to be part of the international team who have been working on this alternative treatment for over 10 years.”
The cost of managing chronic wounds such as diabetic foot ulcers already exceeds $17 billion US dollars annually.
The benefits of cold plasma ionised gas have already been proven in clinical trials, showing it controls not only infection but also stimulates healing. This is due to the potent chemical cocktail of oxidants, namely reactive oxygen and nitrogen species (RONS) it produces when it mixes and activates the oxygen and nitrogen molecules in the ambient air.
Dr Endre Szili, from the University of South Australia who led the study, published this week in the journal Advanced Functional Materials, said: “Antibiotics and silver dressings are commonly used to treat chronic wounds, but both have drawbacks.
“Growing resistance to antibiotics is a global challenge and there are also major concerns over silver-induced toxicity. In Europe, silver dressings are being phased out for this reason.”
The international team of scientists have shown that plasma activating hydrogel dressings with RONS makes the gel far more powerful, killing common bacteria.
Although diabetic foot ulcers were the focus of this study, the technology could be applied to all chronic wounds and internal infections.
“Despite recent encouraging results in the use of plasma activated hydrogel therapy (PAHT), we faced the challenge of loading hydrogels with sufficient concentrations of RONS required for clinical use. We have overcome this hurdle by employing a new electrochemical method that enhances the hydrogel activation,” said Dr Szili.
As well as killing common bacteria (E. coli and P. aeruginosa) that cause wounds to become infected, the researchers say that the plasma activated hydrogels might also help trigger the body’s immune system, which can help fight infections.
“Chronic wound infections are a silent pandemic threatening to become a global healthcare crisis,” added Dr Szili.
“It is imperative that we find alternative treatments to antibiotics and silver dressings because when these treatments don’t work, amputations often occur.”
“A major advantage of our PAHT technology is that it can be used for treating all wounds. It is an environmentally safe treatment that uses the natural components in air and water to make its active ingredients, which degrade to non-toxic and biocompatible components.”
“The active ingredients could be delivered over a lengthy period, improving treatment, with a better chance of penetrating a tumour.
“Plasma has massive potential in the medical world, and this is just the tip of the iceberg,” Dr Szili says.
The next step will involve clinical trials to optimise the electrochemical technology for treatment in human patients.
A video explaining the treatment is available at: https://youtu.be/TdwfA9narMg
Contact
For further information please contact: Amy Huxtable, Senior Media Relations Officer, University of Sheffield, a.l.huxtable@sheffield.ac.uk, 07568116781
Additional information
“Electrochemically Enhanced Antimicrobial Action of Plasma Activated Poly(vinyl alcohol) Hydrogel Dressings” is published in the journal Advanced Functional Materials.
It is authored by scientists from the University of Sheffield, UK; University of South Australia; Osaka City University, Japan; the University of Alabama, US; and the University of Adelaide.
END