Repairing patients’ dura more durably
Highly adhesive and mechanically strong Dural Tough Adhesive addresses multiple limitations in the repair of the dural membrane lining the brain and spinal cord after trauma and surgeries.
By Benjamin Boettner
(BOSTON) — The dural membrane (dura) is the outermost of three meningeal layers that line the central nervous system (CNS), which includes the brain and spinal cord. Together, the meninges function as a shock-absorber to protect the CNS against trauma, circulate nutrients throughout the CNS, as well as remove waste. The dura also is a critical biological barrier that contains cerebrospinal fluid (CSF) surrounding all CNS tissues. Consequently, spontaneous injury, trauma, or necessary surgical procedures may cause CSF to leak, which can threaten patients’ lives, neurological functions, and recovery.
“As neurosurgeons, we routinely open the dura to access the brain or spinal cord, but achieving a watertight seal of the dura at the conclusion of these procedures can be challenging in particular circumstances,” said Kyle Wu, M.D., a neurosurgeon and the co-first and co-corresponding author of a new study presenting an innovative dural repair solution. “Our current options are limited, consisting of suture repair or grafting, which can be difficult to perform if there is no viable tissue, with large defects, or during minimally invasive surgeries Currently available surgical sealants don’t adhere well to wet tissue, are too brittle, and lack the requisite toughness to reliably prevent CSF leakage.” Wu now is an Assistant Professor at The Ohio State University Wexner Medical Center, and at the start of the study was a neurosurgery resident at the Brigham and Women’s Hospital in Boston and Surgical Innovation Fellow at Boston Children’s Hospital.
A new solution to re-sealing the dura has now been developed by a collaborative team of bioengineers at the Wyss Institute for Biologically Inspired Engineering at Harvard University and the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS), and neurosurgeons at the Brigham and Women’s Hospital, and Ohio State University’s Wexner Medical Center and James Cancer Hospital, which uses a multi-functional biomaterial that addresses key limitations of current repair methods and has potential to supplant them. The researchers, led by Wyss Institute Founding Core Faculty member and SEAS Robert P. Pinkas Family Professor of Bioengineering David Mooney, Ph.D., demonstrated that their “Dural Tough Adhesive” (DTA) performed better than currently used surgical sealants in tests using in vivo animal models and human-derived tissues ex vivo. The findings are published in Science Translational Medicine.
Taking inspiration from nature
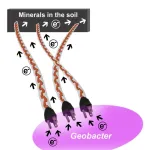
DTAs are an interesting example of “bioinspired engineering.” Almost a decade ago, Mooney’s group, which had already gathered expertise in the design of hydrogels with distinct mechanical features, was looking for examples in nature that could help find new solutions for sealing and regenerating injured tissues in the body. “Material approaches to tissue regeneration at the time mainly focused on creating strong ‘adhesion’ to various body surfaces, but not so much on strong internal ‘cohesion,’ or toughness in the face of tissue mechanical forces,” said co-first author Benjamin Freedman, Ph.D., a former Wyss Research Associate on Mooney’s team. “In addition, they remained relatively ineffective in sticking to wet tissue surfaces covered by different body fluids.” Their search led the group to the Dusky Arion slug (Arion subfuscus), which secretes a special kind of mucus that it uses to rapidly glue itself in place to prevent predators from prying it off various surfaces.
In part by mimicking properties of the slug’s mucus, the team developed a hydrogel consisting of two intermixed polymer networks: a network of permanently cross-linked acrylamide molecules that creates a highly elastic gel, and a network of reversibly cross-linked alginate molecules that can redistribute the energy produced by mechanical forces in underlying tissues. Paired with a highly adhesive layer that uses chitosan, a fibrous, sugar-based substance derived from the outer skeletons of shellfish, the composite Tough Adhesive (TA) hydrogel can bond to a variety of liquid-covered surfaces by forming multiple types of chemical interactions with them that cooperatively create a tight seal. “The Mooney group had previously advanced TA approaches for the repair of multiple tissues, including wounded tissue surfaces, tendons, neural tube defects of babies in the womb, and others. When Dr. Wu reached out to us, we embraced dural membrane leakage as a new clinical opportunity for TAs,” said Freedman, who spearheaded several TA applications on Mooney’s team.
Improved protection for the brain and spinal cord
The team demonstrated that DTA, whose composition follows the same TA basic formulation, has repair-relevant features that are superior to those of existing surgical sealants. In ex vivo studies, they showed that DTA adheres significantly stronger to pigs’ dural membranes and can withstand higher pressures before failing, compared to a commercial sealant. Superior mechanical strength is an important feature of DTAs, since increased intracranial pressure may be encountered in conditions such as brain tumors, stroke, trauma, idiopathic intracranial hypertension, and hydrocephalus.
In vivo, when placed directly onto the dura of rats, DTA maintained its structure and was fully biocompatible for at least four weeks, causing only minimal irritation, which was comparable to commercial sealants.
The team showed that DTAs could deliver these same benefits when tested using human cadaveric tissue. “In light of the persistent trend toward minimally invasive neurosurgeries for patients’ benefit, an ideal dural sealant must not only be a better alternative to suture repair, but also be easier to handle and deploy in tight spaces – current repair methods are not good at both,” said Wu. “In fact, we were able to introduce DTA through the nasal cavity of a human cadaveric cephalus and place it accurately onto a leaking area of the skull base where it withstood artificially generated intracranial pressures that were well beyond the range of even pathological pressures.”
Translating some of their key in vitro findings to an in vivo situation, Mooney, Freedman, Wu and their colleagues focused on a tear in the dural sac enveloping the spinal cord of pigs. The pig spine strongly resembles that of humans. Dural tears are a feared complication during spine surgery. The team successfully sealed incisions in the dura with a DTA patch, or alternatively with the commercial spine sealant DuraSeal as a comparison. Then, they increased the fluid pressure within the spinal cord, applying a physiologic maneuver that many neurosurgeons perform to test the integrity of dural repair at the end of surgeries. While DTA-repaired incisions never experienced any leakage with these mild increases in fluid pressure, DuraSeal-repaired incisions started leaking in 40% of the cases. In the model, DTA also readily resisted leakage even when exposed to fluid pressures much higher than those experienced in the body.
“We are excited to have opened a new perspective for neurosurgeons with this study that, in the future, could facilitate a variety of surgical interventions and lower the risk for patients who need to undergo them. This study also underscores how unique and well-understood advances in the design of biomaterials, like the ones we made in our Tough Adhesive platform, have the potential to impact multiple very diverse areas of regenerative medicine,” said senior author Mooney.
Other authors on the study are Wenya Linda Bi, M.D., Ph.D., Associate Professor of Neurosurgery at Harvard Medical School and Brigham and Women’s Hospital, as well as Phoebe Kwon, Matthew Torre, and Daniel Kent. The work was supported by the Wyss Institute at Harvard University, and National Institutes of Health (under grant# K99/R00AG065495).
PRESS CONTACTS
Wyss Institute for Biologically Inspired Engineering at Harvard University
Benjamin Boettner, benjamin.boettner@wyss.harvard.edu, +1 617-432-8232
###
The Wyss Institute for Biologically Inspired Engineering at Harvard University (www.wyss.harvard.edu) is a research and development engine for disruptive innovation powered by biologically-inspired engineering with visionary people at its heart. Our mission is to transform healthcare and the environment by developing ground-breaking technologies that emulate the way Nature builds and accelerate their translation into commercial products through formation of startups and corporate partnerships to bring about positive near-term impact in the world. We accomplish this by breaking down the traditional silos of academia and barriers with industry, enabling our world-leading faculty to collaborate creatively across our focus areas of diagnostics, therapeutics, medtech, and sustainability. Our consortium partners encompass the leading academic institutions and hospitals in the Boston area and throughout the world, including Harvard’s Schools of Medicine, Engineering, Arts & Sciences and Design, Beth Israel Deaconess Medical Center, Brigham and Women’s Hospital, Boston Children’s Hospital, Dana–Farber Cancer Institute, Massachusetts General Hospital, the University of Massachusetts Medical School, Spaulding Rehabilitation Hospital, Boston University, Tufts University, Charité – Universitätsmedizin Berlin, University of Zürich, and Massachusetts Institute of Technology.
The Harvard John A. Paulson School of Engineering and Applied Sciences (http://seas.harvard.edu) serves as the connector and integrator of Harvard’s teaching and research efforts in engineering, applied sciences, and technology. Through collaboration with researchers from all parts of Harvard, other universities, and corporate and foundational partners, we bring discovery and innovation directly to bear on improving human life and society.
Brigham and Women’s Hospital (https://www.brighamandwomens.org) is a founding member of Mass General Brigham and a teaching affiliate of Harvard Medical School. With nearly 1,000 inpatient beds, approximately 50,000 inpatient stays, and over 2.6 million outpatient encounters annually, clinicians across the Brigham provide compassionate, high-quality care in virtually every medical and surgical specialty to patients locally, regionally, nationally and around the world. An international leader in basic, clinical, and translational research, Brigham and Women’s Hospital has nearly 5,000 scientists, including physician-investigators, renowned biomedical researchers and faculty supported by nearly $750 million in funding. The Brigham’s medical preeminence and service to the community dates to 1832, with the opening of the Boston Lying In, one of the nation's first maternity hospitals designed to care for women unable to afford in-home medical care. Its merger with the Free Hospital for Women resulted in the Boston Hospital for Women in 1966. In 1980, the Boston Hospital for Women, the Peter Bent Brigham Hospital and the Robert Breck Brigham Hospital officially merged to become Brigham and Women’s Hospital. With nearly 21,000 employees across the Brigham family – including the Brigham and Women’s Physicians Organization and Brigham and Women’s Faulkner Hospital – that rich history is the foundation for our commitment to providing superb care for some of the most complex cases, pursuing breakthroughs in biomedical research, training the next generation of health care providers, and serving the local and global community.
END