In particular, the technique identified a cellular neighborhood that correlated with a positive response to immunotherapy, which may help physicians make treatment decisions.
“These cancers are challenging,” said Everett Moding, MD, PhD, an assistant professor of radiation oncology. “Up to half of patients diagnosed with a primary tumor will develop distant metastases, but we don’t have a good way to predict who. Chemotherapy typically doesn’t work well for these patients, and most don’t respond to immunotherapy. Identifying patterns in whether and how different cell types interact with one another and correlating them with outcome is critical to understanding more about the complexity of this disease and improving outcomes.”
Moding is the senior author of the study, which was published this month in Nature Cancer. The lead authors are graduate student Ajay Subramanian, former research assistant Neda Nemat-Gorgani, and hematology and medical oncology fellow Timothy Ellis-Caleo, MD.
A rare cancer
Soft tissue sarcomas are rare — only about 13,500 cases are diagnosed in the United States each year. They arise from what are called mesenchymal cells, which form the connective tissues in the body, rather than from epithelial cells, which line internal organs and skin and from which most other cancers, called carcinomas, arise. This distinction suggests that the underlying biology of sarcomas may differ from that of more common cancers.
There are many subtypes of the cancer, which develops in soft tissues such as fat, blood vessels, fibrous tissues or muscle. About one-half of all soft tissue sarcomas start in an arm or leg; about 40% originate in the abdomen. Surgery can cure many people if the cancer is localized, but the median survival is less than two years for people with metastatic disease.
Researchers are realizing that studying the interplay between different cell types, known as the tumor microenvironment, provides critical insight into the biology of tumors. But the rarity of soft tissue sarcomas, the many subtypes of the disease, and the fact that many tissue samples have been preserved and embedded in paraffin, have made such an analysis challenging. Techniques that include flow cytometry, which separates individual cells into batches much like a coin sorter, or single-cell RNA sequencing, which provides a readout of the RNA messages — and therefore the types of proteins — an individual cell is making, aren’t possible without fresh samples of similar tumors from many patients.
The researchers involved in the study turned instead to a machine-learning technique called EcoTyper, developed in 2021 in the Stanford Medicine laboratory of Aaron Newman, PhD, assistantd professor of biomedical data science; and another called CIBERSORTx, developed in 2019 by Newman and Ash Alizadeh, MD, PhD, the Moghadam Family Professor, professor of medicine and the leader of the Cancer Genomics Program at the Stanford Cancer Institute.
Like an eerily accurate fortune teller, CIBERSORTx predicts the various cell types in a bulk tissue sample based on the relative abundance and patterns of RNA messages in the sample. EcoTyper builds on this prediction to determine what the cell types are up to (a condition called cell state) and which other cells they are interacting with. The information allows researchers to build a picture of complex cellular neighborhoods within tumor tissue that hint at how the tumor is (or isn’t) thriving.
New insights
“Machine learning overcomes many of the problems that had been holding back our understanding of soft tissue sarcomas,” Moding said. “We don’t need fresh tissue, and we can use computational approaches to learn what cell types a tumor contains and which of them tend to interact with each other. We can use publicly available data to generate new insights.”
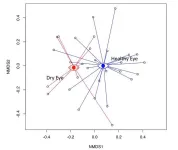
Using CIBERSORTx and Ecotyper, the researchers identified 23 distinct cells states in nine cell types in soft tissue sarcomas isolated from several hundred patients. EcoTyper used this information to pinpoint three multicellular communities, called ecotypes. These ecotypes, the researchers found, correlated with the patients’ clinical outcomes.
In general, patients whose tumors contained cellular communities with a high proportion of cancer-fighting immune cells fared significantly better than patients with tumors that had few immune cells and elevated levels of proteins involved in a signaling pathway called Hedgehog.
People whose tumors contained an intermediate number of immune cells and displayed elevated levels of RNA messages involved in cancer-associated signaling pathways called MYC and MTORC1 had the worst outcomes, but they were also much more likely to respond to immunotherapy than either of the previous two groups.
“This is kind of unusual,” Moding said. “We found that soft tissue sarcoma tumors that respond well to immunotherapy have an intermediate level of infiltration by immune cells, while previous studies of other types of cancers have found that tumors with lots of immune cells — a condition known as ‘immune hot’ — are the most likely to respond to immunotherapy.”
The researchers studied stored samples of soft tissue sarcomas and compared their findings with the clinical outcomes of the patients from whom they were obtained. Moding and his colleagues now hope to conduct a similar prospective study with newly diagnosed patients to investigate whether the new ecotypes can be successfully used to guide patient care.
“Currently immunotherapy is used mostly as a second-line therapy for these patients,” Moding said. “But we’re starting to understand the complexity of the interactions between cancer cells and immune cells, and we hope to leverage these to improve outcomes and develop new therapies.”
Researchers from Memorial Sloan Kettering Cancer Center and the Weill Cornell Medical Center contributed to the work.
The study was funded by the National Institutes of Health (grants S10OD025212 and 1S10ODO21763), the Department of Defense, the National Cancer Institute, the Stanford Cancer Institute, My Blue Dots, and the Tad and Diane Taube Family Foundation.
# # #
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu.
END