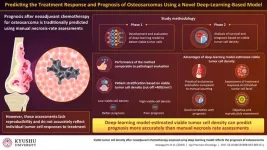
Fukuoka, Japan - Researchers at Kyushu University have developed and validated a machine-learning model that can accurately evaluate the density of surviving tumor cells after treatment in pathological images of osteosarcoma—the most prevalent malignant bone tumor. The model can assess how individual tumor cells respond to treatment and can predict overall patient prognosis more reliably than conventional methods.
Surgery and chemotherapy have significantly improved the outcomes of patients with localized osteosarcoma. However, patients with advanced metastatic disease (the stage where cancerous cells have spread to distant tissues) have a low survival rate. After a standard treatment of surgery and chemotherapy, assessing the prognosis of patients is essential for determining their subsequent individual treatment plans. However, predicting patient outcomes has many challenges. Currently, prognosis relies on necrosis rate assessment, which involves pathologists evaluating the proportion of dead tissue within a tumor. Unfortunately, these methods are limited by variability between pathologists’ assessments and may not accurately predict treatment response.
Recognizing the need for faster and more accurate prognoses, co-first authors Dr. Kengo Kawaguchi and Dr. Kazuki Miyama, from the Department of Orthopedic Surgery, Graduate School of Medical Sciences, Kyushu University, Japan, and Dr. Makoto Endo, a lecturer of Orthopedic Surgery at Kyushu University Hospital, along with collaborators, turned to artificial intelligence (AI) for a more nuanced evaluation. The multidisciplinary team headed by Dr. Endo included Kyushu University’s Professor Ryoma Bise, Professor Yoshinao Oda, and Professor Yasuharu Nakashima. Explaining the rationale behind their research, which was published on 22 January, 2024, in njp Precision Oncology, Dr. Endo says, “In the traditional method, the necrosis rate is calculated as a necrotic area rather than individual cell counts, which is not sufficiently reproducible between assessors and does not adequately reflect the effects of anticancer drugs. We therefore considered using AI to improve the estimation.”
In phase 1 of the study, the team trained a type of AI, called a deep-learning model, to detect surviving tumor cells and validated its detection performance using patient data. The AI model showed proficiency in detecting viable tumor cells in pathological images, aligning with expert pathologists' capabilities. In phase 2, the researchers analyzed two key measures: disease-specific survival, which tracks the duration after diagnosis or treatment without death directly caused by the disease, and metastasis-free survival, which monitors the time post-treatment without cancer cells spreading to distant body parts. They also explored the correlation between AI-estimated viable tumor cell density and prognosis. Notably, the AI model demonstrated comparable detection performance and precision to that of the pathologist, with good reproducibility.
Next, the researchers sorted the patients into groups based on whether the viable tumor cell density was above or below 400/mm2. The survival analysis revealed that the high-density group showed a worse prognosis, while the low-density group showed a better prognosis for disease-specific survival and metastasis-free survival. Necrosis rate, on the other hand, was not associated with disease-specific survival or metastasis-free survival. Furthermore, analysis of individual cases revealed that AI-estimated viable tumor cell density was a more reliable predictor of prognosis than necrosis rate.
Overall, these findings suggest that the AI-based measurement of viable tumor cells reflects the inherent malignancy (ability of the cancer to spread) and individual tumor cell response of osteosarcomas. Incorporating AI in the analysis of pathological images improves detection accuracy, reduces inter-assessor variability, and enables timely assessment. Moreover, the estimation of viable tumor cells, which reflects their ability to keep multiplying following chemotherapy, is a more reliable predictor of treatment response than cell death. Large-scale validation of the AI model developed in this study can aid its wider application in real-life clinical settings.
“This new approach has the potential to enhance the accuracy of prognoses for osteosarcoma patients treated with chemotherapy. In the future, we intend to actively apply AI to rare diseases such as osteosarcoma, which have seen limited advancements in epidemiology, pathogenesis, and etiology. Despite the passage of decades, particularly in treatment strategies, substantial progress remains elusive. By putting AI to the problem, this might finally change,” concludes a hopeful Dr. Endo.
###
For more information about this research, see " Viable tumor cell density after neoadjuvant chemotherapy assessed using deep learning model reflects the prognosis of osteosarcoma" Kengo Kawaguchi, Kazuki Miyama, Makoto Endo, Ryoma Bise, Kenichi Kohashi, Takeshi Hirose, Akira Nabeshima, Toshifumi Fujiwara, Yoshihiro Matsumoto, Yoshinao Oda & Yasuharu Nakashima, npj Precision Oncology, https://doi.org/10.1038/s41698-024-00515-y
About Kyushu University
Founded in 1911, Kyushu University is one of Japan's leading research-oriented institutes of higher education, consistently ranking as one of the top ten Japanese universities in the Times Higher Education World University Rankings and the QS World Rankings. The university is one of the seven national universities in Japan, located in Fukuoka, on the island of Kyushu—the most southwestern of Japan’s four main islands with a population and land size slightly larger than Belgium. Kyushu U’s multiple campuses—home to around 19,000 students and 8000 faculty and staff—are located around Fukuoka City, a coastal metropolis that is frequently ranked among the world's most livable cities and historically known as Japan's gateway to Asia. Through its VISION 2030, Kyushu U will “drive social change with integrative knowledge.” By fusing the spectrum of knowledge, from the humanities and arts to engineering and medical sciences, Kyushu U will strengthen its research in the key areas of decarbonization, medicine and health, and environment and food, to tackle society’s most pressing issues.
END