(Press-News.org) Withdrawing aspirin one month after percutaneous coronary intervention (PCI) in high-risk heart patients and keeping them on ticagrelor alone safely improves outcomes and reduces major bleeding by more than half when compared to patients taking aspirin and ticagrelor combined (also known as dual antiplatelet therapy or DAPT), which is the current standard of care.
These are the results from the ULTIMATE-DAPT study announced during a late-breaking trial presentation at the American College of Cardiology Scientific Sessions on Sunday, April 7, and published in The Lancet.
This is the first and only trial to test high-risk patients with recent or threatened heart attack (acute coronary artery syndromes, or ACS) taking ticagrelor with a placebo starting one month after PCI, and compare them with ACS patients taking ticagrelor with aspirin over the same period. The significant findings could change the current guidelines for standard of care worldwide.
“Our study has demonstrated that withdrawing aspirin in patients with recent ACS one month after PCI is beneficial by reducing major and minor bleeding through one year by more than 50 percent. Moreover, there was no increase in adverse ischemic events, meaning continuing aspirin was causing harm without providing any benefit,” says Gregg W. Stone, MD, the study co-chair of ULTIMATE-DAPT, who presented the trial results.
“It is my belief that it’s time to change the guidelines and standard clinical practice such that we no longer treat most ACS patients with dual antiplatelet therapy beyond one month after a successful PCI procedure. Treating these high-risk patients with a single potent platelet inhibitor such as ticagrelor will improve prognosis,” adds Dr. Stone, who is Director of Academic Affairs for the Mount Sinai Health System and Professor of Medicine (Cardiology), and Population Health Science and Policy, at the Icahn School of Medicine at Mount Sinai.
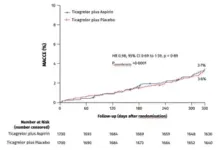
The study analyzed 3,400 patients with ACS at 58 centers in four countries between August 2019 and October 2022. All of the patients had undergone PCI, a non-surgical procedure in which interventional cardiologists use a catheter to place stents in the blocked coronary arteries to restore blood flow. The patients were stable one month after PCI and were on ticagrelor and aspirin. Researchers randomized the patients after one month, withdrawing aspirin in 1,700 patients and putting them on ticagrelor and a placebo, while leaving the other 1,700 patients on ticagrelor and aspirin. All patients were evaluated between 1 and 12 months after the procedure.
During the study period, 35 patients in the ticagrelor-placebo group had a major or minor bleeding event, compared to 78 patients in the ticagrelor-aspirin group, meaning that the incidence of overall bleeding incidents was reduced by 55 percent by withdrawing aspirin. The study also analyzed major adverse cardiac and cerebrovascular events including death, heart attack, stroke, bypass graft surgery, or repeat PCI. These events occurred in 61 patients in the ticagrelor-placebo group compared to 63 patients in the ticagrelor-aspirin group, and were not statistically significant - further demonstrating that removing aspirin did no harm and improved outcomes.
“It was previously believed that discontinuing dual antiplatelet therapy within one year after PCI in patients with ACS would increase the risk of heart attack and other ischemic complications, but the present study shows that is not the case, with contemporary drug-eluting stents now used in all PCI procedures. Discontinuing aspirin in patients with a recent or threatened heart attack who are stable one month after PCI is safe and, by decreasing serious bleeding, improves outcomes,” Dr. Stone adds. “This study extends the results of prior work that showed similar results but without the quality of using a placebo, which eliminates bias from the study.”
This trial was funded by the Chinese Society of Cardiology, the National Natural Scientific Foundation of China, and Jiangsu Provincial & Nanjing Municipal Clinical Trial Project.
Mount Sinai is a World Leader in Cardiology and Heart Surgery
Mount Sinai Fuster Heart Hospital at The Mount Sinai Hospital ranks No. 1 in New York and No. 4 globally according to Newsweek’s “The World’s Best Specialized Hospitals.” It also ranks No. 1 in New York for cardiology, heart, and vascular surgery, according to U.S. News & World Report®.
It is part of Mount Sinai Health System, which is New York City's largest academic medical system, encompassing eight hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. We advance medicine and health through unrivaled education and translational research and discovery to deliver care that is the safest, highest-quality, most accessible and equitable, and the best value of any health system in the nation. The Health System includes approximately 7,400 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report's® “Best Hospitals” Honor Roll for 2023-2024.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
END
Stopping aspirin one month after coronary stenting procedures significantly reduces bleeding complications in heart attack patients
2024-04-07
ELSE PRESS RELEASES FROM THIS DATE:
Short-term incentives for exercise can lead to sustained increases in activity
2024-04-07
Short-term incentives for exercise can lead to sustained increases in activity
NIH-supported study shows certain perks can spur long-term behavior change in adults with cardiovascular disease risks
Adults with heart disease risks who received daily reminders or incentives to become more active increased their daily steps by more than 1,500 after a year, and many were still sticking with their new habit six months later, according to a study supported by the National Institutes of Health that published in Circulation. ...
Successful “first in human” clinical trial of pioneering guidance for heart bypass surgery
2024-04-07
A new approach to the guidance, planning and conduct of heart bypass surgery has been successfully tested on patients for the first time in a clinical trial coordinated by a research team at University of Galway.
The FAST TRACK CABG study, overseen by the University’s CORRIB Research Centre for Advanced Imaging and Core Lab, has seen heart surgeons plan and carry out coronary artery bypass grafting (CABG), based solely on non-invasive cardiac-CT scan images, with HeartFlow’s AI-powered blood flow analysis of the patient’s coronary arteries.
The research was published today in the European Heart Journal and is available at https://academic.oup.com/eurheartj/article-lookup/doi/10.1093/eurheartj/ehae199
The ...
Influenza vaccine immune response in patients with high-risk cardiovascular disease
2024-04-07
About The Study: High-dose influenza vaccine elicited a more robust humoral response in patients with heart failure or prior myocardial infarction enrolled in the INVESTED randomized clinical trial, with no association between seroconversion status and the risk for cardiopulmonary hospitalizations or all-cause mortality. Vaccination to prevent influenza remains critical in high-risk populations.
Authors: Scott D. Solomon, M.D., of Brigham and Women’s Hospital and Harvard Medical ...
Plozasiran (ARO-APOC3) for severe hypertriglyceridemia
2024-04-07
About The Study: This randomized clinical trial demonstrates the potential clinical utility of plozasiran, an investigational APOC3-targeted small interfering–RNA drug, to reduce triglyceride level in patients with severe hypertriglyceridemia. Additional studies will be required to determine whether plozasiran favorably modulates the risk of severe hypertriglyceridemia-associated complications.
Authors: Daniel Gaudet, M.D., Ph.D., of the Université de Montréal, is the corresponding author.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamacardio.2024.0959)
Editor’s ...
Experimental drug could further reduce lipids in the blood in high-risk patients
2024-04-07
Hypertriglyceridemia, or high levels of lipids (fats) in the blood, increases the risk of heart attack, stroke and acute pancreatitis. Currently available medications, including statins, ezetimibe, fibrates and prescription omega 3 fatty acids, typically lower triglyceride levels by anywhere from below 10% to up to 40%. These therapies help, but they are not enough to prevent cardiovascular events in everyone.
An experimental treatment could further lower triglycerides in the blood, according to a placebo-controlled ...
New evidence links passive smoking with dangerous heart rhythm disorder
2024-04-07
Berlin, Germany – 7 April 2024: Exposure to secondhand smoke – even at small amounts – is linked with greater risk of a serious heart rhythm disorder, according to research presented at EHRA 2024, a scientific congress of the European Society of Cardiology (ESC).1 The likelihood of atrial fibrillation increased as the duration of passive smoking lengthened.
“The dangers of secondhand smoke were significant regardless of whether individuals were at home, outdoors, or at work, indicating that exposure universally elevates the risk of atrial ...
Oral vaccine for UTI is potential alternative to antibiotics, finds 9-year study
2024-04-07
Recurrent Urinary Tract Infections (UTIs) can be prevented for up to nine years in more than half of people given an oral spray-based vaccine and is a potential alternative to antibiotic treatments, finds research.
Initial results from the first long-term follow-up study of the safety and effectiveness of the MV140 vaccine for recurrent UTIs are presented this weekend at the European Association of Urology (EAU) Congress in Paris.
They show that in both men and women with recurrent UTIs, 54% of study participants remained UTI-free for nine years after the vaccine, with no notable side effects reported. Full results of the study are expected to be published ...
Antibiotic prophylaxis and infective endocarditis incidence following invasive dental procedures
2024-04-06
About The Study: This systematic review and meta-analysis including data on 1.1 million cases of infective endocarditis found that antibiotic prophylaxis was associated with a reduced risk of infective endocarditis following invasive dental procedures in individuals at high risk but not in those at moderate or low/unknown risk. Currently, there is insufficient data to support any benefit of antibiotic prophylaxis in individuals at moderate risk.
Authors: Federica Turati, Ph.D., of the ...
A multimodal video-based AI biomarker for aortic stenosis development and progression
2024-04-06
About The Study: In this cohort study of patients without severe aortic stenosis undergoing echocardiography or cardiac magnetic resonance imaging, a new artificial intelligence (AI)-based video biomarker was independently associated with aortic stenosis development and progression, enabling opportunistic risk stratification across cardiovascular imaging modalities as well as potential application on handheld devices.
Authors: Rohan Khera, M.D., M.S., of the Yale School of Medicine in New Haven, Connecticut, is the corresponding author.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamacardio.2024.0595)
Editor’s ...
Inter-atrial shunts may benefit some heart failure patients while harming others
2024-04-06
Inter-atrial shunts—investigational devices that create a small pathway for blood to pass from the left to the right side of the heart in order to improve heart failure symptoms and outcomes—may be beneficial to heart failure patients with reduced left ventricular ejection fraction (LVEF) but harmful or even deadly for heart failure patients with preserved LVEF, a new Mount Sinai-led study shows.
The findings of the RELIEVE-HF trial were announced during the opening late-breaking trial session at the American College of Cardiology Scientific Sessions on Saturday, April 6. This is the first study ...