In an important step toward more effective gene therapies for brain diseases, researchers from the Broad Institute of MIT and Harvard have engineered a gene-delivery vehicle that uses a human protein to efficiently cross the blood-brain barrier and deliver a disease-relevant gene to the brain in mice expressing the human protein. Because the vehicle binds to a well-studied protein in the blood-brain barrier, the scientists say it has a good chance at working in patients.
Gene therapy could potentially treat a range of severe genetic brain disorders, which currently have no cures and few treatment options. But FDA-approved forms of the most commonly used vehicle for packaging and delivering these therapies to target cells, adeno-associated viruses (AAVs), aren’t able to efficiently cross the blood-brain barrier at high levels and deliver therapeutic cargo. The enormous challenge of getting therapies past this barrier — a highly selective membrane separating the blood from the brain — has stymied the development of safer and more effective gene therapies for brain diseases for decades.
Now researchers in the lab of Ben Deverman, an institute scientist and senior director of vector engineering at the Broad, have engineered the first published AAV that targets a human protein to reach the brain in humanized mice. The AAV binds to the human transferrin receptor, which is highly expressed in the blood-brain barrier in humans. In a new study published in Science, the team showed that their AAV, when injected into the bloodstream in mice expressing a humanized transferrin receptor, crossed into the brain at much higher levels than the AAV that is used in an FDA-approved gene therapy for the central nervous system, AAV9. It also reached a large fraction of important types of brain cells, including neurons and astrocytes. The researchers then showed that their AAV could deliver copies of the GBA1 gene, which has been linked to Gaucher’s disease, Lewy body dementia, and Parkinson’s disease, to a large fraction of cells throughout the brain.
The scientists add that their new AAV could be a better option for treating neurodevelopmental disorders caused by mutations in a single gene such as Rett syndrome or SHANK3 deficiency; lysosomal storage diseases like GBA1deficiency; and neurodegenerative diseases such as Huntington’s disease, prion disease, Friedreich’s ataxia, and single-gene forms of ALS and Parkinson’s disease.
“Since we came to the Broad we’ve been focused on the mission of enabling gene therapies for the central nervous system,” said Deverman, senior author on the study. “If this AAV does what we think it will in humans based on our mouse studies, it will be so much more effective than current options.”
“These AAVs have the potential to change a lot of patients’ lives,” said Ken Chan, a co-first author on the paper and group leader from Deverman’s group who has been working on solving gene delivery to the central nervous system for nearly a decade.
Mechanism first
For years, researchers developed AAVs for specific applications by preparing massive AAV libraries and testing them in animals to identify top candidates. But even when this approach succeeds, the candidates often don’t work in other species, and the approach doesn’t provide information about how the AAVs reach their targets. This can make it difficult to translate a gene therapy using these AAVs from animals to humans.
To find a delivery vehicle with a greater chance of reaching the brain in people, Deverman’s team switched to a different approach. They used a method they published last year, which involves screening a library of AAVs in a test tube for ones that bind to a specific human protein. Then they test the most promising candidates in cells and mice that have been modified to express the protein.
As their target, the researchers chose human transferrin receptor, which has long been the target of antibody-based therapies that aim to reach the brain. Several of these therapies have shown evidence of reaching the brain in humans.
The team’s screening technique identified an AAV called BI-hTFR1 that binds human transferrin receptor, enters human brain cells, and bypasses a human cell model of the blood-brain barrier.
“We’ve learned a lot from in vivo screens but it has been tough finding AAVs that worked this well across species,” added Qin Huang, a co-first author on the study and a senior research scientist in Deverman’s lab who helped develop the screening method to find AAVs that bind specific protein targets. “Finding one that works using a human receptor is a big step forward.”
Beyond the dish
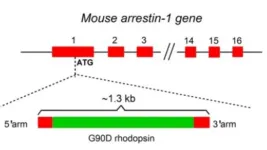
To test the AAVs in animals, the researchers used mice in which the mouse gene that encodes the transferrin receptor was replaced with its human equivalent. The team injected the AAVs into the bloodstream of adult mice and found dramatically higher levels of the AAVs in the brain and spinal cord compared to mice without the human transferrin receptor gene, indicating that the receptor was actively ferrying the AAVs across the blood-brain barrier.
The AAVs also showed 40-50 times higher accumulation in brain tissue than AAV9, which is part of an FDA-approved therapy for spinal muscular atrophy in infants but is relatively inefficient at delivering cargo to the adult brain. The new AAVs reached up to 71 percent of neurons and 92 percent of astrocytes in different regions of the brain.
In work led by research scientist Jason Wu, Deverman’s team also used the AAVs to deliver healthy copies of the human GBA1 gene, which is mutated in several neurological conditions. The new AAVs delivered 30 times more copies of the GBA1 gene than AAV9 in mice and were delivered throughout the brain.
The team said that the new AAVs are ideal for gene therapy because they target a human protein and have similar production and purification yields as AAV9 using scalable manufacturing methods. A biotech company co-founded by Deverman, Apertura Gene Therapy, is already developing new therapies using the AAVs to target the central nervous system.
With more development, the scientists think it’s possible to improve the gene-delivery efficiency of their AAVs to the central nervous system, decrease their accumulation in the liver, and avoid inactivation by antibodies in some patients.
Sonia Vallabh and Eric Minikel, two researchers at the Broad who are developing treatments for prion disease, are excited by the potential of the AAVs to deliver brain therapies in humans.
"When we think about gene therapy for a whole-brain disease like prion disease, you need really systemic delivery and broad biodistribution in order to achieve anything," said Minikel. "Naturally occurring AAVs just aren't going to get you anywhere. This engineered capsid opens up a world of possibilities."
Funding:
This work was supported by Apertura Gene Therapy, the National Institutes of Health Common Fund, the National Institute of Neurological Disorders and Stroke, and the Stanley Center for Psychiatric Research.
Paper cited:
Huang Q, Chan KY, et al. An AAV capsid reprogrammed to bind human transferrin receptor mediates brain-wide gene delivery. Science. Online May 16, 2024. DOI: 10.1126/science.adm8386.
About Broad Institute of MIT and Harvard
Broad Institute of MIT and Harvard was launched in 2004 to empower this generation of creative scientists to transform medicine. The Broad Institute seeks to describe the molecular components of life and their connections; discover the molecular basis of major human diseases; develop effective new approaches to diagnostics and therapeutics; and disseminate discoveries, tools, methods and data openly to the entire scientific community.
Founded by MIT, Harvard, Harvard-affiliated hospitals, and the visionary Los Angeles philanthropists Eli and Edythe L. Broad, the Broad Institute includes faculty, professional staff and students from throughout the MIT and Harvard biomedical research communities and beyond, with collaborations spanning over a hundred private and public institutions in more than 40 countries worldwide.
END