(Press-News.org) Giving high-risk patients access to an obesity specialist through their regular primary care clinic increased their chances of receiving at least one evidence-based weight-management treatment, and led to more weight lost in just a year, a new University of Michigan study finds.
Primary care clinicians commonly struggle to help patients develop an individualized weight-management treatment plan during short clinic visits. Previous U-M research showed that most primary care patients with obesity do not lose at least 5% of their body weight, a goal that’s been shown to reduce obesity-related health risks.
That’s why U-M’s academic medical center, Michigan Medicine, developed the Weight Navigation Program, which teams up patients with obesity and their primary care provider with a board-certified obesity specialist.
The new study evaluating results from it is published in JAMA Network Open by the multidisciplinary team that launched the WNP in fall 2020.
The new study shows that on average, patients who enrolled during the first year of the program lost about 12 pounds, or about 4.4% of their body weight, in the year after they received an individualized obesity treatment plan from an obesity specialist.
That’s compared with very little weight lost by patients similar to the WNP patients who went to a similar U-M primary care clinic that didn’t yet offer the program.
On average, all the patients started with a body mass index (BMI) around 40 kg/m2. To qualify for WNP, patients have to have a BMI above 30 kg/m2 and have at least one weight-related health condition, such as high blood pressure, sleep apnea, type 2 diabetes, or high cholesterol.
Over 40% of those in the WNP lost at least 5% of their body weight, a goal that’s been shown to reduce obesity-related health risks. In comparison, less than 20% of similar patients not in the WNP lost at least 5% of their body weight. In addition, 22% of patients in the WNP lost at least 10% of their body weight compared to less than 4% of similar patients.
The authors say the study suggests that the WNP approach should be tested in a larger clinical trial.
Meanwhile, the WNP is now available to all eligible adult patients who receive primary care through U-M Health clinics, acting as a gateway to multiple treatment options. It’s part of a wide range of weight management programs available by referral in multiple areas of U-M Health.
“The WNP is based in the idea that safe and effective obesity care can be integrated into the primary care settings where most Americans with obesity receive the vast majority of their care,” said Dina Hafez Griauzde, M.D., M.Sc., first author of the study and an internal medicine assistant professor at the U-M Medical School. “Having an obesity specialist work as part of a collaborative team to evaluate patients, help them understand their options, including potential costs, and act as a gateway to specialized care and primary care follow-up, is a model that we hope others will adopt.”
Senior author, Andrew Kraftson, M.D. is an endocrinologist who specializes in obesity medicine But a shortage of such specialists means that programs such as WNP are needed to extend their reach.
The WNP builds on the previous success of other kinds of chronic disease programs that involve closer partnership between specialists and primary care providers. One key difference: two-thirds of current obesity medicine specialists are also primary care physicians, including Griauzde and several of her co-authors.
More about the WNP
Patients referred to the WNP meet with an obesity specialist who has in-depth familiarity with all the obesity treatment options offered at U-M Health as well as community diabetes prevention programs. The obesity specialists also understand insurance coverage and costs such as copays for the different options.
After meeting with the patient, the obesity specialist provides customized treatment recommendations that address the patient’s medical situation, finances, and preferences.
Treatments can range from specialized dietary plans to anti-obesity medications to weight loss surgery. The team monitors progress and coordinates ongoing care with the primary care provider.
More about the study
The new paper tracks the care of 132 people who went through the WNP at a single primary care clinic during the program’s first year, and 132 people with similar health and demographic characteristics who received usual care at a similar U-M Health primary care clinic in that timeframe. Both groups’ records were studied for a full year, and nearly all had weight measurements available at the end of the year.
Two-thirds of both groups were female; the average age was 49 and nearly two-thirds had high blood pressure while about 60% had obstructive sleep apnea and just over 20% had type 2 diabetes.
Of all patients at the clinic offering the WNP who qualified for it, 19% of were referred to it by their primary care provider, and 11% enrolled. This is much higher than the very low percentage of U-M Health primary care patients who received a weight management treatment from their primary care provider or were referred for specialty obesity care in a previous study published by the team based on data from before the WNP launched.
When comparing the WNP patients with the usual care group, WNP patients were more likely to be directed toward health system obesity care resources, with more than twice as many patients in the WNP referred for bariatric surgery evaluations (18% vs. 9%). In all, 4% of the WNP patients had bariatric surgery within a year of starting the program, compared with none of the comparison group.
WNP patients were also much more likely to receive a referral to a program that treats patients through a low-calorie meal replacement plan, or to a program that counsels patients on following a Mediterranean-style diet, which has been shown to have benefits for weight and health.
The percentages receiving a prescription for any obesity medication were similar, at 14% of the WNP patients and 10% of control group patients.
However, the study period was before the U.S. Food and Drug Administration’s approval of semaglutide and tirzepatide for weight management and may not reflect current prescribing practices. Therefore, the researchers are doing a follow-up assessment of weight-management treatment use and patients’ weight loss since the availability of these medications.
In addition to Griauzde and Kraftson, the study’s authors are Cassie D. Turner, LMSW; Amal Othman, MD; Lauren Oshman, MD, MPH; Jonathan Gabison, MD; Patricia K. Arizaca-Dileo, MD; Eric Walford, MD; James Henderson, PhD; Deena Beckius, MPH; Joyce M. Lee, MD, MPH; Eli W. Carter, MPH; Chris Dallas, BBA; Kathyrn Herrera-Theut, MD; Caroline R. Richardson, MD; Jeffrey T. Kullgren, MD, MS, MPH; Gretchen Piatt, PhD, MPH; and Michele Heisler, MD, MPA.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health, through a pilot grant from the Michigan Center for Diabetes and Translational Research (DK092926), and other grants (DK123416, DK089503, DK020572, DK092926) including funds from the Michigan Nutrition Obesity Research Center, the Michigan Diabetes Research Center and the Elizabeth Weiser Caswell Diabetes Institute.
Multiple authors of the paper are members of the Caswell Diabetes Institute and the U-M Institute for Healthcare Policy and Innovation, as well as being current or former faculty and staff in the Department of Internal Medicine and Family Medicine at the U-M Medical School.
A Primary Care–Based Weight Navigation Program, JAMA Network Open, doi:10.1001/jamanetworkopen.2024.12192
END
Study comparing U-M Weight Navigation Program with usual care for high-risk patients shows higher use of evidence-based treatments and more weight lost
2024-05-21
ELSE PRESS RELEASES FROM THIS DATE:
Stuart Orkin awarded the Shaw Prize in Life Science & Medicine 2024 for groundbreaking hemoglobin research
2024-05-21
[BOSTON, MAY 21, 2024] – Stuart Orkin, MD, a researcher at the Dana-Farber/Boston Children's Cancer and Blood Disorders Center and David G. Nathan Distinguished Professor of Pediatrics at Harvard Medical School, has been honored with The Shaw Prize in Life Science & Medicine for his pioneering work discovering the genetic and molecular mechanisms underlying the switch from fetal to adult hemoglobin. Dr. Orkin shares the prize with Swee Lay Thein, PhD, Senior Investigator and Chief of the Sickle Cell Branch of National Heart, ...
Drug-like inhibitor shows promise in preventing flu
2024-05-21
LA JOLLA, CA—Currently available flu medications only target the virus after it has already established an infection, but what if a drug could prevent infection in the first place? Now, scientists at Scripps Research and the Albert Einstein College of Medicine have designed drug-like molecules to do just that, by thwarting the first stage of influenza infection.
The drug-like inhibitors block the virus from entering the body’s respiratory cells—specifically, they target hemagglutinin, a protein on the surface of type A influenza viruses. The findings, published in the Proceedings of the National Academy of Sciences ...
Study finds widespread ‘cell cannibalism,’ related phenomena across tree of life
2024-05-21
In a new review paper, Carlo Maley and Arizona State University colleagues describe cell-in-cell phenomena in which one cell engulfs and sometimes consumes another. The study shows that cases of this behavior, including cell cannibalism, are widespread across the tree of life.
The findings challenge the common perception that cell-in-cell events are largely restricted to cancer cells. Rather, these events appear to be common across diverse organisms, from single-celled amoebas to complex multicellular animals.
The widespread occurrence of such interactions in non-cancer cells suggests that these events are not inherently "selfish" or "cancerous" ...
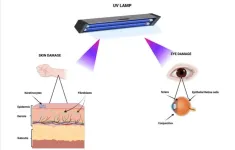
Germicidal lamps using UV-C radiation may pose health safety issues
2024-05-21
“Despite the potential advantages of utilizing UV-C radiation for deactivating pathogens such as SARS-CoV-2, the prevailing conclusion remains that UV-C radiation poses concurrent risks to human health.”
BUFFALO, NY- May 21, 2024 – A new research paper was published in Aging (listed by MEDLINE/PubMed as "Aging (Albany NY)" and "Aging-US" by Web of Science) Volume 16, Issue 9, entitled, “Germicidal lamps using UV-C radiation may pose health safety issues: a biomolecular analysis of their effects on apoptosis and senescence.”
The battle against the COVID-19 pandemic has spurred a heightened state of vigilance in global healthcare, ...
Inhibitory effect of miR-377 on prostate cancer cells
2024-05-21
“Our research findings suggest that miR-377 could potentially serve as a valuable therapeutic strategy for the treatment of prostate cancer (PCa).”
BUFFALO, NY- May 21, 2024 – A new research paper was published in Genes & Cancer on May 16, 2024, entitled, “Inhibitory effect of miR-377 on the proliferative and invasive behaviors of prostate cancer cells through the modulation of MYC mRNA via its interaction with BCL-2/Bax, PTEN, and CDK4.”
The MYC gene is a regulatory and proto-oncogenic gene that is overexpressed in the majority of prostate cancers (PCa). Numerous studies have indicated that aberrant expression of microRNAs is involved in the ...
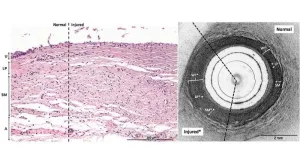
Innovative imaging technique may revolutionize ureteral thermal injury detection
2024-05-21
In a groundbreaking study, scientists have explored a novel approach to detect electrothermal ureteral injuries, a common complication during pelvic surgery. The ureters, delicate tubes that transport urine from the kidneys to the bladder, are particularly vulnerable due to their proximity to other anatomical structures. Unfortunately, current detection methods often fall short in promptly identifying subtle thermal injuries, which can take days or even weeks to manifest.
Enter optical coherence tomography ...
Conservation of nature’s strongholds needed to halt biodiversity loss
2024-05-21
To achieve global biodiversity targets, conservationists and governments must prioritize the establishment and effective management of large, interconnected protected areas with high ecological integrity, John G. Robinson from the Wildlife Conservation Society, US, and colleagues argue in an essay publishing May 21st in the open-access journal PLOS Biology.
The Kunming–Montreal Global Biodiversity Framework (GBF), signed at the 2022 Conference of Parties to the UN Convention on Biological Diversity in Montreal, recognized the importance of protecting large areas of natural habitat to maintain the resilience and integrity of ecosystems. To halt biodiversity ...
Body lice may be bigger plague spreaders than previously thought
2024-05-21
A new laboratory study suggests that human body lice are more efficient at transmitting Yersinia pestis, the bacterium that causes plague, than previously thought, supporting the possibility that they may have contributed to past pandemics. David Bland and colleagues at the United States’ National Institute of Allergy and Infectious Diseases present these findings in the open-access journal PLOS Biology on May 21st.
Y. pestis has been the culprit behind numerous pandemics, including the Black Death of the Middle Ages that ...
Gun violence touches nearly 60 percent of Black Americans – and predicts disability
2024-05-21
Roughly 60 percent of all Black Americans are exposed to some form of gun violence, and such exposures predict elevated rates of disability, according to Rutgers Health research.
Survey data from 3,015 Black Americans linked specific disabilities ranging from trouble concentrating to difficulty dressing or bathing with exposure to various types of gun violence: being shot, being threatened with a firearm, knowing a shooting victim, and witnessing a shooting or hearing of one nearby.
“Traditionally, the majority of efforts related to gun violence have focused on reducing homicides, but this study indicates that we need ...
A rise in sea urchins and related damage to kelp forests impacts Oregon’s gray whales and their food
2024-05-21
NEWPORT, Ore. – A recent boom in the purple sea urchin population off the southern Oregon Coast appears to have had an indirect and negative impact on the gray whales that usually forage in the region, a new study shows.
When urchin numbers rise, the spiky marine invertebrates can devour kelp forests that are a critical habitat for zooplankton, the tiny aquatic organisms that are the primary prey of many marine animals. Damaged kelp forests lead to reductions in zooplankton, and with fewer zooplankton to feed on, gray whales spend less time foraging there, researchers with Oregon State University’s Marine Mammal Institute found.
“This study shows the cascading ...