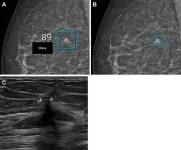
The liquid biopsy technique applied in this work is based on the sequencing of the entire tumor genome from 138 patients and the monitoring of mutations in the blood. This approach achieves high sensitivity in detecting the tumor signal in the blood (1/1,000,000 DNA molecules), and the patterns found reflect how patients respond to immunotherapy.
This study is part of the Comprehensive Program of Cancer Immunotherapy and Immunology (CAIMI) at VHIO, funded by the BBVA Foundation, and is co-led by Dr Rodrigo Toledo, head of the Biomarkers and Clonal Dynamics Group at the Vall d’Hebron Institute of Oncology (VHIO), and Dr Elena Garralda, director of the Molecular Cancer Therapy Research Unit UITM-CaixaResearch.
This work was selected as an oral presentation at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting held in Chicago from 31 May to 4 June.
Dr Rodrigo Toledo, head of the Biomarkers and Clonal Dynamics Group at VHIO and coordinator of the liquid biopsy working group at the Center for Biomedical Research in Cancer Network (CIBERONC), presents today at ASCO a study conducted in collaboration with the Molecular Therapies Research Unit UITM-CaixaResearch and the Early Clinical Drug Development Group at VHIO, led by Dr Elena Garralda and supported by the “la Caixa” Foundation.
This study, which is part of the Comprehensive Program of Cancer Immunotherapy and Immunology (CAIMI) at VHIO funded by the BBVA Foundation, demonstrates the utility of analysing circulating tumor DNA (ctDNA) through a high-sensitivity liquid biopsy platform.
This technology can detect up to one mutated ctDNA molecule among one million circulating DNA molecules in the patient's blood, providing information that allows researchers to predict the response to immunotherapy in patients with various types of cancer.
Positive levels of ctDNA detected in 99% of initial samples
The study was conducted on a cohort of 138 patients with refractory metastatic tumors of 18 different cancer types, who received 1 to 3 successive lines of treatment with immunotherapy drugs in the context of phase 1 clinical trials.
The tumor signal in the blood was detected in 99% of plasma samples taken before starting treatment. Lower initial ctDNA values were associated with longer progression-free survival and overall survival. Early reduction in ctDNA levels after the start of treatment was associated with significant increases in disease stability and survival. Finally, the elimination of ctDNA after the start of immunotherapy translated into radiological responses and significant improvements in both progression-free survival and overall survival.
“The information provided by the ultrasensitive liquid biopsy could allow us to predict whether the treatment we are studying offers clinical benefits to the patient before it can be objectified through radiological images using the criteria established to evaluate the response in phase 1 clinical trials,” comments Dr Elena Garralda, co-coordinating researcher of the study and director of the Molecular Therapies Research Unit UITM-CaixaResearch at VHIO.
“This anticipation can be crucial for making the most appropriate clinical decisions for our patients. Being able to quickly assess whether it is advisable for them to continue participating in the clinical trial or, on the contrary, if we should propose a new therapeutic strategy.”
Ultrasensitive Liquid Biopsy: What does it consist of?
As a non-invasive technique, analysing ctDNA before treatment and serially during the course of the disease allows us to understand the genetic changes occurring in the tumor and to better comprehend its evolution.
“However,” explains Dr Rodrigo Toledo, co-coordinator and presenter of the study, and head of the Biomarkers and Clonal Dynamics Group at VHIO, “one of the limitations of liquid biopsy techniques is sensitivity. In this project, we used a liquid biopsy technique based on whole-genome sequencing of the patient's tumor, which allowed us to detect and monitor thousands of patient-specific tumor mutations in their blood.”
“This is an ultrasensitive technique that enabled us to detect the tumor signal in blood samples collected serially, before and during immunotherapy treatment, and we were able to identify specific patterns that correlated with the response or resistance to treatment.”
“The study we are presenting today at ASCO demonstrates the potential of liquid biopsy to predict prognosis and response to immunotherapy treatment in patients with various types of advanced-stage tumors,” says Toledo.
The Importance of Immune Checkpoint Inhibitors
Under normal conditions, the immune system has proteins known as immune checkpoints that serve to prevent T cells from attacking the body's healthy cells. Tumor cells exploit this control system to evade the immune system and grow. “In recent decades, the advent of immune checkpoint inhibitor drugs has brought about a paradigm shift in cancer treatment. These drugs block immune checkpoints so that T cells can recognize tumor cells as foreign and destroy them,” explains Dr Elena Garralda. Even so, many patients do not respond and research into new drugs that act on the immune system has been growing in recent years, which is reflected in the large number of early-phase clinical trials of this type of treatment.
In the context of early-phase clinical trials of new immune checkpoint inhibitor drugs or new combinations, it is necessary to determine as quickly as possible which patients will benefit clinically from this therapy. “In this regard, analysing ctDNA in blood through liquid biopsy to monitor tumor evolution can help us make the most appropriate clinical decisions for each patient.”
References
Abstract #457032
Rodrigo Toledo, Alma M Calahorro García, Oriol Mirallas, Ana Moreno, Vladimir Galvao, Guzmán Alonso, Maria Vieito, Irene Brana, Arjun Oberoi, M. Julia Lostes-Bardaji, Jose Jimenez, Marta Sanz, Cristina Viaplana, Raquel Perez-Lopez, Paolo Nuciforo, Charles Abbott, Jason Pugh, Richard Chen, Sean Boyle, Elena Garralda.
Prognostic and predictive value of ultrasensitive ctDNA monitoring in a metastatic pan-cancer cohort treated with immune checkpoint inhibitors in the context of phase 1 clinical trials.
Session details
2024 ASCO Annual Meeting
Clinical Science Symposium
Hitting the Mark: The Ongoing Search for Immunotherapy Biomarkers
Primary Track: Developmental Therapeutics—Immunotherapy
4 June – 8 am GMT-5
location_onS406
Speaker: Rodrigo Toledo, VHIO
Chairs: Elena Elez, Vall d'Hebron University Hospital - Benoit Rousseau, Gastrointestinal Oncology Service, Memorial Sloan Kettering Cancer Center
###
About VHIO
The Vall d’Hebron Institute of Oncology (VHIO), established in 2006 and located within the Vall d’Hebron Campus, is a reference comprehensive cancer center for personalized medicine in oncology. Through our purely translational and multidisciplinary research model, we aim to improve the prevention, early diagnosis and treatment of cancer by transforming the latest scientific discoveries made in the laboratory into early phase clinical trials for the development of more effective therapies to improve the quality of life and survival of cancer patients.
VHIO forms part of the CERCA – Research Centres of Catalonia system and is accredited as a Severo Ochoa Center of Excellence.
Research at VHIO would not be possible without the support received from our patrons - Generalitat de Catalunya, Fundació Privada CELLEX, "La Caixa" Foundation, Fundación FERO, and the Fundación BBVA, the public funding it receives as well as the generous support from institutional supporters, private institutions, companies, associations, societies, and individual donors. Only with such continued support will VHIO continue to advance personalized and targeted therapies against cancer.
###
END