Novel liquid biopsy methodology enables the monitoring of disease evolution in patients with metastatic prostate cancer
Extracellular vesicles shed by prostate cancer cells to the bloodstream contain tumor-derived material that can be used as biomarkers of therapy response and resistance in patients with metastatic disease.
Published today in the journal Cancer Cell, results of a VHIO-led study show that a newly developed liquid biopsy-based approach can monitor tumor gene expression through RNA contained in circulating extracellular vesicles secreted by cancer cells.
These findings could help to predict response to treatment, contribute to the development of new combination strategies to combat mechanisms of acquired drug resistance, and expand the opportunities to study cancer from liquid biopsies.
This work was mainly supported by funding received from the ”la Caixa” Foundation, FERO Foundation, and CRIS Cancer Foundation.
Published today in Cancer Cell (1), results of a study directed by Joaquin Mateo, Head of the Vall d’Hebron Institute of Oncology’s (VHIO) Prostate Cancer Translational Research Group, show that DNA/RNA material contained in circulating extracellular vesicles secreted into the blood stream by tumor cells, captures cancer genomics and transcriptomic evolution in patients with metastatic prostate cancer.
“Our findings open avenues for biomarkers of therapy response and acquired drug resistance to help guide clinical decisions in individual patients with metastatic prostate cancer throughout the course of disease,” says Joaquin Mateo, Medical Oncologist at the Vall d’Hebron University Hospital (HUVH), Vall d’Hebron Campus, and Corresponding Author of this VHIO-led study.
With an estimated 1.5 million new cases and 397,000 deaths worldwide, prostate cancer is the world’s second most frequent cancer and the fifth leading cause of cancer death among men in 2022. Mortality rates have decreased in most high income-countries since the mid-1990’s, likely reflecting advancements in treatments and earlier detection (2). Nowadays, the majority of prostate cancer patients diagnosed at an early stage can be cured through cancer surgery, radiotherapy or brachytherapy with or without hormone therapy.
In metastatic prostate cancer, novel systemic therapies, hormone-based treatments or chemotherapy have improved the survival of patients in this setting, but responses to treatment are highly heterogeneous, and tumors eventually develop cancer drug resistance.
“The development of new tools and the identification of novel biomarkers of response and resistance are key to guiding and adapting treatment strategies based on the monitoring of tumor evolution in individual patients,” adds Mateo.
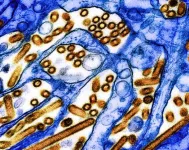
Circulating extracellular vesicles
Under normal conditions, extracellular vesicles are conduits of intercellular communication and mediators of various biological processes. These heterogeneous particles contain proteins, lipids, metabolites, RNA and DNA as cargo. Extracellular vesicles produced by tumor cells promote cancer cell communication, and their protein load composition plays a key role in tumor progression, immune regulation, and metastasis.
“However, the potential of tumor extracellular vesicles as a source of clinically relevant DNA and RNA biomarkers remains largely unexplored. We have now developed a new liquid biopsy application for the analysis of circulating vesicles secreted by cancer cells and performed multi-omic profiling for the genomic and transcriptomic characterization of these tumors,” explains Irene Casanova, an Associate Investigator of Joaquin Mateo’s group and First Author of this Report article.
The transcriptomic and genomic profiling of metastatic prostate cancer in liquid biopsy
The investigators analyzed liquid biopsies—collected by plasma series sampling throughout the course of disease—of a retrospective cohort of 53 metastatic castration-resistant prostate cancer patients who received treatment with hormone therapy or chemotherapy. They studied DNA and RNA in circulating extracellular vesicles, results of which confirm that these vesicles contain tumor-derived genetic material that can help to identify specific mutations present in tumor cells and forecast the evolution of disease.
Using a newly developed liquid biopsy technique, findings demonstrate that DNA and RNA contained in circulating vesicles reflect the genomic and transcriptomic features in metastatic prostate cancer. Furthermore, results of mRNA expression analysis—performed for the first time in extracellular vesicles in liquid biopsies—enables the monitoring of on-therapy changes in these tumors.
“The study of transcriptomic features by liquid biopsy in clinical samples has mostly been unsuccessful due to the rapid degradation of RNA when it is not shielded by the cell membrane. Our study shows that tumor mRNA encapsulated in circulating extracellular vesicles is protected and therefore represents a promising source of clinically relevant information,” adds Casanova.
Carried out in collaboration with colleagues at the Principe Felipe Research Institute (CIPF) in Valencia, and the Spanish National Cancer Research Center (CNIO), Madrid, Spain, the researchers have characterized the transcriptomic profile of these tumors that could serve as a biomarker of response or resistance to therapy. Their findings could also expand the opportunities to study cancer from minimally invasive liquid biopsies.
“Drug resistance remains a major challenge in more effectively treating cancer. Adaptive mechanisms of resistance occur more rapidly and dynamically than mutations driving acquired resistance. Monitoring these changes as they occur by liquid biopsy will enable real‐time clinical decision‐making and the selection of adaptive treatments to help combat evolving tumor dynamics earlier,” concludes Joaquin Mateo.
This work was funded by a ”la Caixa” Foundation Junior Leader Fellowship to Irene Casanova and a grant from the FERO Foundation and Ramon Areces Foundation to Joaquin Mateo. VHIO’s Prostate Cancer Translational Research Group is also supported by funding received from the CRIS Cancer Foundation.
END