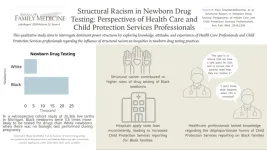
Structural Racism and Inconsistent Hospital Policies Result in Health Care Professionals Disproportionately Testing Black Newborns for Prenatal Drug Exposure
Background and Goal: Black birthing parents and their newborns disproportionately experience newborn drug testing for prenatal substance exposure by health care professionals. This practice contributes to Child Protective Services reporting, family separation, and termination of parental rights. This qualitative study, conducted at the University of Michigan in Ann Arbor, MI, explored knowledge, attitudes, and experiences of health care professionals and Child Protective Services professionals regarding the influence of structural racism on inequities in newborn drug testing practices.
Study Approach: This qualitative analysis is the third qualitative phase of a larger antiracist, justice-informed, community-engaged, multiphase mixed methods study. For this phase, researchers conducted semi-structured interviews between May 2021 and October 2022 with 30 physicians, midwives, nurses, social workers, and Child Protective Services professionals. Researchers also conducted inductive, reflexive thematic analysis, using elements of the Levels of Racism Framework, the Theoretical Domains Framework, and the Public Health Critical Race Praxis.
Main Results: Researchers identified three primary themes: (A) Levels of racism beyond the hospital structure contributed to higher rates of drug testing of Black newborns; (B) Inconsistent hospital policies led to racialized application of state law and downstream Child Protective Services reporting; and (C) health care professionals’ knowledge of the benefits and disproportionate harms of Child Protective Services reporting on Black families influenced their testing decision making.
Why It Matters: Health care professionals recognized structural racism as a driver of disproportionate newborn drug testing, but their beliefs, lack of knowledge, and skill limitations were barriers to dismantling power structures impeding systems-level change.
Structural Racism in Newborn Drug Testing: Perspectives of Health Care and Child Protective Services Professionals
P. Paul Chandanabhumma, PhD, MPH, et al
Department of Family Medicine and Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, Michigan
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
There will be an accompanying Annals of Family Medicine Podcast episode in which lead authors and researchers, Dr. Carol Shetty and Dr. Lauren Oshman, discuss this important study in detail. The episode will be accessible on July 22nd at 5 PM here.
Visual Abstract:
_____________________________________________________________________________________
Editorial
Editorial Highlights Structural Racism in Newborn Drug Testing, Calls for Policy Changes
Background: In this editorial, physicians trained in OB/GYN, urogynecology, medicine/pediatrics, allergy/immunology, and family medicine share their perspectives on an informative and compelling qualitative study titled, “Structural Racism in Newborn Drug Testing: Perspectives of Health Care and Child Protective Services Professionals.” The physicians, each of whom have expertise on racism, discuss the study, which examines the disproportionate use of newborn drug testing on Black newborns to detect prenatal substance abuse.
Key Argument: The editorialists highlight that ingrained stereotypes and inconsistent hospital policies create an environment where newborn drug testing disproportionately targets Black families. They emphasize that health professionals often equate Black race with drug use during pregnancy, leading to an increase in harmful referrals to child protective services. The editorial calls for adherence to guidelines recommending questionnaires for the birthing parents instead of newborn testing. The physicians also call for the establishment of consistent policies to reduce these biases.
Why It Matters: The editorialists stress that clear, consistent policies are important to mitigate structural racism in health care. The harmful effects of biased newborn drug testing can be prevented, and trust between Black families and health systems restored by following recommended guidelines and ensuring equitable treatment. The Substance Abuse Disorder and Family Engagement (SAFE) in Recovery Act are legislative efforts highlighted as positive steps towards supporting families and reducing unnecessary separations.
Stop Testing Black Babies!
José E. Rodríguez, MD, et al
Family and Preventive Medicine, University of Utah, Salt Lake City, Utah
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Study Shows Post-COVID Conditions in Primary Care Are Comparable to Flu and Lower Than Subspecialty and Hospital Settings
Background and Goal: COVID-19 has been considered a condition leading to other post-COVID chronic conditions frequently diagnosed in the primary care setting. This study examines the prevalence of post-COVID conditions among adult patients diagnosed with COVID-19 across the United States from 2020-2021. The study then compares the post-COVID conditions among those patients to patients with influenza-like illness and those who had regular wellness visits but weren’t diagnosed with COVID-19. The goal was to understand the prevalence and types of post-COVID conditions over time, and to see if COVID-19 led to more long-term health problems.
Study Approach: The study was conducted by researchers from Stanford University, the CDC, the American Board of Family Medicine Foundation, and the Institute for Healthcare Policy and Innovation at the University of Michigan. Researchers used the American Family Cohort, a national primary care registry to examine data from the years 2018 to 2021. They compared data from three groups: people who had COVID-19, people from 2018-2019 with flu-like illnesses, and people from 2020-2021 who had regular health check-ups but not COVID-19. Researchers matched people in each group who were similar in age, gender, health status, and other factors. They then checked how many people in each group had long-lasting health problems, looking at the overall number and type of health issues each group had over time.
Main Results:
Patients with COVID-19 had a higher prevalence of certain issues compared to patients with influenza-like illness. Issues included: breathing difficulties, type 2 Diabetes , fatigue and sleep disturbances However, all prevalence differences were less than 3%. This difference suggests that while COVID-19 may lead to specific new health problems, the overall long-term health impact is similar to that of other respiratory illnesses like influenza.
There were no significant differences in the monthly increase of new health conditions between patients with COVID-19 and those with influenza-like illness. Both groups had a similar rate of increase in health problems each month after their diagnosis.
Patients with COVID-19 had a higher prevalence of breathing difficulties and type 2 diabetes compared to patients who had regular wellness visits but did not contract COVID-19. While the differences in prevalence were statistically noted, they are described as modest. This indicates that although there is an increase, it is not dramatically higher.
Why It Matters: This study demonstrates the moderate burden of post-COVID conditions in primary care. The conditions include breathing difficulties, fatigue, sleep disturbances, and type 2 diabetes. Using real-world data from a national primary care registry, the study provides a different picture of the prevalence and impact of post-COVID conditions compared to specialty or hospital settings. Understanding the types and prevalence of post-COVID conditions helps health care professionals diagnose and treat these conditions more effectively.
Post-COVID Conditions in US Primary Care: A PRIME Registry Comparison of Patients With COVID-19, Influenza-Like Illness, and Wellness Visits
Esther E. Velásquez, ScD, et al
Center for Population Health Sciences, Stanford School of Medicine, Stanford University, Palo Alto, California
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Visual Abstract:
____________________________________________________________________________________
Original Research
Long-Term Sulfonylurea Use Linked to Higher Risk of Low Blood Sugar Unawareness in Type 2 Diabetes Patients
Background and Goal: Sulfonylureas are a class of oral medications used to manage blood glucose levels in patients with type 2 diabetes. These drugs increase insulin production regardless of blood sugar levels. For this reason, the drugs can cause blood sugar to drop too low, leading to hypoglycemia. The goal of this study was to compare how prevalent impaired awareness of hypoglycemia was when patients with type 2 diabetes were treated with either insulin or sulfonylureas for both long and short-term periods.
Study Approach: Researchers collected data from a group of 898 participants with type 2 diabetes enrolled in pharmacies, clinics, and health bureaus of Tainan City, Taiwan. Participants were treated with insulin or sulfonylurea between August and November 2022. Researchers assessed the participants’ degree of impaired awareness of their hypoglycemia status, using the Chinese versions of the Clarke and Gold questionnaires.
Main Results:
Up to 94.3% of participants, half male and half female and mostly aged 40-69, visited a clinician as an outpatient every 2-3 months for diabetes care. For participants who used the medication for less than a year, the prevalence of impaired awareness of hypoglycemia in sulfonylurea users was 47.8% (Gold) and 30.4% (Clarke). The prevalence increased to 70.7% (Gold) and 56.9% (Clarke) for users treated with sulfonylurea for more than five years.
For insulin user participants who used the medication for less than a year, the prevalence of impaired hypoglycemia awareness was 57.3% (Gold) and 30.1% (Clarke). This decreased to 41% (Gold) and 28.2% (Clarke) for participants who used the medication for more than five years. Regular ambulatory care with tests, including blood glucose and retina exams, was associated with lower odds of impaired awareness of hypoglycemia in both sulfonylurea and insulin users.
Why It Matters: Using sulfonylureas long-term is associated with impaired awareness of low blood sugar in patients with type 2 diabetes. The longer the patient uses this medication, the higher the risk of hypoglycemia unawareness. Current guidelines recommend using newer classes of medications that offer a reduced risk of hypoglycemia to treat type 2 diabetes over sulfonylureas, which are commonly used due to their affordability.
Long-Term Sulfonylurea Use and Impaired Awareness of Hypoglycemia Among Patients With Type 2 Diabetes in Taiwan
Chung-Yi Li, PhD, et al
Department of Family Medicine, National Cheng Kung University Hospital, Tainan, Taiwan
Department of Public Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Visual Abstract:
_____________________________________________________________________________________
Original Research
Pandemic Lockdown Exacerbated Ongoing Declines in Continuity of Care
Within English General Practices
Background and Goal: Longitudinal continuity of care is the repeated contact between an individual and the same general practitioner (GP). This type of continuity of care is widely regarded as a cornerstone of primary care. Higher levels of longitudinal continuity of care are associated with better health outcomes, greater patient satisfaction, and more cost-effective use of health care resources. This study aimed to describe more recent variations between practices in the slopes of longitudinal continuity of care levels across the COVID-19 pandemic. The study also set out to determine if practice-related factors predicted these variations.
Study Approach: Researchers used the General Practice Patient Survey for the period of 2018- 2022 to analyze data from English general practices with longitudinal continuity of care information. The study included only active practices with at least 750 registered patients. The outcome was the percentage of each practice’s patients who had both a preferred GP and the ability to see that GP repeatedly. The study examined eleven population and practice related factors as potential independent predictors of longitudinal continuity of care variation. Factors included baseline longitudinal continuity of care (in 2018), English National Health Service (NHS) region (London, South East, South West, East of England, Midlands, North East and Yorkshire, or North West), deprivation score, rurality (urban or rural), percentage of White patients and numbers of general practitioners and nurses per 10,000 patients.
Main Results:
Overall Decline in Continuity: In 2018-2022, the mean of longitudinal continuity of care levels across 6,010 practices decreased markedly from 29.3% to 19.0% of patients.
Steeper Decline Post-COVID-19 Lockdown: This decline steepened in 2021- 2022, following the COVID-19 lockdown.
Increasing Variations in Continuity: The coefficient of variation (a measure of relative variability) increased from 48.1% to 63.6% in 2018-2022, indicating progressively widening differences between practices.
Predictors of Variations in Decline of Continuity:
More general practitioners and higher percentages of patients seen on the same day as booking predicted slower declines.
Higher baseline longitudinal continuity of care, living in four of the six regions outside London, and higher percentages of White ethnicity predicted faster declines.
Why It Matters: The findings suggest that factors linked to greater appointment availability predicted slower declines in longitudinal continuity of care levels in English general practices. To prevent the further loss of continuity, the researchers urge immediate nationwide action to improve appointment availability.
Ongoing Decline in Continuity with GPs in English General Practices: A Longitudinal Study Across the COVID-19 Pandemic
Louis Steven Levene, FRCGP, PhD, et al
Department of Population Health Sciences, University of Leicester, Leicester,
England
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Visual Abstract:
_____________________________________________________________________________________
Original Research
Pandemic’s Impact on Primary Care: Significant Drop in Visits and Uneven Telehealth Use Across Patient Groups
Background and Goal: The COVID-19 pandemic likely worsened disparities in access to primary care. The goal of this study was to quantify the nationwide decline in primary care visits and the increase in telehealth utilization and explore whether certain groups of patients were disproportionately impacted.
Study Approach: Researchers used primary care electronic health record data from the American Family Cohort— to examine the percentage change in total visit volume, change in in-person visit volume, and telehealth conversion ratio (how much care was delivered via telehealth, defined as the number of pandemic telehealth visits divided by the total number of pre-pandemic visits). They then assessed whether these outcomes were associated with certain patient characteristics. The characteristics included age, gender, race, ethnicity, comorbidities (additional medical conditions that occur alongside a primary illness), rurality, and area-level social deprivation.
Main Results:
The primary sample included 1,652,871 patients with 8,833,434 visits from 408 practices and 2,328 clinicians.
During the pandemic, decreases of 7% in total and 17% in in-person visit volume were observed as well as a 10% telehealth conversion ratio.
The largest declines in overall and in-person visit volume were observed in pediatric (-24% Total, -31% In-Person) and Asian patients (-11%, -24%) and for those with comorbidities (-9%, -20%).
The smallest declines in total visit volume were observed in 18 to 64 year-old patients (-2%) and Black or African American patients (-2%).
Telehealth usage was highest among Hispanic patients (17%) and those living in urban areas (12%).
Why It Matters: Decreases in primary care visit volume were partially offset by increasing telehealth use for all patients during the COVID-19 pandemic. However, the magnitude of these changes varied significantly by patient characteristics. These variations underscore the need for health care systems to enhance telehealth infrastructure and address barriers in rural and underserved areas to ensure equitable access to care, and the importance of maintaining continuous access to primary care.
The Disproportionate Impact of Primary Care Disruption and Telehealth Utilization During COVID-19
Zachary J. Morgan, MS, et al
American Board of Family Medicine, Lexington, Kentucky
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Visual Abstract:
______________________________________________________________________
Systematic Review
Nirmatrelvir/Ritonavir Antiviral Combination Shows Potential in Reducing COVID-19 Hospitalizations
Background and Goal: SARS-CoV-2, the virus responsible for the COVID-19 pandemic, remains in circulation. The focus has now shifted to testing and treating symptomatic patients. An antiviral drug combination, nirmatrelvir/ritonavir, is approved for treating mild to moderately severe COVID-19 in non-hospitalized patients at risk of worsening symptoms, hospitalization, and death. This systematic review aimed to summarize published evidence on the efficacy, effectiveness, and safety of nirmatrelvir/ritonavir for COVID-19. The review also intended to assess the robustness of the evidence from randomized controlled trials.
Study Approach: A rapid evidence review and comprehensive analysis was conducted. Researchers included both randomized controlled trials and real-world observational studies, adhering to appropriate WHO and Cochrane guidelines. The review involved thorough literature searches in multiple databases, screening of articles, and detailed data extraction. The outcomes of interest were how well the treatment cleared the virus, prevented symptoms from worsening, and reduced hospitalizations and deaths from any cause. Outcomes of interest also included the treatment’s safety, including any serious side effects. The quality and risk of bias of the studies were assessed using established tools. Researchers performed statistical analyses, including trial sequential analysis, to determine if the sample sizes were sufficient to draw reliable conclusions.
Main Results:
• Randomized Controlled Trials: Nirmatrelvir/ritonavir significantly reduced COVID-19 hospitalizations compared to placebo or no treatment. However, the treatment showed no significant difference in reducing worsening severity, viral clearance, adverse events, serious adverse events, or all-cause mortality. The analysis confirmed a sufficient sample size for hospitalization reduction, but sample sizes for the other outcomes were insufficient. This insufficiency made the observed lack of difference inconclusive.
• Real-World Studies: Nirmatrelvir/ritonavir significantly reduced both hospitalizations and all-cause mortality compared to no treatment. However, there was a high level of variability in the results. The high variability level was likely due to differences in patient characteristics and care practices across the studies.
Why It Matters: The nirmatrelvir/ritonavir regimen shows promise in reducing COVID-19 hospitalizations and potentially lowering all-cause mortality in adults with mild to moderately severe COVID-19. However, the evidence is limited and varied, especially from real-world studies, indicating that more rigorous randomized controlled trials are needed to draw firm conclusions. This review highlights the regimen’s potential effectiveness in reducing hospitalizations. However, the evidence remains inconclusive for other outcomes. Understanding these nuances is important for health care professionals and policy makers as they navigate treatment options for COVID-19.
Nirmatrelvir/Ritonavir Regimen for Mild/Moderately Severe COVID-19: A Rapid Review With Meta-Analysis and Trial Sequential Analysis
Dr. George N. Okoli, MD, PhD
George and Fay Yee Centre for Healthcare Innovation, University of Manitoba, Winnipeg, Manitoba, Canada
Rady Faculty of Health Sciences, College of Pharmacy, University of Manitoba, Winnipeg, Manitoba, Canada
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Visual Abstract:
__________________________________________________________________________________
Original Research
Health Care Providers Weigh In On Their Experiences Developing an AI Tool to Understand Primary Care Patients’ Social Determinants of Health
Background and Goal: Social determinants of health are the conditions in which people are born, grow, live, work, and age. These conditions include income, education, and access to health care. Knowledge of these factors is essential for primary care clinicians to deliver fair and complete care, plan programs and distribute resources effectively. However, this information is rarely captured consistently in clinical settings. This study identified how an Artificial Intelligence (AI) social determinants of health tool can be designed using a collaborative design strategy with input from primary care team members.
Study Approach: Semi-structured, 50-minute workshops were conducted with the St. Michael’s Hospital Academic family health team in Toronto, Ontario, Canada from May to June 2023. Participants were asked for their feedback on a proposed AI-based tool that derives patient social determinants of health from electronic health record (EHR) data.
Main Results:
15 participants of the health team participated across 4 workshops.
Participants reported that most patient information was not available or difficult to find in their EHR.
Participants recommended starting with 1-2 social determinants (such as income and housing). They also emphasized the need for adequate resources, staff, and training materials.
Many challenges were reported, including how to discuss the use of AI with patients and confirm their social needs identified by the AI tool.
Why It Matters: The integration of AI into health care is rapidly advancing, presenting both opportunities and challenges. This study provides valuable insights from end users on the meaningful design and implementation of an AI-based tool for social data in primary care. The AI-based tool can potentially improve patient care and reduce clinician burnout.
Developing an AI Tool to Derive Social Determinants of Health for Primary Care Patients: Qualitative Findings From a Codesign Workshop
Stephanie Garies, PhD, et al
Department of Family & Community Medicine, St. Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Visual Abstract:
_____________________________________________________________________________________
Innovations in Primary Care
Teens Benefit From a New Primary Care Virtual Driving Assessment Model
Integrating driving support into a primary care setting can address a leading cause of family stress as well as teen adolescent morbidity and mortality. Motor vehicle crashes are a leading cause of death for adolescents, and a leading cause of crashes is driver error. To address this, researchers at the Children’s Hospital of Philadelphia and Perelman School of Medicine at the University of Pennsylvania implemented a 15-minute self-administered virtual driving assessment test in 19 primary care practices. 3,037 adolescents 15 years and older completed the virtual driving assessment from May 2021 through May 2023. Drivers received an evidence-based, educational personalized feedback report identifying risks and areas for targeted practice. 77% of the teens completed a satisfaction survey, agreeing or strongly agreeing they would recommend the virtual assessment to their friends and would like to take the assessment again.
Testing a New Care Model: Implementing a Virtual Driving Assessment in Primary Care
Alexander G. Fiks, MD, MSCE
Children’s Hospital of Philadelphia: The Possibilities Project and Clinical Futures, Philadelphia, Pennsylvania
Department of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Research Brief
Study Examines the Impact of Social Connections and Professional Networks of NAPCRG Members in Driving Scientific Success
Background and Goal: This study marks the 50th anniversary of the North American Primary Care Research Group (NAPCRG)—the premiere primary care research organization, particularly in family medicine—by examining social connections among members.
Study Approach: Researchers used social network analysis to characterize individual members and the relational structure among NAPCRG community members.
The study invited 5,905 current and past NAPCRG members and participants. The survey, based on the validated Program to Analyze, Record, and Track Networks to Enhance Relationships (PARTNER) Tool, assessed engagement, relationships, and benefits derived from NAPCRG involvement.
Main Results:
The survey garnered 906 participants, who identified an additional 815 individuals with whom the participants reported relationships. The NAPCRG social network analysis contained 1,721 total individuals with 5,196 partner relationships.
Participants felt many relationships led to productivity and improved or advanced the field of primary care.
Most relationships (60%) were described as having an integrated level of collaboration.
Many relationships led to a research paper (58%) or a grant (34%).
The NAPCRG annual meeting was the most common mode of participant engagement (91%).
Why It Matters This study underscores the importance of professional networks in driving scientific success and highlights the need for continued support and development of these connections.
Fifty Years of Connection: Characterizing the Social Network of a Primary Care Research Organization
Sarah Gebauer, MD, MSPH, et al
SLUCare Academic Pavilion, Saint Louis University, Saint Louis, Missouri
The Fiftieth Anniversary Planning Committee, NAPCRG, Leawood, Kansas
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
______________________________________________________________________
Original Research
Dutch Version of the Person-Centered Primary Care Measure Survey Demonstrates Sufficient Validity and Sufficient Reliability for Use in Dutch Primary Care Practices
Background and Goal: Person-centered care focuses on treating patients as individuals with unique needs and involving them actively in their care decisions. The Person-Centered Primary Care Measure (PCPCM) is a recently developed, patient-reported survey able to assess person-centeredness. The PCPCM has demonstrated strong validity and reliability. The goal of this study was to translate the original PCPCM survey into Dutch, adapt the survey for people with low literacy, and evaluate its structure, consistency, and accuracy.
Study Approach: The survey was translated into Dutch and then back to English to ensure accuracy. The Dutch version was then tested to make sure it worked well for Dutch-speaking primary care patients, particularly those with low literacy. To confirm that the Dutch version of the survey accurately measured person-centered care, researchers compared it with a relevant selection of questions from another established survey, the Quality of Care Through the Patient’s Eyes (QUOTE) questionnaire. To ensure the Dutch survey’s reliability and consistency in its results, researchers conducted this comparison in a cross-sectional study.
Main Results: A total of 205 patients from four general practices completed the survey. Analysis showed that the survey worked better with three factors: comprehensiveness of care, personal relationship, and contextual care. The survey was found to be reliable in measuring person-centered care. It also showed a strong agreement with the QUOTE survey, indicating it accurately measured person-centered care.
Why It Matters: Validated outcome measures of important constructs such as patient centered care are important for future high quality research relevant to family medicine. Careful validation of translated tools allows for valid international comparisons.
Dutch Translation and Psychometric Evaluation of the Person-Centered Primary Care Measure
Peter Lucassen, MD, PhD, et al
Department of Primary and Community Care, Radboud Institute for Health Services, Radboud University Medical Center, Nijmegen, the Netherlands
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Research Brief
Transforming Clinical Practice Initiative Linked to Reduced Emergency Department Visits
Background and Goal: The Transforming Clinical Practice Initiative was a four-year nationwide program aimed at improving outpatient health care quality. The initiative, funded by the Centers for Medicare & Medicaid Services, also prepared practices for payment systems based on care quality rather than service quantity and included a Change Package to guide practice transformations. This research brief examines whether these transformations were associated with reductions in emergency department visits among both primary and specialty care practices.
Study Approach: Researchers analyzed data from 3,773 practices in the Transforming Clinical Practice Initiative, serving 3.8 million Medicare beneficiaries. They used the Practice Assessment Tool, developed as part of the initiative, to measure progress on various care milestones. Emergency department visit rates before and after these transformations between April 2015 and September 2021 were compared, adjusting for various factors, to determine if improved practice scores were linked to reduced emergency department visits
.
Main Results: By the second follow-up year, a 40-percentage point improvement in the Practice Assessment Tool score was associated with a 6% reduction in emergency department visits for primary care practices and a 4% reduction for specialty care practices. This translates to 31 fewer emergency department visits per 1,000 beneficiaries per year for primary care and 19 fewer for specialty care. For primary care practices, improvements in five specific areas were linked to a reduction in emergency department visits:Population management, measuring and documenting value and quality improvement strategy, behavioral health integration, coordinated care, and enhanced access. For specialty care practices, improvements in two areas—population management and enhanced access—were linked to a reduction in emergency department visits.
Why It Matters: The study shows that comprehensive practice transformation efforts may significantly reduce costly emergency department visits, supporting the Centers for Medicare & Medicaid Services’ goals. A national reduction of 6% in ED visits could save Medicare up to $1.38 billion annually.
Practice Transformation in the Transforming Clinical Practice Initiative and Emergency Department Use
Lori Timmins, PhD, et al
Mathematica, Chicago, Illinois
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
___________________________________________________________________________
Essay
Compassionate Care in Addressing Depression in Older Patients
Background: A physician recounts an experience with an older patient who revealed feelings of purposelessness and a sense of having “overstayed his welcome” despite appearing content. The patient’s depression could have easily been missed with the Patient Health Questionnaire and other widely used clinical tools that may not adequately address the specific needs of an older population.
Key Argument: The author emphasizes the importance of tailored, compassionate approaches to recognize and address geriatric depression. The physician’s experience stresses the need to go beyond quick fixes or conventional treatments to listen and support patients.
Why It Matters: This narrative underscores the need for health care professionals to develop specialized knowledge and approaches for geriatric care. The author emphasizes that compassion, patience, and individualized care are important in addressing the mental health and overall well-being of older patients. The quality of life for older populations can be improved by understanding and addressing these needs.
The Dilemma of Death’s Call
Tamara A. Huson, MD, FAAFP
Bon Secours Mercy Health Physicians, Cincinnati, Ohio
University of Cincinnati, Cincinnati, Ohio
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Innovations in Primary Care
Using Adult Learning Theory Through Scenario-Based Discussion Questions Improves Discussion on Lifestyle Medicine for Healthy Adults
Healthy adults may perceive their wellness exams as an impersonal, mandatory checklist with counseling on lifestyle changes. Over a four-year period, well visits with patients at the University at Buffalo Medical Doctors (UBMD) Family Medicine clinic in Buffalo, New York, implemented scenario-based discussion questions. To make discussions more engaging, clinicians applied adult learning theory, which emphasizes self-directed and goal-oriented learning. For example, patients were asked how they would perform a specific physical task. Their answers allowed them to reflect on their current lifestyle and identify areas for improvement. Using scenario-based discussion questions was found to be a simple and time-efficient way to improve patient engagement and motivation in lifestyle medicine domains during well visits. The discussion questions also increased the patients’ knowledge of requested topics.
Scenario-Based Discussion: Using Adult Learning Theory to Improve Discussion on Lifestyle Medicine for Healthy Adults
Andrew Baumgartner, MD, et al
Department of Family Medicine, Jacobs School of Medicine & Biomedical Sciences, University of Buffalo, Buffalo, New York
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Innovations in Primary Care
Implementing Diabetic Retinopathy Screening Using In-Clinic Retinal Photographs and Automated Software Analysis Increases Screening Rates for Diabetic Retinopathy Among Low-Income Minority Patients
One-third of diabetic adults in the U.S. do not receive annual eye exams. Additionally, lack of pupillary dilation before exams is associated with ungradable, or insufficient exams. In September 2022, the OhioHealth Grant Medical Center Family Medicine practice implemented on-site diabetic retinopathy screening using digital fundus photography and automated retinal imaging without dilation. The practice later introduced eye dilation for specific patients.
By identifying patients needing screening before appointments and using electronic health record reminders, the clinic increased the rate of interpretable exams from 20% in November 2022 to 35% in May 2023. That same month, the clinic began offering eye dilation to patients over 64 years of age and those who failed non-dilated exams. This change reduced the insufficient exam rate from 36% to 22% over the following eight months. The clinic’s retinopathy detection rate increased from 11% to 18% between September 2022 and January 2024. By January 2024, the screening rate was 57% for patients not seen in a year and 65% for those seen within the year.
The greatest increase in retinopathy screening came after clinic managers started tracking patients who needed screening prior to their appointments, and reminding staff through the electronic health record to perform screening. Offering dilated eye exams further reduced the rate of insufficient exams. Overall, the strategy of using in-clinic retinal photographs with software interpretation and selective eye dilation effectively increased screening rates for our patients from socially disadvantaged populations.
Dilation Before Automated Diabetic Retinopathy Screening Performed in the Primary Care Setting
Jonathan Yun, MD, MPH, et al
OhioHealth Grant Family Medicine, Columbus, Ohio
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Essay
A Return to Compassion-Based Measures of Physicians’ Worth is Urgently Needed for Improvement of Population Health and Reduction of Physician Burnout
Background:Physician value is measured today in terms of productivity, volume, finance, outcomes, and cure rates in addition to a vast knowledge base. Prior to the 20th century, physicians were not expected to excel at speed of care. Neither were they recognized for the volume of decisions made in a short period of time. Instead, their work was rooted in their role as “compassionate witnesses.”
Key Argument: Population health and productivity metrics are necessary measurements for health system outcomes. However, these metrics are poor measures of a physician’s full performance and can lead to feelings of inadequacy and loss of purpose.
Why It Matters: A new paradigm for metrics based on traditional understandings of physicians’ value—their ability to compassionately care—can benefit efforts to avert burnout and imposter syndrome. Such a measure could improve patient satisfaction and outcomes, population health, and physician well-being.
What Are Doctors For? A Call for Compassion-Based Metrics as a Measure of Physician Value
Timothy Aaron Zeller, MD, FAAFP, et al
Clemson Rural Health and Clemson University School of Health Research, Clemson, South Carolina
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Research Brief
Sexual and Gender Minority Adults Avoid Necessary Care Due to Identity Discordance with Clinicians and Experiences of Discrimination
Background and Goal: Identity discordance between patients and clinicians is associated with worse self-rated patient experience and less receipt of necessary care. Most prior studies have focused on racial discordance. However, whether these phenomena also apply to sexual and gender minority adults is currently unknown. This study evaluated how prevalent avoidance due to patient-clinician identity discordance is and its potential association with health care discrimination among sexual and gender minority adults.
Study Approach: A cross-sectional analysis was conducted of the National Institutes of Health’s All of Us Research Program. Data were collected from adults aged 18 years or older enrolled between May 2018 and July 2022. Sexual minority, heterosexual, gender minority, and cisgender adults were identified based on responses to interview questions.
Results: After adjusting for sociodemographic characteristics, sexual minority adults were significantly more likely than heterosexual adults to report care avoidance on the basis of patient-clinician identity discordance. Gender minority adults were also more likely to report care avoidance in comparison to cisgender adults. Additionally, median health care discrimination scores were higher among sexual minority and gender minority adults relative to heterosexual and cisgender adults. Among sexual and gender minority adults, higher levels of health care discrimination were significantly associated with a higher prevalence of care avoidance.
Why It Matters: These findings are consistent with emerging qualitative research showing that sexual and gender minority patients prefer clinicians who share similar sexual orientations and/or gender identities. Patient preferences are likely due to a desire for more affirming care and expertise specific to sexual and gender minorities, in addition to perceptions of safety, comfort, and solidarity.
Health Care Discrimination and Care Avoidance Due to Patient-Clinician Identity Discordance Among Sexual and Gender Minority Adults
Michael Liu, MPhil, et al
Harvard Medical School, Boston, Massachusetts
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
Essay
Revitalizing Primary Care: The Benefits of Small, Independent Practices
Background: This essay reflects on the history and evolution of medical practices, focusing on the shift from small, independent practices to large, corporatized systems. The essay points out similarities between small businesses and medical practices, highlighting the personal touch and community-oriented service of independent practices.
Key Argument: The author argues that smaller, independent medical practices offer numerous benefits.The benefits include better communication, higher levels of trust among clinicians and staff, and lower levels of burnout. These practices foster a sense of autonomy and personal accountability, factors that large, corporatized systems often lack. The author advocates for a return to smaller, community-based practices to rejuvenate the primary care field.
Why It Matters: Emphasizing the importance of small, independent practices in primary care can lead to increased physician satisfaction and a stronger sense of community.
The Shoeshine Stand and the Renaissance of Primary Care
John J. Frey III, MD
Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin
PRE-EMBARGO LINK (Link expires at 5 p.m. July 22nd, 2024)
PERMANENT LINK
# # #
Annals of Family Medicine is a peer-reviewed, indexed research journal that provides a cross-disciplinary forum for new, evidence-based information affecting the primary care disciplines. Launched in May 2003, Annals is sponsored by seven family medical organizations, including the American Academy of Family Physicians, the American Board of Family Medicine, the Society of Teachers of Family Medicine, the Association of Departments of Family Medicine, the Association of Family Medicine Residency Directors, the North American Primary Care Research Group, and The College of Family Physicians of Canada. Annals is published six times each year and contains original research from the clinical, biomedical, social and health services areas, as well as contributions on methodology and theory, selected reviews, essays and editorials. Complete editorial content and interactive discussion groups for each published article can be accessed free of charge on the journal’s website, www.AnnFamMed.org.
Media Contact: Julie Hirschhorn
Annals of Family Medicine
jhirschhorn@aafp.org
END