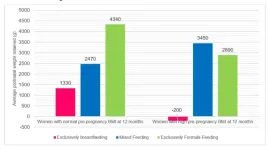
27 August 2024, Singapore – A KK Women’s and Children’s Hospital (KKH) study[1] on breastfeeding practices revealed that among the women who exclusively breastfed, those with high body mass index[2] (BMI) before pregnancy lost more weight than women with a healthy BMI pre-pregnancy.
Women with high BMI who exclusively breastfed, in addition to losing their pregnancy weight, lost an extra 200 grammes on average, 12 months after childbirth. Women with normal BMI who exclusively breastfed lost weight but continued to retain about 1,330 grammes of their postnatal weight during the same period.
Regardless of BMI, all women practising exclusively breastfeeding tended to retain less weight than those who practised mixed feeding or exclusively formula feeding. Refer to Annex A, Figure 1. Most women with normal BMI gain an average of 11 to 16 kilogrammes during pregnancy[3].
Lead author of the study, Dr Loy See Ling, Department of Reproductive Medicine, KKH, said, “In this year-long study, we made an interesting discovery - an additional benefit for women with high BMI. Due to hormonal factors, there is a re-distribution and management of their body fat to the extent that there is an opportunity for them to lose more than the postnatal weight gain.
“This is of particular interest in Singapore where we are facing a rising obesity rate at 10.5 per cent[4] in a year. Encouraging exclusive breastfeeding alongside targeted lifestyle changes may serve as an effective intervention for enhancing the metabolic health of young mothers and their families after childbirth especially if they have high BMI, thus decreasing the likelihood of mother and child developing obesity, diabetes and cardiovascular diseases in the later years.[5]”
Exclusive breastfeeding benefits all mothers
Supported by Tanoto Foundation, the KKH study is the first such study tracking and linking breastfeeding practices with weight loss in an Asian, multi-ethnic population. The study tracked 379 first-time mothers for 12 months after childbirth, and their feeding practices – where the mothers exclusively breastfed, practiced a mix of breast feeding and formula feed, or excusively formula fed.
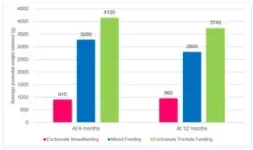
The study revealed that six months after giving birth, women of all BMI who exclusively breastfed retained the least amount of the postnatal weight at approximately 910 grammes. In contrast, women who practiced a mix of breast feeding and formula feeding retained 3,280 grammes, while those who exclusively formula fed retained the most at 4,150 grammes.
These patterns remained consistent at 12 months after childbirth - women of all BMI who exclusively breastfed retained approximately 960 grammes of their postnatal weight, much lower than women who mixed fed their babies (2,800 grammes), and those who exclusively formula fed (3,740 grammes). Refer to Annex A, Figure 2.
Implications of postnatal weight retention in women
Asians are found to have a higher tendency to accumulate abdominal or visceral fat as compared to other populations. This can have a profound impact on the Asian mother’s lifelong health, including metabolic and cardiovascular disease, as well as on subsequent pregnancies and the future health of her child[6],[7].
Dr Loy said, “Postnatal weight retention can also lead to concerns such as stress, anxiety, and depression, especially in Singapore’s culture where there is an emphasis on a rapid return to pre-pregnancy weight. In women with multiple pregnancies, each instance of retained weight can accumulate, resulting in a significant long-term weight increase that can impact pregnancy outcomes and long-term health, thereby increasing the risk of obesity, diabetes and heart diseases[8] for both mother and child.”
Building a Healthier SG with breastfeeding
This study exemplifies the life-course principle of the KKH-led SingHealth Duke-NUS Maternal and Child Health Research Institute (MCHRI), underscoring the benefits of exclusive breastfeeding and its role in optimising health of mothers and children in setting the foundation that will last beyond infancy, through childhood, adolescence into adulthood.
This is the first published study under the Community-enabled Readiness for first 1,000 days Learning Ecosystem (CRADLE) programme funded by Tanoto Foundation[9]. One of the key programmes under the KKH-led MCHRI, CRADLE aims to create a self-learning eco-community that spans from pregnancy to early childhood, to enhance parenting self-efficacy among first-time parents. Started in 2020, the programme involves KKH participants who were randomly assigned to receive (1) standard routine care; (2) behavioural nudges (text messages) along with the use of a social media platform; or (3) midwife-led continuity care involving individualised teleconferencing sessions, during pregnancy and post-delivery.
In the next phase, CRADLE will provide an innovative, sustainable, scientifically-based strategy to help first-time parents enhance their skills in promoting positive child development and behaviours. This will assist to equip children with the right skills and behaviours for preschool.
<Ends>
For more information, please contact:
Angeline Chen
Manager
Corporate Communications
Email: media@kkh.com.sg
About KK Women's and Children's Hospital
KK Women’s and Children’s Hospital (KKH) is Singapore’s largest tertiary referral centre for obstetrics, gynaecology, paediatrics and neonatology. The academic medical centre specialises in the management of high-risk conditions in women and children.
Driven by a commitment to deliver compassionate, multidisciplinary care to patients, KKH leverages research and innovation to advance care. In 2021, the hospital launched the SingHealth Duke-NUS Maternal and Child Health Research Institute (MCHRI) to support the growth of every woman and child to their fullest potential, and transform national heath in the region.
Some of the hospital’s breakthroughs include uSINE®, a landmark identification system for the administration of spinal epidural, the discovery of new genetic diseases like Jamuar Syndrome, and a series of guidelines for women and children to improve population health.
The academic medical centre is also a major teaching hospital for Duke-NUS Medical School, Yong Loo Lin School of Medicine and Lee Kong Chian School of Medicine. In addition, KKH runs the largest specialist training programme for Obstetrics and Gynaecology, and Paediatrics in Singapore.
KKH was founded in 1858 and celebrates its 100th year as a maternity hospital in 2024. For more information, visit www.kkh.com.sg
Follow us on
Facebook | Instagram | LinkedIn | TikTok | YouTube
About SingHealth Duke-NUS Maternal and Child Health Research Institute
The SingHealth Duke-NUS Maternal and Child Health Research Institute (MCHRI) serves as the centre of excellence for women and child health research, to transform and improve national health in Singapore and the region. Taking on a life-course approach to optimise human capital, MCHRI aims to support the growth and development of every woman and child to their fullest potential.
Launched in 2021 at KK Women’s and Children’s Hospital, the Institute seeks to advance reproductive, metabolic and mental health, cognitive developments and cures for cancer and critical diseases, through research with direct impact on patient care, innovation and digital strategies. It will also nurture a pipeline of researchers and establish key partnerships and collaborations, to support value-driven care for Singapore and the region.
About Tanoto Foundation
Tanoto Foundation is an independent philanthropic organisation founded in 1981 by Sukanto Tanoto and Tinah Bingei Tanoto based on the belief that every person should have the opportunity to realise his or her full potential. Tanoto Foundation programmes stem from the belief that quality education accelerates equal opportunity. We harness the transformative strength of education to realise people’s full potential and improve lives. Tanoto Foundation focuses on making an impact in three main areas: improving learning environments, future leader’s development, as well as medical research.
Annex A
Tip for weight loss after childbirth
Breastfeeding burns up to 500 calories in a day, depending on the frequency and duration. The most effective way to lose postnatal weight is by combining exclusive breastfeeding with a balanced and healthy diet and regular exercise. Other benefits of such a healthy lifestyle include improved cardiovascular health, strength, and mental well-being.
The following are some common activities that a woman can do to burn about 500 calories, though the actual calories burned may fluctuate depending on factors such as a woman's age and body composition:
• Brisk walking: ~ 90 minutes
• Running: ~ 45 minutes
• Cycling (moderate): ~ 70 minutes
• Aerobics: ~ 60 minutes
• Swimming (vigorous): ~ 45 minutes
[1] Loy, S.L., Chan, H.G., Teo, J.X., Chua, M.C., Chay, O.M., & Ng, K.C. (2024). Breastfeeding Practices and Postpartum Weight Retention in an Asian Cohort. Nutrients, 16, 2172. https://doi.org/10.3390/nu16132172
[2] High body mass index (BMI) refers to a BMI of ≥ 23 kg/m2
[3] Weight Gain During Pregnancy: What is a Healthy Weight? - HealthXchange.sg
[4] National Population Health Survey 2020
[5] Tambalis, K. D., Mourtakos, S., Panagiotakos, D. B., & Sidossis, L. S. (2018). Association of exclusive breastfeeding with risk of obesity in childhood and early adulthood. Breastfeeding Medicine, 13(10), 602-611. https://doi.org/10.1089/bfm.2018.0117
[6] Lear, S. A., Humphries, K. H., Kohli, S., & Birmingham, C. L. (2007). The use of BMI and waist circumference as surrogates of body fat differs by ethnicity. Obesity, 15(11), 2817-2824. https://doi.org/10.1038/oby.2007.334
[7] Godfrey, K. M., Reynolds, R. M., Prescott, S. L., Nyirenda, M., Jaddoe, V. W. V., Eriksson, J. G., & Broekman, B. F. P. (2017). Influence of maternal obesity on the long-term health of offspring. The Lancet Diabetes & Endocrinology, 5(1), 53-64. https://doi.org/10.1016/S2213-8587(16)30107-3
[8] Ku, C. W., Cheng, T. S., Ku, C. O., Zhou, K. X., Cheung, Y. B., Godfrey, K. M., Han, W. M., Yap, F., Chan, J. K. Y., & Loy, S. L. (2023). Distribution and association of interpregnancy weight change with subsequent pregnancy outcomes in Asian women. Scientific Reports, 13, Article 4834. https://doi.org/10.1038/s41598-023-31947-
END