(Press-News.org) Original Research
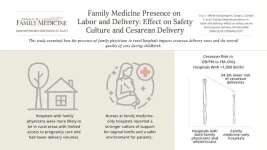
Family Physicians in Rural Hospitals Associated With Lower Cesarean Rates and Safer Maternal Care Culture
Background and Goal: The U.S. is experiencing a maternal health crisis, particularly in rural areas. This issue is compounded by rising rates of severe maternal morbidity and mortality. Family physicians often fill critical gaps in care in rural areas where obstetricians are scarce. This study examined how the presence of family physicians in rural hospitals impacts cesarean delivery rates and the overall quality of care during childbirth.
Study Approach: The study analyzed data from rural hospitals in Iowa and collected survey responses from clinicians about their attitudes and practices related to childbirth. Researchers linked these responses with hospital data on cesarean delivery rates, patient demographics, and other factors. The study compared hospitals where only family physicians provide care, hospitals with both family physicians and obstetricians, and hospitals with only obstetricians.
Main Results: A total of 849 clinicians from 39 hospitals completed the survey: 13 family medicine-only, 11 obstetrician-only, and 15 hospitals with both. All family medicine-only hospitals were rural with fewer than 1,000 annual births.
• Family medicine–only hospitals had a 34.3% lower risk of cesarean deliveries compared to hospitals with both family physicians and obstetricians.
• Nurses at family medicine–only hospitals reported a stronger culture of support for vaginal births and a safer environment for patients.
• Hospitals with family physicians were more likely to be in rural areas with limited access to pregnancy care and had lower delivery volumes.
Why It Matters: The findings of this study suggest that family physicians in rural areas where access to specialized obstetric care is limited contribute to lower cesarean delivery rates and a supportive culture for vaginal births, which are key indicators of maternal care quality.
Family Medicine Presence on Labor and Delivery: Effect on Safety Culture and Cesarean Delivery
Emily White VanGompel, MD, MPH, et al
Department of Family and Community Medicine, University of Illinois at Chicago College of Medicine, Chicago, Illinois
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
____________________________________________________________________________________
Editorial
Family Physicians Play a Vital Role in Improving Maternal Health Outcomes
Background: Pregnancy and childbirth in the U.S. are more dangerous than in any other high-income country, with particularly high risks for Black individuals and those in rural areas. To address this, the American Academy of Family Physicians (AAFP) and the White House have called for expanding and diversifying the perinatal workforce. This includes training family physicians to provide critical pregnancy care, especially in rural and underserved communities.
Key Argument: The editorial calls for policy changes such as health system credentialing to increase family physicians’ involvement in obstetric care and training reforms to prepare the health workforce to improve maternal outcomes. The author asserts that family physicians significantly improve the quality of obstetric care because of their specialized training. Family medicine residencies emphasize interprofessional teamwork, communication, and continuity of care, and frequently include the completion of the AAFP’s Advanced Life Support in Obstetrics (ALSO) course, which improves skills in handling obstetric emergencies. These aspects of their training enable family physicians to foster a strong safety culture and deliver care on par with specialists.
Why It Matters: Family physicians are uniquely trained to lead interprofessional pregnancy care teams that promote a safety culture and improve health outcomes. New training models must diversify the physician workforce and support family physicians’ vital role in improving maternal health outcomes.
Family Medicine Obstetrics: Answering the Call
Wendy B. Barr, MD, MPH, MSCE
Department of Medicine, UMass Chan Lahey Regional Medical Campus, Burlington, Massachusetts
Department of Family Medicine, Tufts University School of Medicine, Boston, Massachusetts
Mario P. DeMarco, MD, MPH
Department of Family Medicine and Community Health, Perelman School of Medicine, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Original Research
Long COVID Patients Seek Better Collaboration With Health Care Professionals
Background and Goal: “Long COVID” is the continuation or development of new symptoms three months after initial SARS-CoV-2 infection. For many patients with long COVID, primary care is the first point of interaction with the health care system. This study aimed to examine the expectations and experiences of primary care patients seeking treatment for long COVID.
Study Approach: Researchers conducted 20 semistructured interviews between 2022 and 2023 with primary care patients from a long COVID triage clinic at the University of Utah. Using a phenomenological framework, the interviews focused on understanding and describing participants’ lived experiences and perceptions through open-ended, flexible questioning. The interviews were analyzed using inductive qualitative content analysis, a method that identifies themes and patterns in the data.
Main Results:
19 interviews were analyzed. Participants averaged 54 years old, and 53% were female. Most participants were infected with COVID-19 for the first time in 2020 (32%) or 2021 (47%).
Patient Expectations: Patients expected their primary care practitioners to be knowledgeable about post-COVID conditions, attentive to their individual condition, and to engage in collaborative processes for treatment.
Patient Experiences: Participants perceived their interactions with practitioners as negative when they felt dismissed or discouraged. Patients also described challenges navigating the fragmented U.S. health care system when coordinating care, treatment and testing, and payment.
Why It Matters: The study results highlight a disconnect between the expectations and experiences of long-COVID patients within the U.S. health care system. Despite facing numerous barriers and frustrations, patients show a desire to collaborate with clinicians to improve treatment outcomes.
Challenges in Receiving Care for Long COVID: A Qualitative Interview Study Among Primary Care Patients About Expectations and Experiences
Elena Gardner, MPH, et al
University of Utah Family and Preventive Medicine, Salt Lake City, Utah
PRE-EMBARGO LINK (Link expires at 5 p.m. August 27th, 2024)
PERMANENT LINK
____________________________________________________________________________
Original Research
Underserved Patients Reduce Blood Pressure and Heart Disease Risk Using Remote Monitoring Program
Background and Goal: Underserved communities are at higher risk for uncontrolled high blood pressure (hypertension), which can lead to heart disease and higher death rates. This study evaluated the impact of a remote monitoring program called DIG IT on blood pressure control in underserved patients at a Federally Qualified Health Center (FQHC) in Orange County, California.
Study Approach: Researchers compared two groups: 70 patients using the DIG IT program, which includes digital blood pressure monitoring, medication management, and a team-based care approach, and a historical control group of 70 patients who received standard care without digital tools. The study focused on patients aged 40 and older with uncontrolled hypertension. Researchers tracked blood pressure readings and heart disease risk scores over three months.
Main Findings:
• Patients in the DIG IT program saw their systolic blood pressure drop by an average of 31 points. This is compared to a reduction of just 15 points in the control group. Diastolic blood pressure decreased by 11 points in the DIG IT group, compared to a 5-point reduction in the control group.
• The program led to a significant reduction in the estimated American College of Cardiology 10-year risk of heart disease. Patients in the DIG IT group showed twice the improvement compared to those in the control group.
• Nearly 73% of patients in the DIG IT program reached their blood pressure goals within three months, compared to 37% in the control group.
Why It Matters: These findings show that remote monitoring programs, like DIG IT, can significantly improve blood pressure control and lower heart disease risks in underserved communities. By connecting digital health tools with real-time care, these programs provide timely interventions crucial for managing chronic diseases.
Digital Innovation to Grow Quality Care Through an Interprofessional Care Team (DIG IT)
Among Underserved Patients With Hypertension
Joyce Y. Lee, PharmD, APh, BCPS, BCACP, CDCES, et al
School of Pharmacy and Pharmaceutical Sciences, University of California, Irvine, California
University of California Irvine Health Family Health Center, Irvine, California
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Systematic Review
High-Sensitivity Troponin Shows Promise in Diagnosing Acute Coronary Syndrome in Primary Care Settings
Background and Goal: Chest pain is a common but challenging symptom for general practitioners to evaluate, as it can be caused by both serious conditions and more benign issues. This study assessed the effectiveness of various risk stratification tools, including clinical decision rules and troponin tests, in helping general practitioners rule out acute coronary syndrome in patients with chest pain.
Study Approach: Researchers conducted a systematic review of studies involving adult patients presenting with chest pain in primary care settings. The review included studies that examined the diagnostic accuracy of different clinical decision rules and troponin point-of-care tests, both conventional and high-sensitivity, in identifying acute coronary syndrome, which includes heart attacks. The study compared these tools to the unaided clinical judgment of general practitioners.
Main Findings: 14 studies were included in the final review.
• Some of the clinical decision rules without troponin improved safety. However, none consistently outperformed unaided general practitioner judgment in ruling out acute coronary syndrome.
• Conventional troponin as a standalone test did not meet the desired diagnostic accuracy, making the tests less reliable in primary care settings.
• High-sensitivity troponin tests demonstrated the highest diagnostic accuracy. However, this finding requires further prospective validation in primary care before it can be recommended for widespread use.
Why It Matters: Although high-sensitivity troponin tests hold promise, they are not yet ready to replace clinical judgment or be used independently in primary care settings without further validation.
Chest Pain in Primary Care: A Systematic Review of Risk Stratification Tools to Rule Out Acute Coronary Syndrome
Simone van den Bulk, MD, et al
Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, The Netherlands
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
______________________________________________________________________________
Original Research
Black, Hispanic/Latine, and Native American Family Physicians Play a Critical Role in the Care of Minority Medicaid Patients
Background and Goal: Underrepresented in Medicine (URiM) physicians are key to better health outcomes for minority patients. However, the proportion of URiM physicians—such as Black, Hispanic/Latine, and Native American physicians—in the U.S. health care system remains low. This study links a unique dataset of information on family physicians’ race and ethnicity to national-level Medicaid claims data to examine the diversity of the family physician workforce caring for Medicaid beneficiaries.
Study Approach: Researchers analyzed data from 13,096 family physicians across 44 states. To do this, they used 2016 Medicaid claims data from the Transformed Medicaid Statistical Information System (T-MSIS) and 2016-17 American Board of Family Medicine certification questionnaire responses. The study examined the diversity of Family Physicians’ Medicaid patient panels and whether the physicians saw at least 150 beneficiaries.
Main Results:
• URiM family physicians, particularly Black and Hispanic/Latine family physicians, are significantly more likely to participate in Medicaid by treating a substantial number of Medicaid patients.
• Black and Hispanic/Latine family physicians were more likely to be core Medicaid providers, defined as seeing at least 150 beneficiaries in 2016.
• The patient panels of URiM family physicians had a much higher proportion of Medicaid beneficiaries from racial and ethnic minorities.
Why It Matters: The findings of this study suggest physician race and ethnicity are correlated with Medicaid participation and emphasize the need to continue efforts to diversify the health care workforce.
A Few Doctors Will See Some of You: The Critical Role of Underrepresented in Medicine (URiM) Family Physicians in the Care of Medicaid Beneficiaries
Anushree Vichare, PhD, MBBS, MPH, et al
Fitzhugh Mullan Institute for Health Workforce Equity, Department of Health Policy and Management, Milken Institute School of Public Health, The George Washington University, Washington, DC
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
____________________________________________________________________________________
Original Research
Study Finds PrEP Use Among Gay and Bisexual Men in Ontario Linked to Higher STI Rates
Background and Goal: Pre-exposure prophylaxis (PrEP) is a preventive medicine that reduces the risk of contracting HIV. There is concern that PrEP use may be associated with an increase in bacterial sexually transmitted infections (STIs) like gonorrhea, chlamydia, and syphilis among men who are gay or bisexual. This study explored the relationship between PrEP use and the rates of bacterial STIs over time.
Study Approach: Researchers used data from the iCruise Study, an online longitudinal study of men who are gay or bisexual or have sex with men, in Ontario from July 2017 to April 2018. The study examined how PrEP use related to the number of self-reported bacterial STIs. Researchers analyzed results from 535 participants who completed a weekly diary survey for up to a three-month study period. The study measured the number of chlamydia, gonorrhea, and syphilis infections per 100 months of participant observation time.
Main Results:
535 participants in the iCruise Study were included in the analysis. Researchers followed participants for a total of 1,623.5 person-months (total time all participants were in the study). About 13.1% (70 participants) reported using PrEP during the study period.
PrEP use was linked to a higher rate of gonorrhea:
The initial analysis suggested that the rate of gonorrhea among PrEP users was four times higher than among non-users., with an incidence rate ratio of 4.00. After conducting a bias analysis to account for potential inaccuracies in self-reported data, the association was less pronounced, with a median incidence rate ratio of 2.36 among PrEP users.
There was no significant increase in the rates of chlamydia or syphilis among PrEP users.
Why It Matters: Individuals who take PrEP are at higher risk for gonorrhea and should be regularly tested and treated to manage this risk effectively. This study highlights the importance of STI testing, risk reduction, and secondary prevention measures.
Self-Reported PrEP Use and Risk of Bacterial STIs Among Ontarian Men Who Are Gay or Bisexual or Have Sex With Men
Nguyen K. Tran, PhD, MPH, et al
Stanford University School of Medicine, Palo Alto, California
Department of Epidemiology and Biostatistics, Drexel University Dornsife School of Public Health, Philadelphia, Pennsylvania
PRE-EMBARGO LINK (Link expires at 5 p.m. August 27th, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Original Research
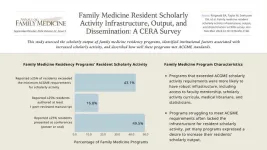
Robust Family Medicine Residency Programs Help Residents Meet Scholarly Output Requirements
Background and Goal: Family medicine residency programs are essential for training future primary care physicians. The Accreditation Council for Graduate Medical Education (ACGME) program requires family medicine residents to perform two scholarly projects. One must be a quality improvement project, and the second project type is at the program's discretion. This study assessed the scholarly activity output of family medicine residency programs in the U.S., identified institutional factors associated with increased scholarly activity, and determined how well these programs meet ACGME standards.
Study Approach: The study surveyed family medicine residency program directors from across the U.S. to gather data on their programs’ scholarly activity. The survey covered various aspects, including the types of scholarly work produced by residents, the availability of resources such as faculty mentorship and access to Institutional Review Boards, and how often residents exceeded the minimum scholarly activity requirements.
Main Results: 298 program directors completed the survey.
• More than half of the program directors reported fewer than 25% of their residents performed more scholarly activity than ACGME minimum requirements.
• The most common forms of scholarly output were letters to the editor, case reports, and population health projects.
• Only 16.9% of programs reported that more than 25% of their residents published peer-reviewed manuscripts. However, 49.6% reported that over 25% of residents presented their work at conferences, with poster presentations being more common than oral presentations.
• Programs that exceeded ACGME scholarly activity requirements were more likely to have robust infrastructure, including access to faculty mentorship, scholarly activity curricula, IRB, medical librarians, and statisticians.
• Programs struggling to meet ACGME requirements often lacked the necessary infrastructure to support resident scholarly activity. However, many programs expressed a desire to increase their residents’ scholarly output.
Why It Matters: Residency programs that provide strong support—such as mentorship, research support, and technical assistance—for increasing scholarly output help residents meet ACGME requirements and prepare them for future challenges in their medical careers.
Family Medicine Resident Scholarly Activity Infrastructure, Output, and Dissemination: A CERA Survey
Bryce A. Ringwald, MD, et al
OhioHealth Riverside Methodist Hospital Family Medicine Residency Program, Columbus, Ohio
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
Original Research
Technology-Assisted Health Coaching Intervention Does Not Improve Weight Loss in Veterans and High-Risk Patients
Background and Goal: Obesity is a significant health issue, particularly among veterans and racial/ethnic minority groups. Primary care is a key setting for addressing obesity. However, many barriers, including time constraints and limited patient engagement, make effective treatment challenging. This study evaluated whether a technology-assisted health coaching intervention called Goals for Eating and Moving (GEM) could help high-risk patients lose weight more effectively than enhanced usual care (EUC).
Study Approach: Researchers conducted a two-arm, cluster-randomized controlled trial involving 19 primary care teams across two health care systems. Patients with obesity or overweight conditions and related comorbidities were randomized to receive either the GEM intervention or EUC. The GEM intervention included one in-person and up to 12 telephone-delivered coaching sessions. Coaches supported goal setting and weight management program engagement, facilitated by a software tool and motivational interviewing. Patients randomized to EUC received educational handouts. The study measured weight changes and other health outcomes over 12 months.
Main Results:
There was no significant difference in weight loss between patients in the GEM intervention and those in EUC at 12 months.
Participants in the GEM group reported a significant increase in weekly physical activity compared to those in the EUC group.
Attendance at weight management programs like MOVE! or DPP did not significantly differ between the GEM and EUC groups.
While more frequent health coaching calls were associated with greater weight loss, overall patient engagement with coaching was low.
Why It Matters: The findings of this study highlight the complexities of managing obesity in high-risk populations and the limitations of relying solely on technology-assisted health coaching in primary care settings.
A Cluster-Randomized Study of Health Coaching for Weight Management in Primary Care
Melanie R. Jay, MD, MS, et al
Department of Medicine, New York University Grossman School of Medicine, New York, New York
Department of Population Health, New York University Grossman School of Medicine, New York, New York
New York Harbor Veterans Health Affairs, New York, New York
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
___________________________________________________________________________
Special Report
The HOMER Study Evolves to Adapt Opioid Treatment Research Amid COVID-19 Challenges
Background and Goal: The HOMER study was launched to determine the most effective setting for starting buprenorphine treatment for opioid use disorder. The study faced challenges including shifts in health care delivery, changes in patient preferences, and the emergence of telehealth. The goal was to adapt the study to these circumstances while maintaining its focus on patient-centered care and effective treatment outcomes.
Key Insights: The HOMER study had to quickly adapt to challenges brought on by the COVID-19 pandemic. With community input, the study design evolved to include a third arm, telehealth, in response to the rapid shift in health care delivery methods. As the study progressed, it became clear that both patients and clinicians had strong preferences for specific induction methods. This led to shifting from a purely randomized approach to a comprehensive cohort design, allowing the study to accommodate patients who preferred not to be randomized. Despite numerous challenges, as of January 2024, HOMER has enrolled nearly 300 study participants, and practices are still participating.
Why It Matters: The experiences and adaptations of the HOMER study show how research can remain resilient and responsive in the face of unforeseen challenges and keep studies relevant and patient-centered.
The Odyssey of HOMER: Comparative Effectiveness Research on Medication for Opioid Use Disorder During the COVID-19 Pandemic
Linda Zittleman, MSPH, et al
University of Colorado Department of Family Medicine, Aurora, Colorado
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
______________________________________________________________________________
Research Brief
Lack of Knowledge About Antibiotic Risks Leads Some Patients to Expect Antibiotics for Common Symptoms
Background and Goal: Patient expectations of receiving antibiotics for common symptoms can trigger unnecessary use, contributing to antibiotic resistance and other health risks. This study examined the prevalence of and factors that influence patient antibiotic expectations for common symptoms.
Study Approach: This study surveyed 564 primary care patients in Texas between January 2020 and June 2021 across public and private clinics. The survey assessed patients’ expectations for antibiotics when experiencing five common symptoms—diarrhea, sore throat, cold/flu, sinus infections, and bronchitis—and their knowledge of the risks associated with antibiotic use. Researchers also examined how health literacy affected these expectations.
Main Results: Over 93% of the patients surveyed expected antibiotics for at least one of the five common symptoms. Public clinic patients were nearly twice as likely to expect antibiotics for sore throat, diarrhea, and cold/flu compared to those in private clinics. Higher expectations for receiving antibiotics for diarrhea and cold/flu symptoms was linked to lack of knowledge about the potential risks of antibiotics. Patients with lower education levels and inadequate health literacy were more likely to expect antibiotics for diarrhea.
Why It Matters: To reduce unnecessary antibiotic use, future efforts should educate patients on when antibiotics are truly needed and emphasize potential risks.
Lack of Knowledge of Antibiotic Risks Contributes to Primary Care Patients’ Expectations of Antibiotics for Common Symptoms
Lindsey A. Laytner, PhD, MPH, et al
Department of Family and Community Medicine, Baylor College of Medicine, Houston, Texas
Center for Innovations in Quality, Effectiveness, and Safety, Michael E. DeBakey Veterans Affairs Medical Center, Houston, Texas
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
___________________________________________________________________________
Research Brief
Using Transparent Capsules in Dry Powder Inhalers Could Significantly Improve Medication Delivery
Background and Goal: This study examined whether patients with non-reversible chronic airway disease using a transparent capsule in single-dose dry powder inhalers affects the amount of medication delivered. The goal was to determine if patients who use transparent capsules that allow them to see if the medication has been fully inhaled have better inhalation results compared to those using opaque capsules.
Study Approach: Researchers conducted an observational cross-sectional study between October 2020 and October 2022 at a tertiary university hospital. The study involved 91 patients using long-acting bronchodilators with single-dose dry powder inhalers for chronic airway disease. Patients used their inhalers under supervision, and the weight of the capsule was measured before and after inhalation to assess how much of the medication was delivered.
Main Results:
• Patients using transparent capsules had a significant decrease in capsule weight after inhalation, with a 30.1% reduction compared to an 8.6% reduction for opaque capsules, indicating more medication was delivered.
• The change in capsule weight was consistent regardless of the severity of the patient’s airway disease.
Why It Matters: The findings suggest that using transparent capsules in dry powder inhalers could improve medication delivery by providing patients with visual feedback on their inhalation technique. This could lead to better management of chronic airway diseases by ensuring that patients receive their full dose of medication.
Evaluation of the Importance of Capsule Transparency in Dry Powder Inhalation Devices
Jose Luis López-Campos, MD, et al=
Unidad Médico-Quirúrgica de Enfermedades Respiratorias. Instituto de Biomedicina de Sevilla (IBiS), Hospital Universitario Virgen del Rocío/ Universidad de Sevilla, Seville, Spain
Centro de Investigación Biomédica en Red de Enfermedades Respiratorias (CIBERES). Instituto de Salud Carlos III, Madrid, Spain
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
______________________________________________________________________________
Essay
Trust and Teamwork Kept This Physician from Walking Away
Background: Family medicine often takes an emotional toll on physicians as they share in the distress and trauma of their patients. This essay recounts a moment when a family physician, overwhelmed by the complexities of patient care, felt ready to walk away from her duties.
Key Argument: The essay highlights the important role of trust and teamwork in health care settings and the strength that health care professionals can draw from one another in moments of vulnerability.
When the physician reached out to a team nurse for support, the nurse’s encouragement helped her regain focus and continue caring for her patients.
Why It Matters: This story illustrates how the emotional support and solidarity within health care teams can be a powerful antidote to burnout, helping professionals navigate the challenges of patient care.
The Day I Almost Walked Away: Trust, Gratitude, and the Power of Teamwork
Colleen T. Fogarty, MD, MSc, et al
Department of Family Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York
University of Rochester Medical Center, Rochester, New York
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
An accompanying episode of the Annals of Family Medicine podcast, featuring Dr. Fogarty and Ms. Schiano, RN, reading their essay aloud, will be available at 5 p.m. on Sept. 23 here.
_____________________________________________________________________________________
Essay
Adding “Contiguity” as a Fifth Core Tenet: The Value of Face-to-Face Care Between Patient and Clinician
Background: In the early 1990s, Barbara Starfield identified four core tenets of primary care: first contact, comprehensiveness, coordination, and continuity. However, in today’s rapidly advancing digital world, telehealth and artificial intelligence are becoming more prevalent, causing the role of physical presence in patient care to be questioned.
Key Argument: This essay argues for the addition of a fifth tenet, “contiguity,” the physical proximity between a patient and their clinician. Face-to-face interactions are essential for building trust, conducting thorough physical exams, and fostering genuine relationships. The essay contends that although technology can improve many aspects of care, it cannot replace the human connection that occurs when patients and clinicians are physically present with one another.
Why It Matters: As health care continues to evolve with digital innovations, it’s important to name contiguity as a core tenet of primary care and articulate the value of physical face-to-face interactions in primary care. Contiguity ensures care remains deeply personal, trusting, and empathic.
Face-to-Face Relationships Still Matter in a Digital Age: A Call for a 5th C in the Core Tenets of Primary Care
Jennifer Y. C. Edgoose, MD, MPH, et al
Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
_______________________________________________________________________________
Innovations in Primary Care
EHR Messaging Before First Visit Fosters a Stronger Patient-Physician Connection
Inspired by the VA’s My Life, My Story project, this initiative used the Electronic Health Record (EHR) to strengthen the patient-physician relationship. The initiative invited patients to share personal narratives before their first visit with a new primary care physician. Conducted at a regional clinic affiliated with the University of Wisconsin-Madison, the project involved sending secure messages to patients, asking them to describe what they wanted their health care team to know about them as a person. The majority of patients responded positively. Some shared deeply personal information they may not have disclosed during a typical clinical encounter. The study physician reported these narratives fostered a stronger connection with patients, facilitated more effective agenda-setting, and improved the overall efficiency of the visit.
Using the Electronic Health Record to Facilitate Patient-Physician Relationship While Establishing Care
Samantha Barbour, et al
University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Innovations in Primary Care
Boston Clinic’s Embedded Neuropsychological Program Helps Immigrants Qualify for Crucial Naturalization Form
To improve access to specialized disability assessments for U.S. citizenship applicants with cognitive and psychiatric conditions, a primary care clinic at Boston Medical Center’s Immigrant and Refugee Health Center implemented an innovative embedded neuropsychological assessment program. This program supports primary care providers by offering specialized evaluations for patients seeking a Medical Certification for Disability Exception (Form N-648), which is necessary for naturalization if the applicant seeks an exception from demonstrating English language proficiency and U.S. history and civics knowledge. The initiative included cognitive screening tools, direct referrals for neuropsychological assessments, and a multidisciplinary team approach. Over two years, the program provided crucial assessments to 34 patients, with 36% qualifying for N-648 forms through specialized testing despite initially normal cognitive screenings. This innovation highlights the value of integrating neuropsychological services within primary care.
Improving Access to Disability Assessment for US Citizenship Applicants in Primary Care: An Embedded Neuropsychological Assessment Innovation
Joelle T. Taknint, PhD, et al
Boston University Chobanian & Avedisian School of Medicine, Boston, Massachusetts
Immigrant & Refugee Health Center, Boston Medical Center, Boston, Massachusetts
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
___________________________________________________________________________________
Innovations in Primary Care
Collaborative Program Between University and Clinic Boosts General Practitioner Recruitment in Deprived Areas of Yokohama, Japan
The “Deep End Kawasaki/Yokohama” program in Japan addresses the critical challenge of recruiting and retaining general practitioners in resource-deprived areas. Launched in 2023 in a socially deprived district of Yokohama, the program establishes a collaboration between a local clinic and a university, creating a partnership that increases the number of general practitioners from one to eight, enhancing clinical care, education, and research opportunities. The program also includes community engagement activities for medical students and trainees to foster empathy and diverse perspectives. The initiative demonstrates a sustainable approach to improving health care delivery in underserved areas and offers a potential model for similar programs in other countries.
Deep End Kawasaki/Yokohama: A New Challenge for GPs in Deprived Areas in Japan
Makoto Kaneko, MD, MClinSci, PhD, et al
Department of Health Data Science, Yokohama City University, Yokohama, Japan
Yokohama Kotobuki-cho Health and Welfare Exchange Center Clinic, Yokohama, Japan
PRE-EMBARGO LINK (Link expires at 5 p.m. September 23rd, 2024)
PERMANENT LINK
END
September/October Annals of Family Medicine Tip Sheet
2024-09-23
ELSE PRESS RELEASES FROM THIS DATE:
Risk model identifies advanced cancer trial patients at highest risk for acute care use
2024-09-23
Investigators from the SWOG Cancer Research Network have developed and validated a risk prediction model for identifying which patients with advanced cancer who are enrolled to clinical trials are at highest risk for unplanned emergency room (ER) visits and hospital stays.
Determining which patients are at significantly higher risk could inform interventions to reduce the need for such visits, improving care quality and reducing costs.
The work will be delivered as an oral presentation by Dawn L. Hershman, MD, MS, at the 2024 ASCO Quality Care Symposium, which will ...
Robust family medicine residency programs help residents meet scholarly output requirements
2024-09-23
Background and Goal: Family medicine residency programs are essential for training future primary care physicians. The Accreditation Council for Graduate Medical Education (ACGME) program requires family medicine residents to perform two scholarly projects. One must be a quality improvement project, and the second project type is at the program's discretion. This study assessed the scholarly activity output of family medicine residency programs in the U.S., identified institutional factors associated with increased scholarly ...
Using transparent capsules in dry powder inhalers could significantly improve medication delivery
2024-09-23
Background and Goal: This study examined whether patients with non-reversible chronic airway disease using a transparent capsule in single-dose dry powder inhalers affects the amount of medication delivered. The goal was to determine if patients who use transparent capsules that allow them to see if the medication has been fully inhaled have better inhalation results compared to those using opaque capsules.
Study Approach: Researchers conducted an observational cross-sectional study between October 2020 and October ...
Family physicians in rural hospitals associated with lower cesarean rates and safer maternal care culture
2024-09-23
Background and Goal: The U.S. is experiencing a maternal health crisis, particularly in rural areas. This issue is compounded by rising rates of severe maternal morbidity and mortality. Family physicians often fill critical gaps in care in rural areas where obstetricians are scarce. This study examined how the presence of family physicians in rural hospitals impacts cesarean delivery rates and the overall quality of care during childbirth.
Study Approach: The study analyzed data from rural hospitals in Iowa and collected survey responses from clinicians about their attitudes and practices related to ...
Long COVID patients seek better collaboration with health care professionals
2024-09-23
Background and Goal: “Long COVID” is the continuation or development of new symptoms three months after initial SARS-CoV-2 infection. For many patients with long COVID, primary care is the first point of interaction with the health care system. This study aimed to examine the expectations and experiences of primary care patients seeking treatment for long COVID.
Study Approach: Researchers conducted 20 semistructured interviews between 2022 and 2023 with primary care patients from a ...
EHR messaging before first visit fosters a stronger patient-physician connection
2024-09-23
Inspired by the VA’s My Life, My Story project, this initiative used the Electronic Health Record (EHR) to strengthen the patient-physician relationship. The initiative invited patients to share personal narratives before their first visit with a new primary care physician. Conducted at a regional clinic affiliated with the University of Wisconsin-Madison, the project involved sending secure messages to patients, asking them to describe what they wanted their health care team to know about them as a person. The majority of patients responded ...
SETI AIR announces Cosmic Consciousness residency recipients
2024-09-23
September 23, 2024, Mountain View, CA – The SETI Institute's AIR program announced the recipients of its Cosmic Consciousness residency for mid-career and emerging artists:
Open (Mid-Career) category: The recipients are the artist team of Bart Kuipers, Julie Michele Morin, and daniela brill estrada, with their project Exoplanet Poetry. The artists plan to create a book of poems using an AI trained on chemical data from imagined extraterrestrial sources. The book will be presented as a multi-sensory chemical experience, making ...
Australian crater could offer fresh insight into Earth’s geological history
2024-09-23
A probable crater stretching more than 370 miles, or 600 kilometers, across the heart of Australia could reshape our understanding of Earth’s geological history.
Researcher Daniel Connelly and Virginia Commonwealth University’s Arif Sikder, Ph.D., believe they have found evidence to support the existence of MAPCIS – the Massive Australian Precambrian-Cambrian Impact Structure -– which is a nonconcentric complex crater that could provide new insights into the geological and biological evolution of our planet.
“Working on the MAPCIS project has been an incredible journey,” said Sikder, an associate professor in the Center for ...
New study raises questions about validity of standard model of solar flares
2024-09-23
Solar flares are extremely intense events that occur in the Sun’s atmosphere, lasting anywhere from a few minutes to several hours. According to the standard flare model, the energy that triggers these explosions is transported by accelerated electrons that hurtle from the magnetic reconnection region in the corona to the chromosphere. As the electrons collide with the chromospheric plasma, they deposit their energy in the plasma, which is heated and ionized as a result. They also cause intense radiation in several ...
Paving the way for new treatments
2024-09-23
A University of Missouri researcher has created a computer program that can unravel the mysteries of how proteins work together — giving scientists valuable insights to better prevent, diagnose and treat cancer and other diseases.
Jianlin “Jack” Cheng from Mizzou’s College of Engineering and his student, Nabin Giri, have developed a tool called Cryo2Struct that uses artificial intelligence (AI) to build the three-dimensional atomic structure of large protein complexes, work recently published in Nature Communications. ...