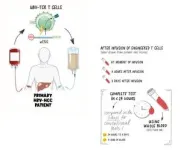
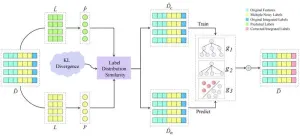
T cells are a type of immune cell that seeks out and destroys cells infected by viruses, bacteria as well as tumour cells. Originally designed to detect SARS-CoV-2-specific T cells, this technology has now been adapted for use in cancer immunotherapy applications. The test, which uses less than a quarter teaspoon of blood, works by stimulating the target T cells in the blood to release chemical signals, called cytokines, through which the quantity and quality of the target T cells can be measured.
In this proof-of-concept study, which was published in Immunotherapy Advances, the research team introduced fragments, called peptides, that stimulate the T cells engineered to fight Hepatitis B virus-related liver cancer present in the treated patients. Using their test, they assessed whether the engineered T cells remained in the blood and continued to function properly after infusion into the patient.
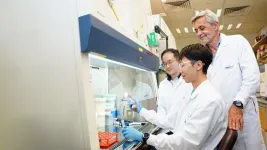
Assistant Professor Anthony Tan, from Duke-NUS’ Emerging Infectious Diseases Programme and first author of the study, commented:
“Our innovative test enables us to swiftly detect and analyse engineered T cells in patient blood samples. Its simplicity and speed could have a significant impact on the clinical field helping to make advanced treatments more accessible.”
With engineered T-cell therapies becoming more widely used to treat malignancies, including Hepatitis B virus-induced liver cancer and a range of blood cancers, being able to accurately and easily track how these engineered cells behave in the body over time will be crucial in monitoring the effectiveness of these therapies in individual patients.
At the same time, this plug-and-play concept can help accelerate the translation of new T-cell-based therapies from the laboratory to patient bedside. The research team has already demonstrated that the test can be adapted for use in numerous viral infections, but this is their first foray into cancer therapies, where the test can be harnessed for T-cell receptor (TCR) engineered T cells, as well as chimeric antigen receptor (CAR) T-cell therapies.
Professor Antonio Bertoletti, from Duke-NUS Emerging Infectious Diseases Programme and senior author of the study, added:
“Tracking the functionality of adoptively transferred engineered T-cell products could provide important information on treatment efficacy over time, an assessment which at the moment remains largely unexplored. We hope that with this proof-of-concept, we can help accelerate research into other CAR and TCR T-cell therapies as well as support clinicians on the frontline caring for patients receiving these novel therapies.”
In collaboration with Lion TCR Pte Ltd, the test has been deployed in a Hepatitis B virus-TCR T-cell therapy clinical trial, called the SAFE-T-HBV trial, evaluating the effectiveness of a novel therapy in two patients and demonstrating the test’s impact on improving the precision of immunotherapy outcomes.
The team is now looking to advance this proof-of-concept through larger clinical studies.
Professor Patrick Tan, Senior Vice-Dean for Research at Duke-NUS, said that he sees potential in the new test. He added:
“This innovation isn’t just a step forward in cancer therapy, it’s a significant advancement in patient care that could extend across multiple diseases. By offering clinicians real-time data on the functionality of these engineered T cells, we are paving the way for highly personalised treatment strategies that could significantly enhance patient outcomes.”
As a leader in biomedical research, Duke-NUS combines basic scientific research with translational applications to innovate treatments approaches and diagnostic tools to advance health globally.
This research is supported by the Singapore Ministry of Health through the National Medical Research Council (NMRC) Office, MOH Holdings Pte Ltd under the NMRC Singapore Translational Research Investigator Award (MOH-000019). The SAFE-T-HBV clinical trial was sponsored by Lion TCR Pte Ltd.
###
DOI: 10.1093/immadv/ltae007
About Duke-NUS Medical School
Duke-NUS is Singapore’s flagship graduate-entry medical school, established in 2005 with a strategic, government-led partnership between two world-class institutions: Duke University School of Medicine and the National University of Singapore (NUS). Through an innovative curriculum, students at Duke-NUS are nurtured to become multi-faceted ‘Clinicians Plus’ poised to steer the healthcare and biomedical ecosystem in Singapore and beyond. A leader in ground-breaking research and translational innovation, Duke-NUS has gained international renown through its five Signature Research Programmes and ten Centres. The enduring impact of its discoveries is amplified by its successful Academic Medicine partnership with Singapore Health Services (SingHealth), Singapore’s largest healthcare group. This strategic alliance has led to the creation of 15 Academic Clinical Programmes, which harness multidisciplinary research and education to transform medicine and improve lives.
For more information, please visit www.duke-nus.edu.sg
About the National Medical Research Council (NMRC)
The NMRC was established in 1994 to oversee research funding from the Ministry of Health and support the development and advancement of biomedical research in Singapore, particularly in the public healthcare clusters and medical schools. NMRC engages in research strategy and planning, provides funding to support competitive research grants and core research enablers, and is responsible for the development of clinician scientists through awards and fellowships. The council’s work is supported by the NMRC Office which is part of MOH Holdings Pte Ltd. Through its management of the various funding initiatives, NMRC promotes healthcare research in Singapore, for better health and economic outcomes.
For media enquiries, please contact:
Brandon Raeburn
Communications & Strategic Relations
Duke-NUS Medical School
braeburn@duke-nus.edu.sg
+65 97768496
END