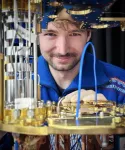
For decades, scientists across the globe have investigated methods to accurately measure drug permeability across the blood-brain barrier, a compact layer of cells that protect the brain from potentially dangerous substances and microbes. They struggled with a number of parameters, such as blood flow and binding to plasma proteins, which were shown to impact permeability in different ways.
In research published in the December 2024 issue of Fluids and Barriers of the CNS (“Brain endothelial permeability, transport and flow assessed over 10 orders of magnitude using the in situ brain perfusion technique”), Quentin R. Smith, Ph.D., from the Department of Pharmaceutical Sciences at the Texas Tech University Health Sciences Center (TTUHSC) Jerry H. Hodge School of Pharmacy, sought to reconcile discrepancies in the field and provide accurate methods for measuring permeability over a very broad range spanning from poorly crossing polar compounds (compounds with a positive or negative charge) to rapidly crossing approved central nervous system (CNS) clinical drugs.
Fluids and Barriers of the CNS is the flagship journal for the blood-brain barrier field, with a journal impact factor of 5.9, placing it in the top 5-6% of all journals. During the journal’s manuscript review, the paper was described as “game changing” and “…clearly the most important manuscript for anyone that considers themselves studying drug delivery in vivo (in a living organism).”
Smith’s team for the project included Haritha Mandula, Ph.D., Jagan Mohan R. Parepally, Ph.D., Fancy Thomas, Ph.D., Helen R. Thorsheim, Ph.D., Abraham J. Al‐Ahmad, Ph.D., and Thomas J. Abbruscato, Ph.D., all from the TTUHSC Department of Pharmaceutical Sciences; Jun Oki, Ph.D., from the TTUHSC Department of Pharmaceutical Sciences and the National Institute on Aging; Per Ask, Ph.D., from Linköping University (Linköping, Sweden); David S. Hage, Ph.D., from the University of Nebraska-Lincoln; and Peter J. Robinson, Ph.D., from the National Institute on Aging.
Smith, who began studying the blood-brain barrier in 1981 while working at the National Institutes of Health, said there had been much confusion in the field regarding the ability of drugs to cross the vasculature of the brain, which for many agents is highly restrictive and forms the core of what is termed the “blood-brain barrier.” Controversy grew regarding how best to accurately assess barrier permeability, distinct from factors such as blood flow and plasma protein binding, which greatly influence brain uptake, particularly for more lipophilic agents (those which dissolve in lipids or fats), which includes the great majority of drugs currently used in treating CNS disorders.
“Researchers were questioning how best to measure permeability, and no single approach at that time gave a clear answer,” Smith said. “Some scientists reverted to just the simplest measurement, such as the brain/blood concentration ratio. But there was no broad agreement on permeability, particularly for agents in the higher realm of lipid solubility, that includes most clinical agents. Our view was to go back and very systematically develop a highly robust model and data set, allowing one to very carefully determine permeability, adjusting and mathematically incorporating the contributions of blood flow and intravascular binding, as well as other factors. The results were striking, providing values 10, 100 and 500 times greater than prior estimates.”
The project team evaluated 120 compounds, revealing that many current CNS drugs permeate the barrier and equilibrate in the brain in less than 10 minutes. The findings challenged previous literature and demonstrated that the equilibration rate for a significant number of CNS drugs is much greater than previously realized.
“We showed that many of the drugs that are used and approved for CNS uptake go into the brain quite well,” Smith said. “They’ve gone through the FDA (Food and Drug Administration) approval process, and they’ve been selected essentially for their ability to get past the blood-brain barrier. A good number of agents in the benzodiazepine, antidepressant, antipsychotic, stimulant and antiepileptic drugs go in as quickly as the blood flow can deliver them. It’s amazingly rapid. For such agents, we had to have extremely accurate measurement of cerebral blood flow.”
The project also highlighted the role of plasma proteins which, for many lipophilic agents can serve an additional brain delivery role beyond that of free drug in plasma. In effect, plasma-bound drugs can dissociate to maintain the intervascular free drug concentration, which otherwise would show rapid depletion under conditions of higher extraction (50-99%). Smith said Valium is a good example of a drug that shows this behavior. Under condition of rapid uptake, Valium from the plasma protein-bound pool can redistribute to maintain free levels to sustain uptake some 10-20-fold greater than that allowed by the free pool alone.
“Our data explained findings from many prior studies where the role of the protein-bound drug had been in question,” Smith said. “With our new model, the findings provide a simple answer consistent across the field. It really was quite exciting to have these ‘aha’ moments where everything comes together, and you say to yourself, ‘Oh, that’s how it all works.’”
One example where the new model provides valuable insight is in the urgent treatment of repetitive epileptic seizures. When a patient experiences a series of seizures in rapid succession, it’s extremely hard on the brain, causing some cells to overwork and burn out. Smith said the treatment of this condition is a medical emergency where literally “time is brain,” so physicians want an agent with a simple administration format that stops the seizures as quickly as possible.
During the development of such products, there was significant discussion over which agent exhibited the greatest brain permeability. Smith’s team studied many of the agents used in the treatment of this condition, and they found that most had very high values in their model. In terms of rapid attainment of therapeutic levels, Smith said other factors may well be of greater importance, including the administration site and how rapid absorption is from such sites under real world conditions in the field. The results also have important implications for conditions of low brain blood flow, such as in ischemic stroke or brain bleeds.
“There are a number of discrepancies in the literature, and we show how those got going,” Smith said. “The entire data set gives a linear relation for permeability that holds over 10 orders of magnitude in solute lipid solubility. We also found a strong inverse relationship with drug size that was highly statistically significant. Overall, we accounted for more than 95% of the variability in the data from drugs that cross the blood-brain barrier by passive diffusion.”
The study also looked at those compounds that do not go into the brain well. This is often because the compound is polar or highly charged. In addition, a significant number of biological compounds are transported out of the brain by active efflux transporters. These efflux transporters have a very important role. Scientists have speculated on the fraction of drugs that cross the barrier well. Most current estimates say 95-99% are kept out, though Smith suspects the actual number is lower — maybe 65-80%.
Smith said he has learned so much during his 50-plus years of working in science. He expects that 30 years from now, the blood-brain barrier field will be far ahead of what is known today.
“That is one of the great pleasures of being a scientist,” Smith said. “We get a front row seat in a movie showing how life works and what are the critical factors behind many things. And we are so proud that this work is fostered and supported by TTUHSC. The totality of the biomedical advances is truly amazing.”
###
END