The researchers at the Icahn School of Medicine at Mount Sinai found that activities like brisk walking or aerobic exercise can lead to measurable improvements in mental well-being, regardless of pain levels or history of anxiety or depressive disorders. Their findings were reported in the February 26 online issue of the Journal of Pain Research.
CPPDs affect millions of women worldwide, leading to increased health care costs, reduced quality of life, and a higher risk of anxiety and depression, yet effective management strategies remain limited. This study highlights the potential of physical activity as a simple and accessible way to enhance mental well-being, say the investigators.
"Chronic pelvic pain disorders are incredibly complex and burdensome for those affected, yet we still have very few effective treatment strategies," says lead corresponding author Ipek Ensari, PhD, an Assistant Professor in the Windreich Department of Artificial Intelligence and Human Health at the Icahn School of Medicine and a member of the Hasso Plattner Institute of Digital Health at Mount Sinai. "Our research suggests that physical activity could be an important tool for improving mental health in these patients, offering them a proactive way to enhance their well-being."
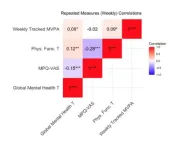
The study tracked 76 women with CPPDs over 14 weeks using mobile health technology, collecting more than 4,200 days’ worth of data. Participants reported their mental health, physical functioning, and pain levels weekly via an app (ehive), while Fitbit devices recorded their daily physical activity. The researchers used advanced statistical modeling to analyze how movement patterns influenced mental health outcomes over time.
One key finding was that the benefits appear to accumulate over time rather than provide immediate relief. "We were particularly intrigued to find that the positive effects of exercise seem to lag by a few days, meaning the mental health benefits may build up gradually," says Dr. Ensari. "This insight is vital for both patients and health care providers, as it underscores the importance of consistency in physical activity."
Beyond its implications for patient care, the study also highlights the growing role of artificial intelligence and mobile health technologies in chronic disease management.
"This study showcases the power of wearable technology and AI-driven analysis to uncover valuable insights about health and behavior in real time," says Girish N. Nadkarni, MD, Chair of the Windreich Department of Artificial Intelligence and Human Health at the Icahn School of Medicine, Director of the Hasso Plattner Institute for Digital Health, Irene and Dr. Arthur M. Fishberg Professor of Medicine, and Director of The Charles Bronfman Institute for Personalized Medicine. Dr. Nadkarni is also the inaugural System Chief of the Division of Data-Driven and Digital Medicine within Mount Sinai’s Department of Medicine and Co-Director of the Mount Sinai Clinical Intelligence Center. “By using innovative data modeling techniques, we can better understand how lifestyle factors like physical activity interact with health conditions and pave the way for more personalized treatment approaches."
While the findings are encouraging, the researchers emphasize that physical activity should not be viewed as a replacement for medical treatment but rather as a complementary strategy. Future research will explore how different types and intensities of exercise impact mental health, pain, and fatigue, with the ultimate goal of developing personalized interventions using wearable technology and mobile apps.
The paper is titled “Trajectories of mHealth-tracked mental health and their predictors in female chronic pelvic pain disorders.”
The remaining authors, all with the Icahn School of Medicine except where indicated, are Emily L. Leventhal, BA: Nivedita Nukavarapu, PhD; Noemie Elhadad, PhD (Columbia University Irving Medical Center); Suzanne R. Bakken, PhD, RN, FAAN, FACMI, FIAHSI (Columbia University School of Nursing); Michal A. Elovitz, MD; Robert P. Hirten, MD; Jovita Rodrigues, MS; Matteo Danieletto, PhD; and Kyle Landell, BA.
The study was supported by a grant award from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (R01HD108263). In addition, this research was supported by T32 grant 5T32GM146636.
-####-
About Mount Sinai's Windreich Department of AI and Human Health
Mount Sinai’s Windreich Department of AI and Human Health, the first of its kind in a U.S. medical school, is leading the charge to revolutionize the intersection of artificial intelligence and human health. The department is committed to leveraging AI in a responsible, effective, equitable, and safe manner to transform research, clinical care, education, and operations. By bringing together world-class AI expertise, cutting-edge infrastructure, and unparalleled computational power, the department is advancing breakthroughs in multi-scale, multimodal data integration while streamlining pathways for rapid testing and translation into practice.
The department benefits from dynamic collaborations across Mount Sinai, including with the Hasso Plattner Institute for Digital Health at Mount Sinai—a partnership between the Hasso Plattner Institute for Digital Engineering in Potsdam, Germany, and the Mount Sinai Health System—which complements its mission by advancing data-driven approaches to improve patient care and health outcomes.
At the heart of this innovation is the renowned Icahn School of Medicine at Mount Sinai, which serves as a central hub for learning and collaboration. This unique integration enables dynamic partnerships across institutes, academic departments, hospitals, and outpatient centers, driving progress in disease prevention, improving treatments for complex illnesses, and elevating quality of life on a global scale.
In 2024, the Department's innovative NutriScan AI application, developed by the Mount Sinai Health System Clinical Data Science team in partnership with Department faculty, earned Mount Sinai Health System the prestigious Hearst Health Prize. NutriScan is designed to facilitate faster identification and treatment of malnutrition in hospitalized patients. This machine learning tool improves malnutrition diagnosis rates and resource utilization, demonstrating the impactful application of AI in health care.
For more information on Mount Sinai's Windreich Department of AI and Human Health, visit: ai.mssm.edu
About the Hasso Plattner Institute at Mount Sinai
At the Hasso Plattner Institute for Digital Health at Mount Sinai, the tools of data science, biomedical and digital engineering, and medical expertise are used to improve and extend lives. The Institute represents a collaboration between the Hasso Plattner Institute for Digital Engineering in Potsdam, Germany, and the Mount Sinai Health System.
Under the leadership of Professor Lothar Wieler, a globally recognized expert in public health and digital transformation, the shared goal is to drive innovations that have a positive impact on the lives of patients, while transforming how people think about their personal health and health systems.
The Hasso Plattner Institute for Digital Health at Mount Sinai receives generous support from the Hasso Plattner Foundation. Current research programs and machine learning efforts focus on improving the ability to diagnose and treat patients.
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the eight- member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to New York City’s large and diverse patient population.
The Icahn School of Medicine at Mount Sinai offers highly competitive MD, PhD, MD-PhD, and master’s degree programs, with enrollment of more than 1,200 students. It has the largest graduate medical education program in the country, with more than 2,600 clinical residents and fellows training throughout the Health System. Its Graduate School of Biomedical Sciences offers 13 degree-granting programs, conducts innovative basic and translational research, and trains more than 500 postdoctoral research fellows.
Ranked 11th nationwide in National Institutes of Health (NIH) funding, the Icahn School of Medicine at Mount Sinai is among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges. More than 4,500 scientists, educators, and clinicians work within and across dozens of academic departments and multidisciplinary institutes with an emphasis on translational research and therapeutics. Through Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai.
-------------------------------------------------------
* Mount Sinai Health System member hospitals: The Mount Sinai Hospital; Mount Sinai Beth Israel; Mount Sinai Brooklyn; Mount Sinai Morningside; Mount Sinai Queens; Mount Sinai South Nassau; Mount Sinai West; and New York Eye and Ear Infirmary of Mount Sinai.
END