(Press-News.org) Rules don't reduce death, morbidity or adverse effects
Surgeon who best knows patient should continue with critical care
Restrictions may hurt patient safety
CHICAGO --- Controversial restrictions on hospital residents' duty hours imposed in 2011 did not improve surgery patients' outcomes, reports a large new Northwestern Medicine study of U.S. hospitals, one of the first national evaluations of the results of the restrictions.
The restrictions also did not result in any differences in surgical residents' performance on exams.
"Our study suggests that these latest duty hour restrictions have no benefit and may actually have the unintended consequences of hurting patient safety, resident education and the doctor-patient relationship," said lead study author Dr. Karl Bilimoria. "They seriously disrupt the continuity of caring for surgical patients, which is vitally important, so we believe the recent 2011 rules should be repealed."
Bilimoria is the director of the Surgical Outcomes and Quality Improvement Center at Northwestern University Feinberg School of Medicine and a surgical oncologist at Northwestern Memorial Hospital. He is also vice chair for quality in the department of surgery at Feinberg.
The study will be published Dec. 9 in the Journal of the American Medical Association.
Some of the first duty hour restrictions implemented in 2003 by the Accreditation Council for Graduate Medical Education (ACGME) were necessary to prevent resident fatigue that leads to errors, the authors said. But the latest round of restrictions in 2011 likely have detrimental effects on surgical patient care.
"The newest rules have led to decreased continuity of care so the same doctor is not able to care for a patient throughout the life-threatening moments of a particular episode," Bilimoria said. "You want the person who knows you to take care of you through the really critical phases. Once you are stabilized or the operation is done, then you can hand off care in a responsible way."
A 2012 meta-analyis and a 2014 review suggested that the latest duty restrictions resulted in more deaths and serious post-operative complications in overall surgical outcomes. While the Northwestern study did not show higher adverse events, Bilimoria said that's probably because other members of the surgical team now bridge the gap in care.
"Now the residents come and go more frequently because the duty hour limits force them to leave and stop taking care of their patients," Bilimoria said. "Previously the residents provided great continuity of care in addition to the attending physician. You had two or more well-trained invested people caring for patients, and now that is often diminished to just the attending physician because of the limitations imposed on residents."
The 2011 restrictions required at least eight hours off between shifts for residents and imposed a 16-hour cap on continuous in-hospital duty for interns (first-year residents).
These ACGME duty hour limits were implemented primarily on the basis of public pressure, not high-level evidence, Bilimoria said.
The rules impair training for residents by creating a shift worker mentality for doctors in training and not allowing them to provide continuity or get the critical educational experiences that only come from taking care of patients during the entirety of a life-threatening episode.
"The rules may need to be different for surgical residents and medical residents," Bilimoria said.
The Northwestern study of general surgery patient outcomes examined the outcomes of 204,641 general surgery patients from 23 teaching and 31 non-teaching hospitals two years before (academic years 2009-2010) and after (academic years 2012-2013) the 2011 duty hour reform.
In adjusted analyses (accounting for the ongoing improvement trend in surgical outcomes), the 2011 ACGME duty hour reform was not associated with a significant change in death or serious morbidity. There also was no association between duty hour reform and any other postoperative adverse outcome.
Northwestern is currently leading a national prospective study in which 152 hospitals have been randomized to either current resident duty hour rules or a subset of the 2003 rules which require no more than an 80-hour work week, call no more frequent than every other night and one day off per week. These restrictions make sense and are well accepted by most teaching hospitals, Bilimoria said.
"Our study results confirm the need for the prospective study," he said. "We are not trying to revoke all duty hour rules; we want to identify and maintain certain key limits while still allowing the flexibility necessary to deliver high-quality patient care and resident education."
INFORMATION:
Other Northwestern authors include: Dr. Ravi Rajaram, Jeanette Chung, Allison Dahlke, Mark Cohen and Dr. David Hoyt.
The research was supported by the Agency for Healthcare Research and Quality, the American College of Surgeons Clinical Scholars in Residence Program and an educational grant from Merck.
NORTHWESTERN NEWS: http://www.northwestern.edu/newscenter/
An examination of the effect of resident duty hour reforms in 2011 finds no significant change in mortality or readmission rates for hospitalized patients, according to a study in the December 10 issue of JAMA, a theme issue on medical education.
In 2011, the Accreditation Council for Graduate Medical Education (ACGME) implemented new duty hour reforms for all ACGME-accredited residency programs. The revisions maintain the weekly limit of 80 hours set forth by the 2003 duty hour reforms but reduced the work hour limit from 30 consecutive hours to 16 hours for firstyear ...
An examination of the effect of resident duty hour reforms in 2011 finds no significant change in outcomes for general surgery patients, according to a study in the December 10 issue of JAMA, a theme issue on medical education.
Ravi Rajaram, M.D., of the American College of Surgeons, Chicago, and colleagues conducted a study to determine if the 2011 Accreditation Council for Graduate Medical Education (ACGME) duty hour reform was associated with a change in general surgery patient outcomes or in resident examination performance.
The study examined general surgery patient ...
Among primary care physicians, the spending patterns in the regions in which their residency program was located were associated with expenditures for subsequent care they provided as practicing physicians, with those trained in lower-spending regions continuing to practice in a less costly manner, even when they moved to higher-spending regions, and vice versa, according to a study in the December 10 issue of JAMA, a theme issue on medical education.
Regional and system-level variations in Medicare spending and overall intensity of medical services delivered to patients ...
An analysis of the non-English-language skills of U.S. medical residency applicants finds that although they are linguistically diverse, most of their languages do not match the languages spoken by the U.S. population with limited English proficiency, according to a study in the December 10 issue of JAMA, a theme issue on medical education.
More than 25 million U.S. residents have limited English proficiency, an 80 percent increase from 1990 to 2010. Limited English proficiency (LEP) may impede participation in the Englishlanguage-dominant health care system. Little ...
There has been a doubling during the last decade in the number of U.S. medical schools that have student-run free clinics, with more than half of medical students involved with these clinics, according to a study in the December 10 issue of JAMA, a theme issue on medical education.
Sunny Smith, M.D., of the University of California, San Diego, and colleagues conducted a study to assess whether there has been growth of student-run free clinics (SRFCs) in medical schools and describe the characteristics of these clinics. The first national study of SRFCs conducted in 2005 ...
In a sample of U.S. emergency departments, compared to attending physicians alone, supervised visits (involving both resident and attending physicians) were associated with a greater likelihood of hospital admission and use of advanced imaging and with longer emergency department stays, according to a study in the December 10 issue of JAMA, a theme issue on medical education.
A common assumption is that care at academic medical centers costs more than care at nonteaching hospitals in part because of a higher frequency of testing and other resource use in teaching settings. ...
PHILADELPHIA - In the first year after the Accreditation Council for Graduate Medical Education (ACGME) reduced the number of continuous hours that residents can work, there was no change in the rate of death or readmission among hospitalized Medicare patients, according to a new study published in JAMA. The study was led by researchers at the Perelman School of Medicine at the University of Pennsylvania and The Children's Hospital of Philadelphia.
"There has been a lot of speculation about the effect of the 2011 ACGME duty hour reforms on patient outcomes, so we looked ...
ROCHESTER, Minn. -- Clinical recommendations discouraging the use of CYP2D6 gene testing to guide tamoxifen therapy in breast cancer patients are based on studies with flawed methodology and should be reconsidered, according to the results of a Mayo Clinic study published in the Journal of the National Cancer Institute.
For years, controversy has surrounded the CYP2D6 gene test for breast cancer. Women with certain inherited genetic deficiencies in the CYP2D6 gene metabolize tamoxifen less efficiently, and thus have lower levels of tamoxifen's active cancer-fighting metabolite ...
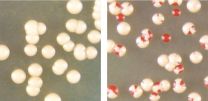
Yeast cells can sometimes reverse the protein misfolding and clumping associated with diseases such as Alzheimer's, according to new research from the University of Arizona.
The new finding contradicts the idea that once prion proteins have changed into the shape that aggregates, the change is irreversible.
"It's believed that when these aggregates arise that cells cannot get rid of them," said Tricia Serio, UA professor and head of the department of molecular and cellular biology. "We've shown that's not the case. Cells can clear themselves of these aggregates."
Prions ...
COLUMBUS, Ohio - Thinking you're good at math and actually being good at it are not the same thing, new research has found.
About one in five people who say they are bad at math in fact score in the top half of those taking an objective math test. But one-third of people who say they are good at math actually score in the bottom half.
"Some people mis-categorize themselves. They really don't know how good they are when faced with a traditional math test," said Ellen Peters, co-author of the study and professor of psychology at The Ohio State University.
The results ...