(Press-News.org) Taking a combination of antidepressants and common painkillers is associated with an increased risk of bleeding soon after starting treatment, finds a study published in The BMJ this week.
The researchers say their results may have been affected by other unmeasured or unknown factors and should be interpreted with caution. However, they suggest special attention is needed when patients use both these classes of drugs together.
Depression produces the greatest decrement in health of all common chronic conditions and depression in older people is an important public health problem.
But concern exists that antidepressants may interact with common painkillers called non-steroidal anti-inflammatory drugs (NSAIDs) to increase the risk of bleeding inside the skull (intracranial haemorrhage).
So a team of researchers based in Korea compared the risk of bleeding among patients treated with antidepressants with and without NSAIDs.
Using the Korean nationwide health insurance database, their study involved over four million people who were prescribed antidepressants for the first time between 2009 and 2013.
NSAID prescriptions were obtained and hospital records were used to identify time to first admission with intracranial haemorrhage within 30 days of a new prescription. Factors that could affect the results, such as age, sex, and use of other medications, were taken into account.
Compared with use of antidepressants alone, the team found that combined use of antidepressants and NSAIDs was associated with a substantially increased bleeding risk.
They found no statistically meaningful differences in risk of bleeding between different types of antidepressant drugs, or with age. Being male was the most common factor for a higher risk of bleeding with combined use of antidepressants and NSAIDs.
"The addition of NSAIDs to antidepressant treatment increased the risk of intracranial haemorrhage within 30 days of the combination starting, especially in men," conclude the authors. "This result adds to evidence confirming the increase of risk with combination use of antidepressants and NSAIDs."
In an accompanying editorial, Dr Stewart Mercer at the University of Glasgow and colleagues at the University of Cambridge, say the results give some cause for concern.
They point out that both types of drug are widely used, and that co-morbidity of the conditions for which these drugs are used is very high - 65% of those with major depression also have chronic pain.
They urge family doctors to be extra vigilant in terms of prescribing behaviour and discussing the risks with patients, especially in deprived areas where "the combination of mental and physical problems (including chronic pain) is very common." And they say further research is required to extend the findings over longer time periods and in differing populations.
INFORMATION:
Women should be able to treat cystitis themselves with antibiotics without a prescription, says a general practitioner in The BMJ this week.
Dr Kyle Knox says this would save three million scarce GP appointments a year.
Acute uncomplicated urinary tract infections (AUUTIs) such as cystitis are the most common bacterial infections in women. Cystitis affects around half of women at least once in their lifetime and is coded as the reason for 1% of the 300 million GP consultations held annually in the UK.
Management of cystitis is straightforward - a short course of ...
Should doctors recommend homeopathy? Two experts debate the issue in The BMJ this week.
Peter Fisher, Director of Research at the Royal London Hospital for Integrated Medicine, says that of all the major forms of complementary medicine, homeopathy is the most misunderstood.
He questions the methods used to review the evidence for homeopathy. For example, in a recent report by the Australian National Health and Medical Research Council which stated that "there are no health conditions for which there is reliable evidence that homeopathy is effective."
"The fact that ...
Standardised mortality ratios (SMRs) for hospitals do not provide an accurate picture of how many deaths could have been avoided, according to a new study by researchers at the London School of Hygiene & Tropical Medicine and Imperial College London published in the BMJ.
The authors say the widely used hospital-wide standardised mortality ratios, such as HSMR (Hospital Standardised Mortality Ratio) and SHMI (Summary Hospital level Mortality Indicator), should not be used to benchmark hospitals' quality of care.
Hospital-wide SMRs compare the number of deaths in a hospital ...
The first comprehensive genome analyses of 7 melon varieties was completed by a research team led by Josep Casacuberta, Jordi Garcia-Mas and Sebastian Ramos-Onsins, providing breeders new knowledge important for understanding phenotypic variability and helping increasing plant quality yields by selective breeding. The findings were published in the advanced online edition of Molecular Biology and Evolution.
The researchers sought to bridge the gap between expanding the genetic knowledge of melons and understanding important traits such as flavor, size and water use.
The ...
Disruptions in a key brain region can explain the varied outcomes after a traumatic brain injury (TBI) in children and adolescents, according to research published July 15 in The Journal of Neuroscience. Post-injury outcomes vary widely, and injury severity can only explain some of this variance. Combining data from brain imaging and recording, researchers at the University of Southern California and UCLA found that disruptions in the structure and function of a brain region called the corpus callosum could explain the variance in cognitive outcomes.
TBI is the leading ...
Why do some youngsters bounce back quickly from a traumatic brain injury, while others suffer devastating side effects for years?
New UCLA/USC research suggests that damage to the fatty sheaths around the brain's nerve fibers--not injury severity-- may explain the difference. Published in the July 15 edition of the Journal of Neuroscience, the finding identifies possible biomarkers that physicians could use to predict higher-risk patients who require closer monitoring.
The study is the first to combine imaging scans with recording of the brain's electrical activity ...
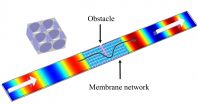
WASHINGTON, DC, July 14, 2015 -- When a sound wave hits an obstacle and is scattered, the signal may be lost or degraded. But what if you could guide the signal around that obstacle, as if the interfering barrier didn't even exist? Recently, researchers at Nanjing University in China created a material from polyethylene membranes that does exactly that.
Their final product, described this week in the Journal of Applied Physics, from AIP Publishing, was an acoustical "metamaterial" with an effective density near zero (DNZ). This work could help to endow a transmission ...
A quick biological test may be able to identify children who have literacy challenges or learning disabilities long before they learn to read, according to new research from Northwestern University.
The study, publishing in the Open Access journal PLOS Biology on July 14th, centers on the child's ability to decipher speech -- specifically consonants -- in a chaotic, noisy environment. Preliterate children whose brains inefficiently process speech against a background of noise are more likely than their peers to have trouble with reading and language development when ...
A yearlong study of more than 300 patients found that the investigational drug patiromer can reduce elevated blood-potassium levels--a common side effect of drugs essential in the treatment of chronic diabetic kidney disease.
The drug, given in this trial at one of four doses based on disease severity, returned blood potassium levels to normal when measured at four weeks and kept them under control for one year, the length of the trial. By quickly bringing potassium levels back to normal and keeping them there, patiromer can prevent life-threatening adverse events.
The ...
The new guidelines for determining whether patients should begin taking statins to prevent cardiovascular disease issued in 2013 by the American College of Cardiology (ACC) and the American Heart Association (AHA) are more accurate and more efficient than an earlier set of guidelines in assigning treatment to adults at increased risk for cardiovascular events - including heart attacks and strokes - and identifying those whose low risk rules out the need to take statins. In their paper appearing in the July 15 issue of JAMA, a team led by Massachusetts General Hospital (MGH) ...