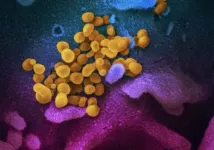
After a year of the pandemic, an increasingly clear picture is emerging for science and medicine of how the immune response protects people from SARS-CoV-2. Two protagonists play central roles: antibodies and T-killer cells (also called cytotoxic CD8 T cells). While antibodies dock directly onto viruses to render them harmless, T-killer cells recognize viral protein fragments on infected cells and subsequently kill them to stop virus production. More and more studies show that SARS-CoV-2 can evade the antibody immune response through mutations and thus also impair the effectiveness of vaccines. Whether such mutations also affect T-killer cells in their function had not been clarified so far. Benedikt Agerer in the laboratory of Andreas Bergthaler (CeMM), Maximilian Koblischke and Venugopal Gudipati in the research groups of Judith Aberle and Johannes Huppa (both Medical University of Vienna) have now worked together closely to investigate the effect of viral mutations in so-called T cell epitopes, i.e., in regions recognized by T-killer cells. For this purpose, they sequenced 750 SARS-CoV-2 viral genomes from infected individuals and analyzed mutations for their potential to alter T cell epitopes. "Our results show that many mutations in SARS-CoV-2 are indeed capable of doing this. With the help of bioinformatic and biochemical investigations as well as laboratory experiments with blood cells from COVID-19 patients, we were able to show that mutated viruses can no longer be recognized by T-killer cells in these regions," says Andreas Bergthaler.
Focus on spike protein might be too narrow
In most natural infections, several epitopes are available for recognition by T-killer cells. If the virus mutates in one place, it is likely that other epitopes indicate the presence of the virus. Most of the current vaccines against SARS-CoV-2 are directed exclusively against the so-called spike protein, which is one of 26 virus proteins. This also reduces the number of epitopes that are available for recognition by T-killer cells. "The spike protein has, on average, one to six of these T cell epitopes in an infected person. If the virus mutates in one of these regions, the risk that the infected cells will not be recognized by the T-killer cells increases," explains Johannes Huppa. Judith Aberle emphasizes: "Especially for the further development of vaccines, we therefore have to keep a close eye on how the virus mutates and which mutations prevail globally. Currently, we see few indications that mutations in T killer cell epitopes are increasingly spreading."
The study authors see no reason in their data to believe that SARS-CoV-2 can completely evade the human immune response. However, these results provide important insights into how SARS-CoV-2 interacts with the immune system. "Furthermore, this knowledge helps to develop more effective vaccines with the potential to activate as many T-killer cells as possible via a variety of epitopes. The goal are vaccines that trigger neutralizing antibody and T killer cell responses for the broadest possible protection," the study authors say.
INFORMATION:
Authors: Benedikt Agerer*, Maximilian Koblischke*, Venugopal Gudipati*, Luis Fernando Montaño-Gutierrez, Mark Smyth, Alexandra Popa, Jakob-Wendelin Genger, Lukas Endler, David M. Florian, Vanessa Mühlgrabner, Marianne Graninger, Stephan W. Aberle, Anna-Maria Husa, Lisa Ellen Shaw, Alexander Lercher, Pia Gattinger, Ricard Torralba-Gombau, Doris Trapin, Thomas Penz, Daniele Barreca, Ingrid Fae, Sabine Wenda, Marianna Traungott, Gernot Walder, Winfried F. Pickl, Volker Thiel, Franz Allerberger, Hannes Stockinger, Elisabeth Puchhammer-Stöckl, Wolfgang Weninger, Gottfried Fischer, Wolfgang Hoepler, Erich Pawelka, Alexander Zoufaly, Rudolf Valenta, Christoph Bock, Wolfgang Paster, René Geyeregger, Matthias Farlik, Florian Halbritter, Johannes B. Huppa**, Judith H. Aberle**, Andreas Bergthaler**
*, **Equal contribution
Funding: This project was funded in part by two grants from the Vienna Science and Technology Fund (WWTF) as part of the WWTF COVID-19 Rapid Response Funding 2020 awarded to Andreas Bergthaler and René Geyeregger, respectively.
Benedikt Agerer was supported by the Austrian Science Fund (FWF) DK W1212. Mark Smyth and Alexander Lercher were supported by DOC fellowships of the Austrian Academy of Sciences (No. 24813, No. 24158 and No. 24955 respectively). Venugopal Gudipati, Vanessa Mühlgrabner and Johannes B. Huppa received support from the Vienna Science and Technology Fund (WWTF, LS14-031). Judith H. Abele was supported by the Medical-Scientific fund of the Mayor of the federal capital Vienna (grant COVID003). Winfried F. Pickl. was supported by the Medical-Scientific fund of the Mayor of the federal capital Vienna (grant COVID006). Christoph Bock and Andreas Bergthaler were supported by ERC Starting Grants (European Union's Horizon 2020 research and innovation program, grant agreement numbers 679146 respectively 677006).
Judith Aberle is a virologist and Associate Professor of Virology at the Medical University of Vienna. She studied medicine in Vienna and performed her research education at the Center for Virology. She leads a group with expertise in the areas of virology and viral immunology, working in close cooperation with other research groups at the Center for Virology. Current projects comprise investigations of SARS-CoV-2-specific T cell subsets and longitudinal kinetics of antibody titers from blood of COVID-19 patients, specific mutational patterns in serial samples taken from immunosuppressed patients and their effect on disease severity.
Andreas Bergthaler studied veterinary medicine in Vienna. After his doctorate under Hans Hengartner and Nobel Prize winner Rolf Zinkernagel at the University of Zurich and the ETH Zurich, he completed postdoctoral research stays at the University of Geneva and the Institute for Systems Biology in Seattle. Since 2011 he has been a research group leader at CeMM and ERC Start Laureate.
Johannes Huppa teaches molecular immunology at the Medical University of Vienna. His primary interest revolves around the question of how T lymphocytes manage to detect minute quantities of antigens. Looking for answers he devises together with his team molecular imaging modalities to apply them in combination with biophysical and system-biological approaches.
The mission of CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences is to achieve maximum scientific innovation in molecular medicine to improve healthcare. At CeMM, an international and creative team of scientists and medical doctors pursues free-minded basic life science research in a large and vibrant hospital environment of outstanding medical tradition and practice. CeMM's research is based on post-genomic technologies and focuses on societally important diseases, such as immune disorders and infections, cancer and metabolic disorders. CeMM operates in a unique mode of super-cooperation, connecting biology with medicine, experiments with computation, discovery with translation, and science with society and the arts. The goal of CeMM is to pioneer the science that nurtures the precise, personalized, predictive and preventive medicine of the future. CeMM trains a modern blend of biomedical scientists and is located at the campus of the General Hospital and the Medical University of Vienna. http://www.cemm.at
Medical University of Vienna (MedUni Vienna) is one of the most traditional medical education and research facilities in Europe. With almost 8,000 students, it is currently the largest medical training center in the German-speaking countries. With 5,500 employees, 30 departments and two clinical institutes, 12 medical theory centers and numerous highly specialized laboratories, it is also one of Europe's leading research establishments in the biomedical sector. http://www.meduniwien.ac.at/web/en