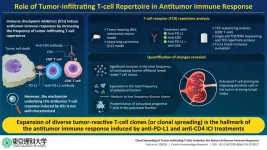
Immune checkpoint inhibitors (ICIs) are widely sought after for the treatment of different types of cancers. Unfortunately, only 20–30% patients with cancer respond to ICI treatment. Although the factors that influence the positive or negative response to ICI treatment are poorly understood, the strength of the ICIs’ antitumor response by TILs is thought to play a key role. Hence, investigating the antitumor response induced by ICIs might provide insights into their underlying mechanism.
It is known that CD8+ tumor-infiltrating T-lymphocytes (TILs) are the primary effector cells that lead to antitumor response. TILs are composed of various T-cell clones that are determined by their unique T-cell receptor (TCR) genes. A diverse TCR repertoire can indicate the existence of TIL population that can recognize multiple tumor-antigens. However, the way the diversity of tumor-reactive clones influences their antitumor effects remains unclear.
To this end, a team of researchers led by Associate professor Satoshi Ueha, including Dr. Shigeyuki Shichino and Professor Kouji Matsushima from the Tokyo University of Science, and Mr. Hiroyasu Aoki from The University of Tokyo, Japan, investigated the correlation between TIL clones and their antitumor effects. Their work was published in Cancer Immunology Research.
Discussing the team’s motivation behind this study, Prof. Ueha explains, “By clarifying the mechanism by which ICIs increase tumor reactive CD8+ T cells, we hoped to develop a diagnostic method to predict the efficacy of this therapy as well as a new combined cancer immunotherapy”.
First, the team analyzed the TCR repertoire of B16F10 and Lewis lung carcinoma (LLC) tumor bearing mice, treated with the ICIs—anti-PD-L1 anti-CD4, and a combination of both (CD4 + PDL1) antibodies. They observed that the antibodies increased the mobilization of overlapping (OL) T-cell clones in draining lymph nodes (dLNs) and tumors.
Next, they categorized the dLN-tumor OL clones into oligoclonal and polyclonal fractions. They found that ICI administration significantly increased the polyclonal fraction of OL repertoire but not the oligoclonal fraction in both tumor model. These findings confirmed that the increase in dLN-tumor repertoire was due to clonal spreading, i.e., the expansion of diverse polyclonal clones, and not clonal skewing, i.e., the expansion of oligoclonal clones.
The team further found that increase of the polyclonal fraction of OL repertoire due to ICI administration was correlated with the tumor volume after treatment, a parameter reflecting an antitumor effect. Moreover, single-cell RNA and TCR sequencing exhibited that the polyclonal dLN-tumor OL clones were rich in progenitor exhausted T cells (T cells having more proliferative potential and play an important role in the antitumor effects of ICI).
After establishing that clonal spreading was responsible for effective antitumor response to ICIs, Associate Prof. Ueha and his team investigated the mechanism of clonal spreading. They used tumor-bearing knock-in mice that were selectively depleted of dLN migratory dendritic cells (migDCs) and treated them with anti-PD-L1 and anti-CD4 antibodies. Upon examining the dLN-tumor OL clones, they noted that ICIs enhanced the priming of polyclonal tumor-reactive T-cells by migDCs in the dLN, resulting in clonal spreading.
So, what are the future implications of these findings? “Our results can be used to predict and diagnose the efficacy of ICIs, thereby making it possible to deliver these rather expensive drugs to patients who can benefit from them. In the long term, the clonal spreading response found in our study may be used to develop therapeutic drugs that induce stronger anti-tumor T-cell responses when used in combination with ICIs,” muses a hopeful Prof. Ueha. He also believes that focusing on a greater variety of tumor reactive clones and their proliferation can have important implications in advancing this field of research.
We are confident that the applications of these ICIs will soon extend to clinical trials and bring much needed respite to patients grappling with cancer.
***
Reference
DOI: https://doi.org/10.1158/2326-6066.CIR-22-0517
About The Tokyo University of Science
Tokyo University of Science (TUS) is a well-known and respected university, and the largest science-specialized private research university in Japan, with four campuses in central Tokyo and its suburbs and in Hokkaido. Established in 1881, the university has continually contributed to Japan's development in science through inculcating the love for science in researchers, technicians, and educators.
With a mission of “Creating science and technology for the harmonious development of nature, human beings, and society", TUS has undertaken a wide range of research from basic to applied science. TUS has embraced a multidisciplinary approach to research and undertaken intensive study in some of today's most vital fields. TUS is a meritocracy where the best in science is recognized and nurtured. It is the only private university in Japan that has produced a Nobel Prize winner and the only private university in Asia to produce Nobel Prize winners within the natural sciences field.
Website: https://www.tus.ac.jp/en/mediarelations/
About Associate Professor Satoshi Ueha from Tokyo University of Science
Dr. Satoshi Ueha is an Associate Professor at the Research Institute for Biomedical Sciences, Tokyo University of Science, Japan. Prof. Ueha specializes in tumor immunology and transplantation immunology. He has over 150 publications that have been extensively read and cited. He also holds 9 patents, of which the latest one has been granted for a method that can predict cancer treatment effects using immune checkpoint inhibitors.
Funding information
This study was supported by the Japan Society for the Promotion of Science under Grant Number 20281832 and 17929397, and by the Japan Agency for Medical Research and Development (AMED) under Grant Number JP 21gm6210025, 22fk0310509s0101, and 22ama221306h0001.
END