(Press-News.org) EHR Workload Continues to Grow for Primary Care Physicians
The study evaluated recent trends in primary care physicians’ (PCPs) electronic health record (EHR) workload. Prior to and early in the COVID-19 pandemic, PCPs spent more time in the EHR and received more messages than physicians in other specialties, but it is unclear if the pandemic further accelerated the growth of PCPs’ EHR workload. Researchers observed EHR usage of 141 academic PCPs practicing family medicine, internal medicine, and general pediatrics within the University of Wisconsin-Madison health system, which cares for nearly 300,000 primary care patients per year. This longitudinal study compared the amount of time participating PCPs spent on EHR tasks during four periods across four years: May 2019–February 2020; June 2020–March 2021; May 2021–March 2022; and April 2022–March 2023. EHR time and inbox message volume were calculated for each PCP and normalized per 8 hours of scheduled clinic appointments. The volume of messages PCPs received increased significantly in May 2019–February 2020 and April 2022–March 2023 for three message types, including MyChart messages (+5.4 messages, 55.5%), prescription refills (+2.3 messages, 19.5%), and eConsults (+0.12 messages, 61.0%), while the volume of patient calls (–2.8 messages, –10.5%) and results messages (–0.3 messages, –2.7%) both decreased. PCPs spent nearly 30 minutes more (7.8%) on EHR tasks per 8 hours of scheduled clinic appointments between the pre-pandemic period (May 2019–February 2020) and the final year of the study (April 2022–March 2023). Time spent on EHR tasks outside of scheduled hours also increased by 6.4 minutes (8.2%) on days with scheduled appointments and 13.6 minutes (19.9%) on days without scheduled appointments.
What We Know: For primary care physicians, completing EHR tasks and responding to patients’ inbox messages take up a significant amount of time, often including working after-hours. Not only do such demands impinge on their clinical and personal time, they also put PCPs at risk of burnout and can factor into their decision to cut back on time in clinic or leave the profession.
What This Study Adds: PCPs’ time in the EHR continues to grow. Although PCPs’ inbox time may be stabilizing, it is still substantially higher than pre-pandemic levels. It is imperative that health systems develop strategies to change the EHR workload trajectory to minimize PCPs’ occupational stress and mitigate unnecessary reductions in effective physician workforce resulting from the increased EHR burden.
More Tethered to the EHR: EHR Workload Trends Among Academic Primary Care Physicians, 2019–2023
Brian G. Arndt, MD, et al.
Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Clear and Open Communication With Care Teams Could Improve the Birthing Experience for Black People
This study explored the perspectives of Black birthing people on how better communication with care teams may have improved their birth experiences. Researchers interviewed 30 non-Hispanic Black, English-language–proficient, low-income birthing people in the Philadelphia, Pennsylvania, area, all of whom were insured by Medicaid. All gave birth to preterm infants before 34 weeks gestation, or before 36 weeks gestation to birthing people with a modifiable risk factor such as high blood pressure. The interviews uncovered three main themes regarding the quality of communication with their care teams and the effect on their experiences: 1) communication gaps during urgent or emergent intrapartum procedures contributed to negative birth experiences; 2) postpartum opportunities to share birth experiences, particularly with peers, sometimes mitigated the psychological consequences of negative birth experiences; and 3) interviewees did not consistently discuss concerns about future pregnancy risk related to negative birth experiences with their clinical teams.
What We Know: Physically or psychologically distressing birth experiences can influence postpartum health, parenting efficacy, and future pregnancy plans. Obstetric racism, in the form of interpersonal racism (e.g.,the effect of clinician bias on relationships and communication with patients) and/or structural racism (underfunded and/or understaffed facilities serving predominantly Black populations), may create negative birth experiences for Black birthing people.
What This Study Adds: This study adds an important patient perspective on racial inequities in maternal health care in the U.S. The findings suggest that health systems could promote positive birth experiences for Black birthing people by improving communication during emergency intrapartum procedures, fostering a welcoming environment for sharing their birth experiences, and promoting ongoing conversations with care teams about future pregnancy risks they may face.
Communication and Birth Experiences Among Black Birthing People Who Experienced Preterm Birth
Emily F. Gregory, MD, MHS, et al.
Department of Pediatrics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
A Simple Three-Question Screening Tool May Help to Identify Precarious Employment Among Primary Care Patients
Precarious employment, defined by temporary contracts, unstable employment, or job insecurity, is increasingly common and is associated with inconsistent access to health insurance, lower incomes, and greater exposure to physical hazards and psychological stress. A team of researchers in Toronto, Canada, created and tested a new three-question screening tool to help primary care clinics identify these patients. The screener included the following three questions: 1) non-standard employment (Are you currently employed in a casual, short-term, or temporary position?); 2) violations of occupational health and safety rights and protections (Do you feel fearful that you could be fired if you raised employment concerns?); and 3) income variability (Does your pay vary a lot from month to month?).
To test the validity of their screening tool and assess the feasibility of adding these questions to social determinant screening, the research team recruited a convenience sample of 200 people in waiting rooms at seven Toronto clinics in areas with higher poverty rates than the rest of the city. Participants ranged in age from 18 to 72 years (mean 38), fluency in English, and employed, with 93 (45.6%) identifying as men and 119 (58.3%) identifying as White. Participants also completed the Poverty and Employment Precarity in Southern Ontario (PEPSO) Employment Precarity Index. The PEPSO Index uses a score ranging from 0 to 100 to categorize work status along a gradient (secure, stable, vulnerable, and precarious). A score of 38 or above suggests a precarious employment status. Those who answered yes to at least two of the questions on the researchers’ survey were almost four times more likely to be precariously employed based on their PEPSO scores.
What We Know: Employment is a key social determinant of health, with a significant impact on one’s income, access to basic necessities, and social connectedness. While primary care physicians screen for other social determinants of health, they do not ask about employment concerns. People with chronic health issues are at greater risk of experiencing precarious employment and may face difficulty re-entering the workforce if unemployed. While it is especially important to screen for precarious employment in primary care settings, there exists no standard screening tool at this time.
What This Study Adds: The results of this study suggest that a simple three-question screener could help identify precarious employment among primary care patients and serve as an opening for conversations in clinical settings about employment precarity and work conditions. Implementation of this screener in primary care settings could improve how resources are targeted for managing care and how patients are connected with relevant support services; regional pooling of data collected in this way could spark policy changes on a broader scale to reduce precarious employment. The researchers note that clinicians may need direction in how and when to intervene based on their patients’ responses to the screening questions, and that clinical time constraints may make it difficult to obtain more detailed information.
A Brief Tool to Screen Patients for Precarious Employment: A Validation Study
Andrew D. Pinto, MD, CCFP, FRCPC, MSc, et al.
Upstream Lab, MAP/Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute, Unity Health Toronto, Toronto, Ontario, Canada
Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada
Interdisciplinary Health Program, St. Francis Xavier University, Antigonish, Nova Scotia, Canada
Department of Family and Community Medicine, St. Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada
Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Primary Care Physicians and Urologists Work Together to Provide Optimal Care for Men With Low-Risk Prostate Cancer
This study considers the perspectives of primary care physicians (PCPs) and urologists on what facilitates and what creates barriers to active surveillance (AS) care for men with low-risk prostate cancer. Researchers conducted in-depth, semi-structured interviews with 19 PCPs (9 female, 4 in community practices, 15 in academic medical centers) and 15 urologists (3 female, 5 in private practice, 3 in academic medical centers) between June 2020 and March 2021. Their goal was to assess interviewees’ knowledge of AS, what factors they felt influence adherence to follow-up testing, and their preferences concerning PCPs’ and urologists’ roles in team-based care delivery.
Both PCPs and urologists noted the importance of patient education. Patients who understand AS are more likely to select it and adhere to follow-up. While urologists were most knowledgeable about AS, PCPs may lack a good general understanding of AS as well as its follow-up protocols and how to interpret test results. They may find it difficult to explain AS to their patients and often defer to urologists.
Both PCPs and urologists recognized that patients can become lost to follow-up. One way to prevent this is for doctors to communicate more directly with each other about a shared patient’s treatment (e.g., by phone instead of electronic health records). PCPs should discuss urologist visits with their patients. However, PCPs and urologists tended to agree that the PCP role in AS is mainly supportive, with urologists handling follow-up care.
What We Know: Over the past 20 years, U.S. national guidelines for managing care for men with low-risk prostate cancer have moved away from surgery or radiation, with their risk of overtreatment and harmful side effects, in favor of active surveillance (AS). AS involves routine urologist visits, prostate-specific antigen (PSA) lab testing, and serial tumor burden reassessment with magnetic resonance imaging (MRI) or prostate biopsy at recommended intervals. As of 2021, AS has increased to nearly 60% nationwide, though adherence to treatment and follow-up have been uneven, and some men whose condition is stable may receive more intensive treatment than they need. At the same time, patients are increasingly involving their PCPs in their cancer care.
What This Study Adds: While prior studies have addressed the role of PCPs in team-based care delivery for cancer survivors, PCPs’ role in AS care for men with low-risk prostate cancer remains unexplored. The PCPs and urologists interviewed for this study revealed how they view their complementary roles in AS care. Clear communication—between doctors and patients as well as among care team members—is essential. Urologists have greater knowledge of AS and take the lead in managing treatment for patients with low-risk prostate cancer.
Primary Care Physician and Urologist Perspectives on Optimizing Active Surveillance for Low-Risk Prostate Cancer
Archana Radhakrishnan, MD, MHS, et al.
Department of Internal Medicine, University of Michigan, Ann Arbor, MI
Center for Clinical Management Research, VA Ann Arbor Healthcare System, Ann Arbor, MI
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Patients Who Obtained Telemedicine Medication Abortions (TeleMAB) Through Primary Care Have Positive Feelings About Their Experience
This study explores patients’ experiences and perspectives on obtaining telemedicine medication abortions (TeleMAB) through their primary care health system. Researchers conducted in-depth phone interviews with 14 English, Spanish, and/or Portuguese-speaking patients, ranging in age from 26 to 42, who received a TeleMAB between July 2020 and December 2021 from a large primary care safety-net community health system in Massachusetts. Thirteen of the interviewees provided demographic information. All 13 identified as female, and 10 had children between 8 months and 15 years old. Six (42.8%) identified as African American/Black, three (21.4%) as Asian/Pacific Islander/Native Hawaiian, two (14.3%) as White and Black, one (7%) as White, and one as Hispanic/Latino.
Three main themes emerged from the interviews. First, participants found the process of obtaining TeleMAB through primary care to be easy. The medication was delivered as expected, and the provider counseling and clear instructions made them feel well prepared. They were comfortable with their primary care network; while some participants received care from someone other than their regular primary care doctor, they were able to trust another provider from the network. Second, telemedicine allowed them to receive abortion care at home or wherever they felt safe and comfortable. This decreased anxiety as well as disruptions to their daily lives. Third, primary care normalizes abortion care. An abortion clinic might feel unfamiliar and unknown, whereas the primary care relationship is established and familiar. A primary care physician can provide abortion care in the context of the patients’ other medical concerns and history. Overall, the participants in this study expressed positive feelings about their TeleMAB experience centering around these three themes.
What We Know: Throughout the United States, laws restricting access to reproductive health care, and especially access to abortion, continue to be introduced and enacted. Since the U.S. Supreme Court overturned Roe v. Wade with its June 2022 decision in Dobbs v. Jackson Women’s Health Organization, almost half of all U.S. states have severely restricted or banned abortion care altogether. This disproportionately affects underserved and minority people, who make up about 70% of those who obtain abortion services and for whom primary care is critical. Prior to Dobbs, few primary care practices offered abortion, yet abortion in primary care settings, including direct-to-patient telemedicine medication abortion (TeleMAB), in which pills are mailed to patients and medical guidance is provided remotely, has been shown to be a safe, feasible, and effective option.
What This Study Adds: Although research has shown that administering TeleMAB by primary care is safe and efficient, no previous study has evaluated patients’ experiences obtaining TeleMAB through their primary care health system. Overall, the participants interviewed for this study felt that using TeleMAB services through their primary care health system was a positive and easy experience. This supported their ability to exercise control over their treatment, allowed them autonomy and flexibility, and decreased barriers they may have experienced with in-clinic care. Many said they use primary care for pregnancy-related health care needs, and they valued receiving abortion care from their regular clinicians within the context of their ongoing care for other medical concerns. Primary care practices can integrate TeleMAB services to decrease care silos, normalize abortion as a part of comprehensive primary care, and improve access for many people of reproductive age through remote care.
Telemedicine Abortion in Primary Care: An Exploration of Patient Experiences
Amy Tressan, MD, et al.
Department of Family Medicine, Planned Parenthood of Orange and San Bernardino Counties, Anaheim, CA
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
A Quality Improvement Intervention Links High-Risk Prenatal Patients at Safety-Net Health Centers With Primary Care
Researchers assessed the development and implementation of a quality improvement learning collaborative’s (QILC) intervention to link high-risk prenatal patients with primary care. The aims of the study were twofold: to identify any quantitative impact of the intervention on postpartum and primary care utilization for high-risk prenatal patients and to explore the Federally Qualified Health Center (FQHC) participants’ experiences of working with a QI collaborative.
Using information from patients’ charts and/or electronic health records (EHRs), 19 clinics within the six participating FQHCs identified high-risk prenatal patients in their care who delivered between January and June 2021. High-risk conditions included pregestational diabetes, gestational diabetes, gestational/chronic hypertension, and depression. The QI intervention implemented a patient registry to facilitate linking these patients to primary care within six months of delivery. FQHC participants conducted direct patient outreach through six months postpartum to connect patients to postpartum and primary care. The researchers compared data reported by the FQHC at the start and end of the intervention. The primary outcome was the change in proportion of high-risk patients with a documented primary care visit within six months postpartum, while the secondary outcome was the change in proportion of patients with a documented postpartum visit within six weeks post-delivery. The former measure increased from 25% to 72%, while the latter went from 83% up to 91%. At the conclusion of the intervention, all six FQHCs had successfully implemented processes for coordinating their maternal and primary care. However, post-implementation, only five chose to continue following the new processes they had developed.
What We Know: Maternal mortality rates continue to rise across the United States, with non-Hispanic Black birthing people being disproportionately affected—in 2020, they were almost three times more likely to die than non-Hispanic White birthing people. As many deaths occur postpartum, transitioning from prenatal to primary care and remaining engaged in care throughout the first year are critical preventive steps.
What This Study Adds: This was the first initiative in Chicago to directly tackle the issue of maternal mortality and morbidity across multiple community-based clinics sites using a QILC framework. The researchers found that, by both quantitative and qualitative measures, FQHC participation in this QILC intervention significantly improved postpartum and primary care utilization for high-risk prenatal patients, albeit with challenges resulting from institutional and structural factors. Greater resources are necessary to ensure sustainability.
A Mixed Methods Evaluation of a Quality Improvement Model to Optimize Perinatal and Primary Care in the Community Health Setting
Jena Wallander Gemkow, MPH, BSN, RN, et al.
AllianceChicago, Chicago, IL
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
An Update on a 2015 Report Shows That Gabapentinoid Usage in the U.S. Has Continued to Climb
Gabapentinoids are commonly prescribed for an array of off-label conditions, including management of chronic pain. Updating their 2015 report on gabapentinoid usage in the U.S., researchers used the 2002–2021 Medical Expenditure Panel Survey (MEPS) to investigate the proportion of the adult population using gabapentinoids, medications, and diagnoses associated with users, and the likelihood of starting, stopping, or continuing gabapentinoids. They found that gabapentinoid use has increased from 4.0% in 2015 to 4.7% in 2021. Gabapentinoids continue to be used in conjunction with other sedating medications, despite a 2019 FDA warning against doing so. Although off-label use is difficult to connect with specific medical conditions and is likely under-reported, numerous chronic pain conditions remain associated with gabapentinoids. Between the survey periods of 2011–2012 and 2017–2018, the percentage of those continuing to use gabapentinoids year on year was greater than those who stopped, though this difference appears to have decreased more recently.
What We Know: Gabapentinoid prescription and use continues to increase in the U.S., from 4.0% in 2015 to 4.7% in 2021. Despite a 2019 FDA warning, gabapentinoids continue to be used in conjunction with other sedating medications.
What This Study Adds: Gabapentinoid users have continued to increase since the authors’ 2015 publication, despite a dearth of evidence supporting use in many cases. While these clinical scenarios can be challenging, continuation should be reconsidered at regular intervals.
Update to Gabapentinoid Use in the United States, 2002–2021
Michael E. Johansen, MD, MS
Grant Family Medicine, OhioHealth, Columbus, OH
Donovan T. Maust, MD, MS
Center for Clinical Management Research, VA Ann Arbor Health Care System, Ann Arbor, MI;
Department of Psychiatry, University of Michigan, Ann Arbor, MI
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
The Serious Risks and High Costs of Monoclonal Antibodies May Outweigh the Benefits for Patients With Alzheimer Dementia
Researchers performed a meta-analysis of randomized trial studies that compared the use of amyloid-reducing monoclonal antibodies (MABs) in patients with Alzheimer dementia at a dose consistent with that used in Phase 3 or FDA approval trials with the use of a placebo. Their purpose was to evaluate clinically meaningful benefits and harms of MABs to these patients. For inclusion in this meta-analysis, the RCT studies had to include adult participants with cognitive impairment or Alzheimer disease of any severity and report at least one clinically relevant benefit or harm to participants after at least one year. The research team identified 19 such publications that evaluated the effects of 8 different MABs on a total of 23,202 participants. Neither the results of any single study nor the results of all combined studies showed quantitative evidence that MABs improved cognitive or day-to-day functional abilities beyond the measure of minimal clinically important differences (MCIDs). Conversely, the studies indicated that MABs consistently cause statistically significant harms and could increase patients’ risk of serious harms such as cerebral edema, hemorrhage, serious adverse events, and death. Additionally, these drugs are prohibitively expensive ($26,500 to $28,200 per year) and require regular MRI monitoring.
What We Know: The theory that amyloid deposition is part of the causal pathway in the development of Alzheimer dementia has led to the development of MABs to reduce amyloid deposition. FDA approval of these drugs was based primarily on improvements to laboratory measures such as medical imaging and biomarkers. However, the failure of MABs to provide clinically significant improvement in patient-oriented outcomes such as reduced mortality or morbidity has resulted in controversy. Previous systematic reviews evaluating the efficacy and harms of using MABs to target amyloid did not include recent studies that were critical to drug approval, and some included Phase 1 and 2 trials that used different doses from those used in later trials and did not interpret the findings in the context of minimal clinically important differences for patient outcomes.
What This Study Adds: Although lab-based evidence shows that MABs may be a promising treatment for Alzheimer dementia, focusing on actual patient outcomes can provide a greater understanding of the potential benefits and harms of using MABs. This meta-analysis of recent clinical trials involving over 20,000 participants with Alzheimer dementia or similar cognitive impairments suggests that MABs have not been shown to lead to clinically significant improvements in cognitive or functional abilities and could potentially cause serious harm to patients taking these drugs.
Clinically Important Benefits and Harms of Monoclonal Antibodies Targeting Amyloid for the Treatment of Alzheimer Disease: A Systematic Review and Meta-Analysis
Mark H. Ebell, MD, MS, et al.
Department of Epidemiology and Biostatistics, College of Public Health, University of Georgia, Athens, GA
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Telemedicine is Changing the Practice of Family Medicine, Not Necessarily for the Better
A family doctor considers how the growth of telemedicine in primary care affects the role of physicians and relationships with their patients. Through anecdotes of her telemedicine experiences with her patients, she demonstrates what is lost without in-person clinical visits. She calls for a renewed commitment to the values of building interpersonal relationships and clinical experience in training the next generation of family doctors.
Telemedicine Could Reduce the Role of Family Physicians to Case Managers
Ruth Kannai, MD
Department of Family Medicine, The Haim Doron Division of Community Health,
Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Aya Rice (Alon), MA, Clinical psychologist
Department of Counseling and Human Development, Haifa University, Haifa, Israel
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Understanding Patients’ Lived Experiences, Especially When It Comes to Race, Is Essential in Providing Equitable Health Care
A Black family medicine resident—the only one on his team—was able to allay the fears of a young Black patient and his mother about starting a new medication when other team members could not. When a senior team member chastised him in a team meeting for addressing the issue of race in the exam room—they treat all patients as equals—the junior resident explained that racial and cultural disparities in medicine do have a significant impact on patients’ experiences.
The Color of Medicine
John E. Ukadike, DO, MPH, PGY1 Resident
University of Nebraska Medical Center Emergency Medicine Residency Program, Omaha, NE
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Family Health Care Teams Provide Access to Care Along the Amazon River
For people in rural communities along the Amazon River, the long distance to the nearest health center creates a significant challenge to health care access. To address this issue, floating primary health centers (PHCs)—boats outfitted with medical and dental consulting rooms, procedure rooms, vaccination facilities, a lab, and a pharmacy—bring basic care to them. Staffed with family physicians, nurses, dentists, pharmacists, and support staff, floating PHCs stay in each community for 1–3 days, serve up to 100 people daily, and return every three months. This groundbreaking, scalable approach represents a crucial step toward health equity for isolated, often-overlooked communities in the Amazon.
The Floating Primary Health Center Model in the Amazon Rainforest
Sileno de Queiroz Fortes-Filho, MD, PhD, et al.
School of Health Sciences, Amazonas State University, and Instituto Metropolitano de Ensino, Amazonas, Brazil
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
A Critical Access Hospital Partners With Community Leadership to Provide Reliable Maternity Care in Rural North Carolina
Many pregnant people in the U.S. cannot access adequate maternity care; minorities and those living in rural areas face particular challenges, including unplanned out-of-hospital births and higher rates of maternal mortality. Chatham Hospital, a critical access hospital in rural Siler City, North Carolina, joined with UNC Family Medicine, the Chatham Health Department, nonprofits, and other local and state organizations to open a Level-1 maternity care center. Siler City has a large Black and Hispanic population compared with the rest of Chatham County. The center’s culturally diverse medical staff includes family physicians with obstetrical and surgical training, an OB/GYN, certified nurse midwives, and certified registered nurse anesthetists. This allows people with low-risk pregnancies to deliver safely and receive supportive care within their own community.
Closing the Gap: How a Community Effort Can Improve Rural Maternity Care
Jesus Ruiz, MD
University of North Carolina at Chapel Hill School of Medicine, Department of Family Medicine, Chapel Hill, NC
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Family Medicine Residents and Faculty Gain Insight Into the Needs of Patients With Diabetes by Wearing Continuous Glucose Monitoring Devices Themselves
In rural Wyoming, where there is limited access to specialized diabetes care, diabetes management usually occurs in a primary care setting. To deepen their understanding of daily challenges faced by patients with diabetes, 35 residents, nurses, and faculty members in the University of Wyoming Family Medicine Residency Program wore continuous glucose monitoring (CGM) devices for 10 days. Using a smartphone app and clinical portal, they logged their food intake and activities to gain relevant experience to guide their patients. This firsthand experience gave them more comprehensive training in how CGM devices work, which in turn improved their ability to educate and engage patients in their own diabetes and prediabetes treatment.
Enhancing Patient-Centered Care Through Firsthand Experience With Continuous Glucose Monitoring in Rural Wyoming
Drew Mahoney, MD
University of Wyoming Family Medicine Residency Program at Cheyenne, Cheyenne, WY
Lavinia Salama, PharmD, BCACP, BC-ADM, CDCES
University of Wyoming Family Medicine Residency Program at Cheyenne; University of Wyoming School of Pharmacy, Laramie, WY
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
Turning Maternal Care Into Lifelong Care for Those Who Need It Most
High-risk pregnancy conditions such as hypertensive disorders of pregnancy (HDP) and gestational diabetes mellitus (GDM) are associated with an increased risk of developing chronic diseases well beyond the first postpartum year. Dr. Carolyn F. Pearce and Dr. Mary Beth Sutter, both family physicians at Brown University’s Warren Alpert Medical School, have seen the impact of pregnancy complications on the long-term health of their patients. In this editorial, they stress how critical it is to connect people with high-risk pregnancies to longitudinal primary care, reiterating the importance of the findings of a study presented by Dr. Jena Wallander Gemkow and colleagues in their article “A Mixed Methods Evaluation of a Quality Improvement Model to Optimize Perinatal and Primary Care in the Community Health Setting.” Dr. Pearce and Dr. Sutter highlight the success of the quality improvement initiative by Wallander Gemkow et al at Federally Qualified Health Centers (FQHCs) in Chicago to coordinate the transition of patients with high-risk pregnancies to postpartum primary care. As America confronts a growing maternal health crisis—one that hits underserved and BIPOC communities particularly hard—they declare that “family doctors, often the backbone of the health care workforce of community health centers, are needed now more than ever in the spectrum of continuity spanning pre-pregnancy, pregnancy, and postpartum.”
From Cradle to Grave: Health During Pregnancy and Over a Lifetime
Carolyn F. Pearce, MD, MPH
The Warren Alpert Medical School at Brown University Department of Family Medicine, Providence, RI
Mary Beth Sutter, MD
The Warren Alpert Medical School at Brown University Department of Family Medicine, Providence, RI
PRE-EMBARGO LINK (Link expires at 5 p.m. EDT Jan. 22, 2024)
PERMANENT LINK
END
Annals of Family Medicine January/February 2024 Tip Sheet
2024-01-22
ELSE PRESS RELEASES FROM THIS DATE:
A quality improvement intervention links high-risk prenatal patients at safety-net health centers with primary care
2024-01-22
Researchers assessed the development and implementation of a quality improvement learning collaborative’s (QILC) intervention to link high-risk prenatal patients with primary care. The aims of the study were twofold: to identify any quantitative impact of the intervention on postpartum and primary care utilization for high-risk prenatal patients and to explore the Federally Qualified Health Center (FQHC) participants’ experiences of working with a QI collaborative.
Using information from patients’ charts and/or ...
A new drug candidate can shrink kidney cysts
2024-01-22
Autosomal dominant polycystic kidney disease (ADPKD), the most common form of polycystic kidney disease, can lead to kidney enlargement and eventual loss of function. The disease affects more than 12 million people worldwide, and many patients end up needing dialysis or a kidney transplant by the time they reach their 60s.
Researchers at MIT and Yale University School of Medicine have now found that a compound originally developed as a potential cancer treatment holds promise for treating ADPKD. The drug works by exploiting kidney cyst cells’ vulnerability to oxidative stress — a state ...
Bone marrow adipocytes provide early sign of progression from MGUS to multiple myeloma
2024-01-22
A new research perspective was published in Oncotarget's Volume 15 on January 16, 2024, entitled, “Bone marrow adipocytes provide early sign for progression from MGUS to multiple myeloma.”
Multiple Myeloma (MM) is the second most common hematological malignancy and is characterized by clonal expansion of malignant plasma cells in the bone marrow. In spite of recent advances in the field of MM, the disease has remained incurable. MM is preceded by a premalignant state known as monoclonal gammopathy of undetermined significance (MGUS), with a risk of progression to MM of 1% per year. Establishing a scalable approach that refines ...
Dr. Blagosklonny’s battle with cancer (Part 1)
2024-01-22
On January 3, 2024, Mikhail V. Blagosklonny M.D., Ph.D., from Roswell Park Comprehensive Cancer Center published a new brief report in Oncoscience (Volume 11), entitled, “My battle with cancer. Part 1.”
“In January 2023, diagnosed with numerous metastases of lung cancer in my brain, I felt that I must accomplish a mission. If everything happens for a reason, my cancer, in particular, I must find out how metastatic cancer can be treated with curative intent. This is my mission now, and the reason I was ever born. In January 2023, I understood the meaning of life, of my life. I was born to write this article. In this article, I argue that monotherapy with ...
Don’t blame the sharks: Research led by UMass Amherst reveals why more hooked tarpon are being eaten
2024-01-22
In wave-making research recently published in Marine and Coastal Fisheries, a team of researchers, led by biologists at the University of Massachusetts Amherst, has quantified the rate at which great hammerhead sharks are eating Atlantic tarpon hooked by anglers at Bahia Honda, Florida—one of the prime tarpon fishing spots in the Florida Keys.
Called the “depredation rate,” the team found that 15.3% of tarpon that were hooked by anglers and fought for more than five minutes were eaten while still on the line. But the researchers also show that this is not necessarily a sign that the ecosystem is out of balance. To the contrary, increased reports ...
Shallow soda lakes show promise as cradles of life on Earth
2024-01-22
Charles Darwin proposed that life could have emerged in a “warm little pond” with the right cocktail of chemicals and energy. A study from the University of Washington, published this month in Communications Earth & Environment, reports that a shallow “soda lake” in western Canada shows promise for matching those requirements. The findings provide new support that life could have emerged from lakes on the early Earth, roughly 4 billion years ago.
Scientists have known that under ...
Computing with the power of light
2024-01-22
The exponential demand for high computing power is far exceeding the capabilities of current electronic systems; however, engineers at the University of Pittsburgh are shining a light on new solutions.
Nathan Youngblood, principal investigator and assistant professor of electrical and computer engineering at Pitt’s Swanson School of Engineering, received a $552,166 Faculty Early Career Development Award from the National Science Foundation (NSF) and a $449,240 award from the Air Force Office of Scientific Research (AFOSR) through its Young Investigator Program (YIP) to continue his pioneering work in phase-change materials and optical computing.
“Dr. ...
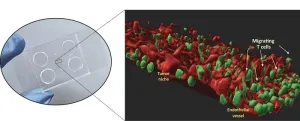
Cholangiocarcinoma: New organ-on-chip aims at accelerating research and personalized medicine
2024-01-22
Milano, January 22nd 2024 – It is only a few centimeters in size and can be held between two fingers, but in the micro-channels carved inside it, it’s hidden a three-dimensional and highly faithful model of a biliary tract cancer called cholangiocarcinoma, complete with its tumor microenvironment. This 3D model is built starting from a sample of patient’s cancer cells and thus it represents a patient-specific "organ-on-chip": a technology made possible only through a multidisciplinary approach that merges biomedicine, physics and engineering.
The innovative prototype is the result ...
Bioengineered material developed to rapidly stop bleeding in patients on blood thinners
2024-01-22
More than 11 million people in the United States take anticoagulation or antiplatelet medications, such as heparin or aspirin, to treat serious conditions like heart attack and stroke. However, these medications also put patients at risk of life-threatening bleeding in the case of injury or during surgery. To improve strategies for reducing blood loss, a team led by investigators from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, developed a porous material that maximizes blood absorption and effectively activates clotting mechanisms, even in patients on anticoagulation or ...
New biomarkers for active lupus nephritis discovered
2024-01-22
New biomarkers with improved diagnostic performance for early detection of lupus nephritis have been discovered in the University of Houston lab of Chandra Mohan, a pioneer in lupus research. Early identification of renal involvement in lupus and prompt treatment are essential in reducing the pain, suffering and eventual mortality it causes.
Systemic Lupus Erythematosus (SLE), commonly called lupus, is an autoimmune disease that occurs when the body attacks its own tissues and organs. Inflammation from the disease can impact many different parts of the body including joints, skin, kidneys, blood cells, brain and heart. Lupus nephritis is one ...