(Press-News.org) Giving high-risk patients access to an obesity specialist through their regular primary care clinic increased their chances of receiving at least one evidence-based weight-management treatment, and led to more weight lost in just a year, a new University of Michigan study finds.
Primary care clinicians commonly struggle to help patients develop an individualized weight-management treatment plan during short clinic visits. Previous U-M research showed that most primary care patients with obesity do not lose at least 5% of their body weight, a goal that’s been shown to reduce obesity-related health risks.
That’s why U-M’s academic medical center, Michigan Medicine, developed the Weight Navigation Program, which teams up patients with obesity and their primary care provider with a board-certified obesity specialist.
The new study evaluating results from it is published in JAMA Network Open by the multidisciplinary team that launched the WNP in fall 2020.
The new study shows that on average, patients who enrolled during the first year of the program lost about 12 pounds, or about 4.4% of their body weight, in the year after they received an individualized obesity treatment plan from an obesity specialist.
That’s compared with very little weight lost by patients similar to the WNP patients who went to a similar U-M primary care clinic that didn’t yet offer the program.
On average, all the patients started with a body mass index (BMI) around 40 kg/m2. To qualify for WNP, patients have to have a BMI above 30 kg/m2 and have at least one weight-related health condition, such as high blood pressure, sleep apnea, type 2 diabetes, or high cholesterol.
Over 40% of those in the WNP lost at least 5% of their body weight, a goal that’s been shown to reduce obesity-related health risks. In comparison, less than 20% of similar patients not in the WNP lost at least 5% of their body weight. In addition, 22% of patients in the WNP lost at least 10% of their body weight compared to less than 4% of similar patients.
The authors say the study suggests that the WNP approach should be tested in a larger clinical trial.
Meanwhile, the WNP is now available to all eligible adult patients who receive primary care through U-M Health clinics, acting as a gateway to multiple treatment options. It’s part of a wide range of weight management programs available by referral in multiple areas of U-M Health.
“The WNP is based in the idea that safe and effective obesity care can be integrated into the primary care settings where most Americans with obesity receive the vast majority of their care,” said Dina Hafez Griauzde, M.D., M.Sc., first author of the study and an internal medicine assistant professor at the U-M Medical School. “Having an obesity specialist work as part of a collaborative team to evaluate patients, help them understand their options, including potential costs, and act as a gateway to specialized care and primary care follow-up, is a model that we hope others will adopt.”
Senior author, Andrew Kraftson, M.D. is an endocrinologist who specializes in obesity medicine But a shortage of such specialists means that programs such as WNP are needed to extend their reach.
The WNP builds on the previous success of other kinds of chronic disease programs that involve closer partnership between specialists and primary care providers. One key difference: two-thirds of current obesity medicine specialists are also primary care physicians, including Griauzde and several of her co-authors.
More about the WNP
Patients referred to the WNP meet with an obesity specialist who has in-depth familiarity with all the obesity treatment options offered at U-M Health as well as community diabetes prevention programs. The obesity specialists also understand insurance coverage and costs such as copays for the different options.
After meeting with the patient, the obesity specialist provides customized treatment recommendations that address the patient’s medical situation, finances, and preferences.
Treatments can range from specialized dietary plans to anti-obesity medications to weight loss surgery. The team monitors progress and coordinates ongoing care with the primary care provider.
More about the study
The new paper tracks the care of 132 people who went through the WNP at a single primary care clinic during the program’s first year, and 132 people with similar health and demographic characteristics who received usual care at a similar U-M Health primary care clinic in that timeframe. Both groups’ records were studied for a full year, and nearly all had weight measurements available at the end of the year.
Two-thirds of both groups were female; the average age was 49 and nearly two-thirds had high blood pressure while about 60% had obstructive sleep apnea and just over 20% had type 2 diabetes.
Of all patients at the clinic offering the WNP who qualified for it, 19% of were referred to it by their primary care provider, and 11% enrolled. This is much higher than the very low percentage of U-M Health primary care patients who received a weight management treatment from their primary care provider or were referred for specialty obesity care in a previous study published by the team based on data from before the WNP launched.
When comparing the WNP patients with the usual care group, WNP patients were more likely to be directed toward health system obesity care resources, with more than twice as many patients in the WNP referred for bariatric surgery evaluations (18% vs. 9%). In all, 4% of the WNP patients had bariatric surgery within a year of starting the program, compared with none of the comparison group.
WNP patients were also much more likely to receive a referral to a program that treats patients through a low-calorie meal replacement plan, or to a program that counsels patients on following a Mediterranean-style diet, which has been shown to have benefits for weight and health.
The percentages receiving a prescription for any obesity medication were similar, at 14% of the WNP patients and 10% of control group patients.
However, the study period was before the U.S. Food and Drug Administration’s approval of semaglutide and tirzepatide for weight management and may not reflect current prescribing practices. Therefore, the researchers are doing a follow-up assessment of weight-management treatment use and patients’ weight loss since the availability of these medications.
In addition to Griauzde and Kraftson, the study’s authors are Cassie D. Turner, LMSW; Amal Othman, MD; Lauren Oshman, MD, MPH; Jonathan Gabison, MD; Patricia K. Arizaca-Dileo, MD; Eric Walford, MD; James Henderson, PhD; Deena Beckius, MPH; Joyce M. Lee, MD, MPH; Eli W. Carter, MPH; Chris Dallas, BBA; Kathyrn Herrera-Theut, MD; Caroline R. Richardson, MD; Jeffrey T. Kullgren, MD, MS, MPH; Gretchen Piatt, PhD, MPH; and Michele Heisler, MD, MPA.
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health, through a pilot grant from the Michigan Center for Diabetes and Translational Research (DK092926), and other grants (DK123416, DK089503, DK020572, DK092926) including funds from the Michigan Nutrition Obesity Research Center, the Michigan Diabetes Research Center and the Elizabeth Weiser Caswell Diabetes Institute.
Multiple authors of the paper are members of the Caswell Diabetes Institute and the U-M Institute for Healthcare Policy and Innovation, as well as being current or former faculty and staff in the Department of Internal Medicine and Family Medicine at the U-M Medical School.
A Primary Care–Based Weight Navigation Program, JAMA Network Open, doi:10.1001/jamanetworkopen.2024.12192
END
Adding obesity experts to primary care clinics improves patients’ weight loss outcomes
Study comparing U-M Weight Navigation Program with usual care for high-risk patients shows higher use of evidence-based treatments and more weight lost
2024-05-21
ELSE PRESS RELEASES FROM THIS DATE:
Detecting odors on the edge: Researchers decipher how insects smell more with less
2024-05-21
Whether it’s the wafting aroma of our favorite meal or the dangerous fumes seeping from a toxic chemical, the human sense of smell has evolved into a sophisticated system that processes scents through several intricate stages. The brains of mammals have billions of neurons at their disposal to recognize odors they are exposed to, from pleasant to pungent.
Insects such as fruit flies, on the other hand, have a mere 100,000 neurons to work with. Yet their survival is dependent upon their ability to decipher the meaning of complex odor mixtures around them to locate food, seek potential mates and avoid predators. Scientists have pondered how insects are able to smell, or extract ...
Recycling carbon dioxide into household chemicals
2024-05-21
A low-cost, tin-based catalyst can selectively convert carbon dioxide to three widely produced chemicals — ethanol, acetic acid and formic acid.
Lurking within the emissions from many industrial operations is an untapped resource — carbon dioxide (CO2). A contributor of greenhouse gas and global warming, it could instead be captured and converted to value-added chemicals.
In a collaborative project involving the U.S. Department of Energy’s (DOE) Argonne National Laboratory, Northern Illinois University and Valparaiso University, ...
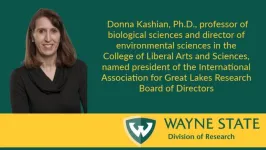
Wayne State faculty member named president of the International Association for Great Lakes Research board
2024-05-21
DETROIT —
The International Association for Great Lakes Research today announced its new board of directors and has named Donna Kashian, Ph.D., professor of biological sciences and director of environmental sciences in the College of Liberal Arts and Sciences at Wayne State University, as president. Kashian previously served as vice president of the board.
Founded in 1967, the International Association for Great Lakes Research is a scientific organization made up of researchers studying the Laurentian Great Lakes, other large lakes of the world and their watersheds, as well as those ...
Consultative support to pediatric primary care providers in providing gender-affirming care
2024-05-21
New Rochelle, NY, May 21, 2024—A new study in the peer-reviewed journal Telemedicine and e-Health found that access to consultative support can increase pediatric primary care provider comfort providing gender-affirming care. Click here to read the article now.
The literature suggests that access to gender-affirming medical care is associated with improved medical outcomes among adolescents who identify as gender diverse or endorse a gender identity that differs from their sex assigned at birth. An increasing number of gender diverse youth seek guidance and support from their pediatric primary care providers (PPCPs), who often lack adequate training in this ...
Alaska’s rusting waters: Pristine rivers and streams turning orange
2024-05-21
Dozens of Alaska’s most remote streams and rivers are turning from a crystal clear blue into a cloudy orange, and the staining could be the result of minerals exposed by thawing permafrost, new research in the Nature journal Communications: Earth and Environment finds.
For the first time, a team of researchers from the National Park Service, U.S. Geological Survey, the University of California, Davis, and other institutions have documented and sampled some of the impaired waters, pinpointing ...
Jefferson Lab director named to 2024 Hampton Roads Power List
2024-05-21
NEWPORT NEWS, VA – Stuart Henderson, director of the U.S. Department of Energy's Thomas Jefferson National Accelerator Facility, has been named to the Hampton Roads Power List by Inside Business. The list recognizes the major players in Hampton Roads’ economy. According to Inside Business, the 2024 list considered milestones and current events, and it features “the talk of Hampton Roads and the change that’s coming.”
“I am honored to be included in this list of people who are moving Hampton ...
New crystal production method could enhance quantum computers and electronics
2024-05-21
Irvine, Calif., May 21, 2024 — In a study published in Nature Materials, scientists from the University of California, Irvine describe a new method to make very thin crystals of the element bismuth – a process that may aid the manufacturing of cheap flexible electronics an everyday reality.
“Bismuth has fascinated scientists for over a hundred years due to its low melting point and unique electronic properties,” said Javier Sanchez-Yamagishi, assistant professor of physics & astronomy at UC Irvine and a co-author of the study. “We developed a new method to make very thin crystals ...
Inherited genes play a larger role in melanoma risk than previously believed
2024-05-21
CLEVELAND - When it comes to skin cancer, most people think of warnings about sunburn and tanning beds. Thoughts of “cancer genes” or inherited risks are reserved for diseases like breast cancer or colon cancer. A new study challenges this status quo by showing that genetics play a larger role in melanoma risk than recognized.
Physicians rarely order genetic screens to assess risk factors for patients with a family history of melanoma because, according to the previous, limited studies, only 2-2.5% of all cases are genetic. For the same reason, insurance companies rarely cover these tests outside of the most extreme ...
Two promising UCF researchers earn 2024 NSF CAREER Awards
2024-05-21
Two Promising UCF Researchers Earn 2024 NSF CAREER Awards
Early-career professors Fan Yao and Li Fang are receiving significant research funding to continue catalyzing their work as part of an annual NSF grant program.
By Eddy Duryea ’13
ORLANDO, May 21, 2024 – UCF assistant professors Li Fang and Fan Yao have been named 2024 U.S. National Science Foundation (NSF) Faculty Early Career Development program (CAREER) award winners. The recipients were awarded funding through five years for their submitted projects.
Fang, who is an assistant professor in UCF’s Department of Physics within the College of Sciences, is using the ...
Study comparing U-M Weight Navigation Program with usual care for high-risk patients shows higher use of evidence-based treatments and more weight lost
2024-05-21
Giving high-risk patients access to an obesity specialist through their regular primary care clinic increased their chances of receiving at least one evidence-based weight-management treatment, and led to more weight lost in just a year, a new University of Michigan study finds.
Primary care clinicians commonly struggle to help patients develop an individualized weight-management treatment plan during short clinic visits. Previous U-M research showed that most primary care patients with ...
LAST 30 PRESS RELEASES:
Brainwaves of mothers and children synchronize when playing together – even in an acquired language
A holiday to better recovery
Cal Poly’s fifth Climate Solutions Now conference to take place Feb. 23-27
Mask-wearing during COVID-19 linked to reduced air pollution–triggered heart attack risk in Japan
Achieving cross-coupling reactions of fatty amide reduction radicals via iridium-photorelay catalysis and other strategies
Shorter may be sweeter: Study finds 15-second health ads can curb junk food cravings
Family relationships identified in Stone Age graves on Gotland
Effectiveness of exercise to ease osteoarthritis symptoms likely minimal and transient
Cost of copper must rise double to meet basic copper needs
A gel for wounds that won’t heal
Iron, carbon, and the art of toxic cleanup
Organic soil amendments work together to help sandy soils hold water longer, study finds
Hidden carbon in mangrove soils may play a larger role in climate regulation than previously thought
Weight-loss wonder pills prompt scrutiny of key ingredient
Nonprofit leader Diane Dodge to receive 2026 Penn Nursing Renfield Foundation Award for Global Women’s Health
Maternal smoking during pregnancy may be linked to higher blood pressure in children, NIH study finds
New Lund model aims to shorten the path to life-saving cell and gene therapies
Researchers create ultra-stretchable, liquid-repellent materials via laser ablation
Combining AI with OCT shows potential for detecting lipid-rich plaques in coronary arteries
SeaCast revolutionizes Mediterranean Sea forecasting with AI-powered speed and accuracy
JMIR Publications’ JMIR Bioinformatics and Biotechnology invites submissions on Bridging Data, AI, and Innovation to Transform Health
Honey bees navigate more precisely than previously thought
Air pollution may directly contribute to Alzheimer’s disease
Study finds early imaging after pediatric UTIs may do more harm than good
UC San Diego Health joins national research for maternal-fetal care
New biomarker predicts chemotherapy response in triple-negative breast cancer
Treatment algorithms featured in Brain Trauma Foundation’s update of guidelines for care of patients with penetrating traumatic brain injury
Over 40% of musicians experience tinnitus; hearing loss and hyperacusis also significantly elevated
Artificial intelligence predicts colorectal cancer risk in ulcerative colitis patients
Mayo Clinic installs first magnetic nanoparticle hyperthermia system for cancer research in the US
[Press-News.org] Adding obesity experts to primary care clinics improves patients’ weight loss outcomesStudy comparing U-M Weight Navigation Program with usual care for high-risk patients shows higher use of evidence-based treatments and more weight lost