By Benjamin Boettner
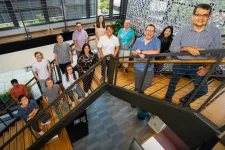
(BOSTON) — Researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard Universityreceived a contract for up to $12M from the Defense Advanced Research Projects Agency (DARPA)’s new SHIELD program. The SHIELD (Synthetic Hemo-technologies to Locate and Disinfect) program aims to develop a prophylactic treatment that can be broadly administered to trauma victims in combat casualty care scenarios to rapidly clear multiple bloodborne bacterial and fungal pathogens, limit morbidity and mortality, and protect recipients for up to seven days.
Blood stream infections (BSIs) can be uniquely challenging in trauma victims who are affected by burn and blast injuries because of the time-consuming process it takes to call out specific pathogens, antibiotic resistance, and the toxicity of certain treatments, especially for fungal infections. The SHIELD program thus asked whether a Roomba-like treatment could be created that circulates in the blood to whisk away pathogens before they can become life-threatening.
The Wyss project proposes an innovative solution for this challenge by combining two key technologies, “FcMBL-mediated pathogen-binding” and “macrophage-activating cellular backpacks” that individually have been extensively validated in multiple medical applications and together could synergistically enable a powerful new approach against infectious pathogens.
“We are thankful to DARPA for launching this Program and selecting us to develop a novel class of therapeutics to defend against a broad range of pathogens. Our goal is to develop a pathogen-agnostic treatment for defending human health in situations when the pathogen identity is unknown or there is insufficient time to identify the pathogen,” said Wyss Core Faculty member Samir Mitragotri, Ph.D., who is the Principal Investigator on the project. Mitragotri also is the Hiller Professor of Bioengineering and Hansjörg Wyss Professor of Biologically Inspired Engineering at the Harvard John A. Paulson School of Applied Sciences and Engineering (SEAS).
Cellular backpacks developed by Mitragotri are micrometer-scale disk-shaped microparticles engineered to quickly and tightly bind to the surface of specific types of immune cells, including macrophages, outside and inside the body, without being engulfed by the cells. Mitragotri’s group showed that, when loaded with slowly released cytokine molecules and bound to macrophages in mice, cellular backpacks could continuously activate the immune cells for days, unleash their tumor cell-killing potential and thus control tumor growth. As an important additional benefit, the close proximity of backpacks to immune cells such as macrophages, also avoids known systemic toxicities of the released cytokines. Beyond cancer applications, Mitragotri and his team have developed easily deployable cellular backpack devices to also control autoimmune disorders such as multiple sclerosis, and as key components of non-invasive diagnostics and therapeutics for “silent” traumatic brain injuries, among other disease targets.
The FcMBL pathogen-binding technology was developed with prior DARPA support by a Wyss team led by Wyss Founding Director Donald Ingber, M.D., Ph.D. and Michael Super, Ph.D, Director of ImmunoMaterials at the Wyss Institute, to enable various pathogen-agnostic therapeutic and diagnostic applications. It consists of a genetically engineered version of the human blood opsonin, Mannose Binding Lectin, which is linked to the Fc portion of an immunoglobulin. After demonstrating that FcMBL bound to more than 130 different types of pathogens, including all major bacterial and fungal species that cause BSI and sepsis, the team engineered fast and effective FcMBL-based pathogen-clearing devices for sepsis, as well as diagnostic assays for use in different infectious disease settings. More recently, the researchers showed that FcMBL-coated liposomes that were loaded with antifungal drugs successfully concentrated the drug at sites of fungal infections to provide enhanced pathogen clearance while preventing unwanted side-effects of antifungals.
“It was a logical step to combine the FcMBL pathogen-binding technology with the cellular backpacks advanced in Professor Samir Mitragotri’s group as this would harness the powers of FcMBL inside the bodies of infected individuals by activating critical cells of the innate immune system that are the body’s first line of defense,” said Super, who was instrumental in conceiving the project with Mitragotri and will coordinate the team effort as a co-investigator on this project.
The FcMBL backpack therapeutics that will be developed under the new DARPA-SHIELD-funded project can be safely and rapidly applied to prevent and treat BSIs in individuals who, due to trauma to various parts of the body, are at high risk of developing sepsis and organ failures and don’t have access to care facilities. FcMBL backpacks, injected directly into the blood circulation, bind to macrophages to keep them activated over days due to a constant stream of backpack-released cytokines. Backpack-carrying macrophages can then patrol the blood stream as well as internal organs, such as the spleen and liver, which are the major natural pathogen-clearance sites, to eliminate pathogens before they can become a threat.
“The beauty of this groundbreaking project is that it combines two extremely powerful technologies that enable pathogen capture and immune cell activation, which synergize with each other when they are assembled into a living pathogen-killing machinery that can patrol inside the bodies of infected individuals. Easily to manufacture, store, and deploy, FcMBL backpacks could save the lives of many by enabling superior pathogen clearance in trauma patients at the site of injury,” said Ingber, who also is also the Judah Folkman Professor of Vascular Biology at HMS and Boston Children’s Hospital, and the Hansjörg Wyss Professor of Biologically Inspired Engineering at SEAS.
PRESS CONTACT
Wyss Institute for Biologically Inspired Engineering at Harvard University
Benjamin Boettner, benjamin.boettner@wyss.harvard.edu
###
The Wyss Institute for Biologically Inspired Engineering at Harvard University (www.wyss.harvard.edu) is a research and development engine for disruptive innovation powered by biologically-inspired engineering with visionary people at its heart. Our mission is to transform healthcare and the environment by developing ground-breaking technologies that emulate the way Nature builds and accelerate their translation into commercial products through formation of startups and corporate partnerships to bring about positive near-term impact in the world. We accomplish this by breaking down the traditional silos of academia and barriers with industry, enabling our world-leading faculty to collaborate creatively across our focus areas of diagnostics, therapeutics, medtech, and sustainability. Our consortium partners encompass the leading academic institutions and hospitals in the Boston area and throughout the world, including Harvard’s Schools of Medicine, Engineering, Arts & Sciences and Design, Beth Israel Deaconess Medical Center, Brigham and Women’s Hospital, Boston Children’s Hospital, Dana–Farber Cancer Institute, Massachusetts General Hospital, the University of Massachusetts Medical School, Spaulding Rehabilitation Hospital, Boston University, Tufts University, Charité – Universitätsmedizin Berlin, University of Zürich, and Massachusetts Institute of Technology.
END