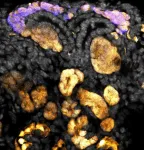
The study, led by researchers at Sylvester Comprehensive Cancer Center, part of the University of Miami Miller School of Medicine, is the first to quantify tumor changes in glioblastoma patients receiving MRI-guided radiation therapy. This novel technique, also known as MRI-linear accelerator or MRI-linac, pairs daily imaging with radiation. Sylvester was the first to use this technology for patients with glioblastoma and remains one of the few cancer centers to offer it for the disease.
The Sylvester researchers found that this daily imaging can serve as an important monitoring system to signal tumor growth during treatment earlier than standard imaging, providing evidence that the method could one day be used to guide rapid treatment adaptation during radiation therapy.
The study was published Sept. 30 in the International Journal of Radiation Oncology – Biology – Physics and simultaneously presented at the American Society for Radiation Oncology (ASTRO) meeting by the study’s first author, Kaylie Cullison, Ph.D., an M.D./Ph.D. student in the Miller School’s Medical Scientist Training Program.
“Our study shows that these daily scans can serve as an early warning sign for potential tumor growth,” Cullison said.
In the study, which was led by Eric A. Mellon, M.D., Ph.D., a radiation oncologist and co-leader of Sylvester’s Neurologic Cancer Site Disease Group, the researchers followed 36 glioblastoma patients over a six-week course of daily radiation and MRI scans using MRI-linac. They then compared the data from these daily scans to standard-of-care imaging to measure tumor size, namely, a single MRI image with contrast performed one week before radiation treatment and another a month after the radiation course is completed. Although MRI-linac could be paired with a contrast agent, some patients are concerned about frequent use of these heavy metals, so the study was conducted without contrast for the daily scans.
Typically, brain radiation is guided by X-ray or CT scan to position the patient correctly under the radiation beam. But these kinds of imaging only reveal the position of the skull.
“Any machine that does not include MRI, which is 99% of radiation-delivery equipment out there, cannot see what's going on inside of the brain,” Mellon said. “MRI-linac allows you to see what’s going on in the brain, for the first time.”
The researchers found that for 74% of the trial participants, their MRI-linac imaging matched the information found in the typical, contrast MRI performed before and after treatment. That is, both modalities agreed on whether the patients’ tumors grew, shrank, or remained the same size during the course of radiation therapy. For the other 26% of patients, the MRI-linac imaging predicted tumor growth while the pre- and post-treatment imaging showed that the tumor shrank.
Although the daily MRI did not agree with the contrast imaging 100% of the time, the fact that it did not miss any cases of true tumor growth suggests that it could be used to signal possible tumor growth during radiation therapy, the researchers said. That signal could then be confirmed with contrast imaging and, ultimately, could be used to adapt the patient’s treatment to more quickly address the tumor growth.
The daily imaging could also be useful in other cases besides tumor growth. If a tumor is shrinking, the radiation field could be narrowed to ensure only cancerous tissue is targeted. Additionally, most glioblastoma patients undergo surgery before radiation therapy, and the site where the tumor was removed, the surgical resection cavity, often shrinks as the brain heals. Following that shrinkage over time and changing the radiation therapy accordingly could be critical to spare healthy tissue from irradiation. In their current study, the Sylvester researchers traced changes in both the tumor size and surgical cavity size.
Mellon and his team plan to conduct future studies to test MRI-linac’s ability to guide treatment decisions for glioblastoma patients during the course of radiation therapy as well as to test the method in other types of brain cancer. Because so few clinics use the technology to treat brain cancers, it was not realized prior to Mellon’s studies that glioblastomas change significantly during radiation. The research team hopes to use that knowledge to improve outcomes for patients with this all-too-often deadly form of cancer.
about this important research on the InventUM Blog and follow @SylvesterCancer on X for the latest news on its research and care.
# # #
PHOTO CAPTION/CREDIT: The study, led by Eric A. Mellon, M.D., Ph.D. and Kaylie Cullison, Ph.D., at Sylvester Comprehensive Cancer Center, is the first to quantify tumor changes in glioblastoma patients receiving MRI-guided radiation therapy. This novel technique, also known as MRI-linear accelerator or MRI-linac, pairs daily imaging with radiation. Sylvester was the first to use this technology for patients with glioblastoma and remains one of the few cancer centers to offer it for the disease. Photo by Sylvester.
# # #
Authors: In addition to Cullison and Mellon, authors from Sylvester, the University of Miami and/or the University of Miami Miller School of Medicine include Kayla Samimi, Jonathan B. Bell, Danilo Maziero, Alessandro Valderrama, Adrian L. Breto, Kolton Jones, Macarena I. De La Fuente, Gregory Kubicek, Jessica Meshman, Gregory A. Azzam, John C. Ford and Radka Stoyanova. Maziero is also affiliated with UC San Diego Health. Jones is also affiliated with West Physics, Atlanta.
Funding: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award numbers R37CA262510, P30CA240139, K12CA226330, and F30CA278357, and the National Center for Advancing Translational Sciences of the National Institutes of Health/Miami Clinical and Translational Science Institute under award number UL1TR002736. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Aspects of this study were presented in an oral presentation at the American Society for Radiation Oncology (ASTRO) Annual Meeting in October 2022.
Disclosures: D.M., former employee of the University of Miami and current medical physics resident at UC San Diego Health, was a paid consultant for ViewRay and received honoraria totaling $3,000 in 2021–2022. He has no other personal financial interests in this work. J.C.F., employee of the University of Miami, was a paid consultant for ViewRay, received no funds related to this work, and has no financial interests in this work. E.A.M., employee of the University of Miami, has been funded under a United States National Cancer Institute Academic-Industrial Partnership grant (R37CA262510) for this and related work. In 2022, he received support totaling $2,235.01 from ViewRay for travel attendance at ViewRay sponsored workshops related to this and similar work. He has no other personal financial interests in this work. ViewRay and other funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. For all other authors (K.C., K.S., J.B.B., A.V., A.L.B., K.J., M.I.D., G.K., J.M., G.A.A., and R.S.), there are no conflicts of interest to declare.
Article: “Dynamics of Daily Glioblastoma Evolution During Chemoradiotherapy on the 0.35T MRI-Linear Accelerator”
DOI: 10.1016/j.ijrobp.2024.09.028
# # #
END