(Press-News.org) Patients in emergency departments who are treated by physicians with a high propensity to admit those they see into the hospital are more likely to be discharged after only a short stay, suggesting a possible unnecessary admission, while they are no less likely to die, new research suggests.
The findings suggest that differences in physicians’ skill or risk aversion may come into play when they make admitting decisions, said Dr. Dan Ly, assistant professor of medicine in the division of general internal medicine and health services research at the David Geffen School of Medicine at UCLA.
“Physicians, just like professionals in other domains, differ in their abilities and decisions, which has consequences for how much care you might receive, including, in this case, your likelihood of being hospitalized,” said Ly, who co-authored the paper with Stephen Coussens, a health economist and senior data scientist at the Washington state-based data management company Abett. “Some physicians may order more tests and hospitalize more of their patients, but this doesn't appear to translate to better health.”
The findings will be published in the peer-reviewed JAMA Internal Medicine.
While previous studies have shown great variation in emergency department physicians’ likelihood of admitting a patient to the hospital, there has been little evidence whether and how this affects patient outcomes.
Using electronic health records from Veterans Affairs for January 2011 through December 2019, the researchers compared physicians practicing within the same emergency department. Their cross-sectional study captured data for 2,100 physicians in 105 emergency departments across the U.S. comprising more than 2.1 million patient visits. They focused on patients coming into the emergency department for chest pain, shortness of breath, or abdominal pain.
About 41% of the visits led to hospital admission, with 19% of those patients discharged in less than 24 hours. Variation in admission rates varied greatly. For example, patients who saw high-admitting physicians (those in the 90th percentile) were almost twice as likely to be admitted as patients who were treated by low-admitting physicians (those in the 10th percentile), even though their underlying health did not differ. Overall, about 2.5% of patients died within 30 days. The researchers found no relationship between a physician’s admission rate and the 30-day mortality rate of their patients. This lack of relationship was also true for 7-day, 14-day, 90-day, and one-year mortality.
The findings suggest that differences across physicians in admission rates are driven less by a patient’s underlying health than variation in physician decision-making, the researchers write. In addition, these additional hospitalizations from high-admitting physicians led neither to short-term protection from severe outcomes nor to a reduction in patients’ risk for dying for up to a year afterward. And patients who were treated by physicians with a lower propensity to admit spent less total time after their ED visit in the hospital, which suggests that low-propensity physicians were not simply deferring a necessary hospitalization into the future, they write.
Limitations of the study include the possibility that some potential clinical confounders were not captured in the electronic health records; the manner that the researchers used to measure patients’ health prior to the emergency department visit, called the Elixhauser Comorbidity Index score, does not measure the severity of a person’s presenting condition; variations in physician characteristics, such as medical training, could not be controlled for; the findings are specific to the VA, whose patients are largely male, and has emergency department staffing with more non-emergency medicine trained physicians, so the findings may not be applicable to other institutions; and other factors besides the physician also play a role in variation in admission rates.
While more research is needed to fully understand these differences in admission rates, “our study is able to better account for patient differences and make apples-to-apples comparisons between physicians to demonstrate true differences in ED physician practice patterns and show that these differences do not translate to better patient health outcomes,” Ly said.
The study was funded in part by the Veterans Affairs Health Systems Research Center for the Study of Healthcare Innovation Implementation & Policy Locally Initiated Project. (LIP 65-175)
Article: “Variation in Emergency Department Physician Admitting Practices and Subsequent Mortality,” doi: 10.1001/jamainternmed.2024.6925
Patients in emergency departments who are treated by physicians with a high propensity to admit those they see into the hospital are more likely to be discharged after only a short stay, suggesting a possible unnecessary admission, while they are no less likely to die, new research suggests.
The findings suggest that differences in physicians’ skill or risk aversion may come into play when they make admitting decisions, said Dr. Dan Ly, assistant professor of medicine in the division of general internal medicine and health services research at the David Geffen School of Medicine at UCLA.
“Physicians, just like professionals in other domains, differ in their abilities and decisions, which has consequences for how much care you might receive, including, in this case, your likelihood of being hospitalized,” said Ly, who co-authored the paper with Stephen Coussens, a health economist and senior data scientist at the Washington state-based data management company Abett. “Some physicians may order more tests and hospitalize more of their patients, but this doesn't appear to translate to better health.”
The findings will be published in the peer-reviewed JAMA Internal Medicine.
While previous studies have shown great variation in emergency department physicians’ likelihood of admitting a patient to the hospital, there has been little evidence whether and how this affects patient outcomes.
Using electronic health records from Veterans Affairs for January 2011 through December 2019, the researchers compared physicians practicing within the same emergency department. Their cross-sectional study captured data for 2,100 physicians in 105 emergency departments across the U.S. comprising more than 2.1 million patient visits. They focused on patients coming into the emergency department for chest pain, shortness of breath, or abdominal pain.
About 41% of the visits led to hospital admission, with 19% of those patients discharged in less than 24 hours. Variation in admission rates varied greatly. For example, patients who saw high-admitting physicians (those in the 90th percentile) were almost twice as likely to be admitted as patients who were treated by low-admitting physicians (those in the 10th percentile), even though their underlying health did not differ. Overall, about 2.5% of patients died within 30 days. The researchers found no relationship between a physician’s admission rate and the 30-day mortality rate of their patients. This lack of relationship was also true for 7-day, 14-day, 90-day, and one-year mortality.
The findings suggest that differences across physicians in admission rates are driven less by a patient’s underlying health than variation in physician decision-making, the researchers write. In addition, these additional hospitalizations from high-admitting physicians led neither to short-term protection from severe outcomes nor to a reduction in patients’ risk for dying for up to a year afterward. And patients who were treated by physicians with a lower propensity to admit spent less total time after their ED visit in the hospital, which suggests that low-propensity physicians were not simply deferring a necessary hospitalization into the future, they write.
Limitations of the study include the possibility that some potential clinical confounders were not captured in the electronic health records; the manner that the researchers used to measure patients’ health prior to the emergency department visit, called the Elixhauser Comorbidity Index score, does not measure the severity of a person’s presenting condition; variations in physician characteristics, such as medical training, could not be controlled for; the findings are specific to the VA, whose patients are largely male, and has emergency department staffing with more non-emergency medicine trained physicians, so the findings may not be applicable to other institutions; and other factors besides the physician also play a role in variation in admission rates.
While more research is needed to fully understand these differences in admission rates, “our study is able to better account for patient differences and make apples-to-apples comparisons between physicians to demonstrate true differences in ED physician practice patterns and show that these differences do not translate to better patient health outcomes,” Ly said.
The study was funded in part by the Veterans Affairs Health Systems Research Center for the Study of Healthcare Innovation Implementation & Policy Locally Initiated Project. (LIP 65-175)
Article: “Variation in Emergency Department Physician Admitting Practices and Subsequent Mortality,” DOI: 10.1001/jamainternmed.2024.6925
END
Emergency department physicians vary widely in their likelihood of hospitalizing a patient, even within the same facility
Patients hospitalized by physicians with higher admission rates likelier to be discharged within 24 hours but no less likely to die than patients hospitalized by physicians with lower admission rate
2024-12-23
ELSE PRESS RELEASES FROM THIS DATE:
Firearm and motor vehicle pediatric deaths— intersections of age, sex, race, and ethnicity
2024-12-23
About The Study: In this cross-sectional study, U.S. youths ages 0 to 19 years experienced important disparities in firearm and motor vehicle crash fatality rates and increases over time when considering the intersectionality by age group, sex, race, and ethnicity. These findings suggest that a multipronged strategy focused on individual, community, and policy level approaches for specific high-risk groups for each injury mechanism is necessary to address these leading causes of death in U.S. youths.
Corresponding Author: To contact the corresponding author, Lois K. Lee, MD, MPH, email lois.lee@childrens.harvard.edu.
To access the embargoed study: Visit ...
Association of state cannabis legalization with cannabis use disorder and cannabis poisoning
2024-12-23
About The Study: In this longitudinal cohort study, medical cannabis laws were associated with increased cannabis use disorder and cannabis poisoning diagnoses, and recreational cannabis laws were associated with increased cannabis poisoning in adults ages 18 to 64 with employer-sponsored health insurance. Communities with increased access to cannabis may experience increased health care use and costs due to increases in cannabis poisoning and cannabis use disorder, and new clinical and policy interventions are needed to curb these rising diagnoses.
Corresponding ...
Gestational hypertension, preeclampsia, and eclampsia and future neurological disorders
2024-12-23
About The Study: In this study, gestational hypertension, preeclampsia, and eclampsia were associated with an increased risk of new-onset migraine, headache, epilepsy, sleep disorder, or mental fatigue within months to years after giving birth. Guidelines recommend follow-up after delivery for women with gestational hypertension and preeclampsia for their increased risk of cardiovascular disease. At these visits, caregivers should also pay attention to persisting or new-onset of neurological symptoms, since this group of women ...
Adoption of “hospital-at-home” programs remains concentrated among larger, urban, not-for-profit and academic hospitals
2024-12-23
Hospitals that have adopted the Center for Medicare and Medicaid (CMS) “hospital-at-home” program, which serves as an alternative to admission to brick-and-mortar facilities, are concentrated in large, urban, not-for-profit, and academic hospitals, new research suggests.
The findings are among the first to portray the landscape of hospitals participating in this rapidly growing care model, said Dr. Hashem Zikry, a participant in the National Clinician Scholars Program at UCLA and lead author on the paper, which will be published in the peer-reviewed JAMA.
“If CMS’ goal is to continue to expand hospital-at-home, these findings suggest ...
Unlocking the mysteries of the human gut
2024-12-23
When making decisions about nutrition and diet, the focus is often on the potential impacts to the heart or brain; and gut health can frequently end up an afterthought despite a whole industry revolving around probiotics and digestive aids. With its direct link to those two important organs, should gut health be prioritized more?
Imagine an entire civilization of trillions of microorganisms living in harmony inside of your digestive system. This microbiome is unique to each individual and varies greatly based on many genetic and environmental factors. The complexity of gut health can often make diagnosis of maladies difficult, especially when new ...
High-quality nanodiamonds for bioimaging and quantum sensing applications
2024-12-23
Quantum sensing is a rapidly developing field that utilizes the quantum states of particles, such as superposition, entanglement, and spin states, to detect changes in physical, chemical, or biological systems. A promising type of quantum nanosensor is nanodiamonds (NDs) equipped with nitrogen-vacancy (NV) centers. These centers are created by replacing a carbon atom with nitrogen near a lattice vacancy in a diamond structure. When excited by light, the NV centers emit photons that maintain stable spin information ...
New clinical practice guideline on the process for diagnosing Alzheimer’s disease or a related form of cognitive impairment or dementia
2024-12-23
Key Takeaways
An expert workgroup representing primary and specialty care has developed new guidelines for comprehensive evaluation of patients who may have cognitive impairment or dementia due to Alzheimer’s disease or a related disease. Current guidelines for a comprehensive evaluation process are more than 20 years old.
Results of the evaluation should be a three-step diagnostic formulation, summarizing the patient’s overall level of impairment, a brief summary of the symptoms they are experiencing, and the likely underlying brain disease(s) and/or conditions contributing to their ...
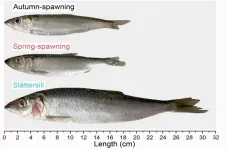
Evolution of fast-growing fish-eating herring in the Baltic Sea
2024-12-23
Atlantic and Baltic herring are typical plankton-eating fish of central importance for the northern Atlantic Ocean and Baltic Sea ecosystems. A new study published in Nature Communications led by scientists from Uppsala University (Sweden) documents the discovery of the evolution of genetically distinct, fish-eating herring in the Baltic Sea, a young water body that has only existed since the end of the last glaciation.
Atlantic and Baltic herring have a key role in the ecosystem, acting as a critical link between plankton production and other organisms, like predatory fish, sea birds, sea mammals, and humans. Previous research from the Uppsala group has documented that herring is subdivided ...
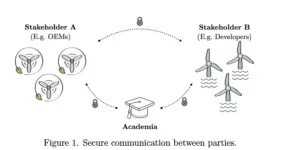
Cryptographic protocol enables secure data sharing in the floating wind energy sector
2024-12-23
Floating wind power offers enormous potential for deepwater offshore energy development. However, the management and secure exchange of data between stakeholders represents a key challenge for its evolution. A new cryptographic framework, proposed by researchers Claudia Bartoli (IMDEA Software) and Irene Rivera-Arreba (Norwegian University of Science and Technology, NTNU), presented at WindTech 2024 Conference, tries to solve this problem with a data sharing scheme that guarantees data integrity without compromising privacy. This breakthrough seeks to foster collaboration between industries and academia, driving innovation in floating wind technologies.
Context
Floating wind power ...
Can drinking coffee or tea help prevent head and neck cancer?
2024-12-23
In a recent analysis of data from more than a dozen studies, coffee and tea consumption was linked with lower risks of developing head and neck cancer, including cancers of the mouth and throat. The findings are published by Wiley online in CANCER, a peer-reviewed journal of the American Cancer Society.
Head and neck cancer is the seventh most common cancer worldwide, and rates are rising in low- and middle-income countries. Many studies have assessed whether drinking coffee or tea is associated with head and neck cancer, with inconsistent results.
To provide additional insight, investigators examined data from 14 studies by different scientists associated with the International Head and ...
LAST 30 PRESS RELEASES:
Towards tailor-made heat expansion-free materials for precision technology
New research delves into the potential for AI to improve radiology workflows and healthcare delivery
Rice selected to lead US Space Force Strategic Technology Institute 4
A new clue to how the body detects physical force
Climate projections warn 20% of Colombia’s cocoa-growing areas could be lost by 2050, but adaptation options remain
New poll: American Heart Association most trusted public health source after personal physician
New ethanol-assisted catalyst design dramatically improves low-temperature nitrogen oxide removal
New review highlights overlooked role of soil erosion in the global nitrogen cycle
Biochar type shapes how water moves through phosphorus rich vegetable soils
Why does the body deem some foods safe and others unsafe?
Report examines cancer care access for Native patients
New book examines how COVID-19 crisis entrenched inequality for women around the world
Evolved robots are born to run and refuse to die
Study finds shared genetic roots of MS across diverse ancestries
Endocrine Society elects Wu as 2027-2028 President
Broad pay ranges in job postings linked to fewer female applicants
How to make magnets act like graphene
The hidden cost of ‘bullshit’ corporate speak
Greaux Healthy Day declared in Lake Charles: Pennington Biomedical’s Greaux Healthy Initiative highlights childhood obesity challenge in SWLA
Into the heart of a dynamical neutron star
The weight of stress: Helping parents may protect children from obesity
Cost of physical therapy varies widely from state-to-state
Material previously thought to be quantum is actually new, nonquantum state of matter
Employment of people with disabilities declines in february
Peter WT Pisters, MD, honored with Charles M. Balch, MD, Distinguished Service Award from Society of Surgical Oncology
Rare pancreatic tumor case suggests distinctive calcification patterns in solid pseudopapillary neoplasms
Tubulin prevents toxic protein clumps in the brain, fighting back neurodegeneration
Less trippy, more therapeutic ‘magic mushrooms’
Concrete as a carbon sink
RESPIN launches new online course to bridge the gap between science and global environmental policy
[Press-News.org] Emergency department physicians vary widely in their likelihood of hospitalizing a patient, even within the same facilityPatients hospitalized by physicians with higher admission rates likelier to be discharged within 24 hours but no less likely to die than patients hospitalized by physicians with lower admission rate