Media Contact:
Michael E. Newman,
mnewma25@jhmi.edu
Even as the first vaccines for SARS-CoV-2, the virus that causes COVID-19, are being distributed, scientists and clinicians around the world have remained steadfast in their efforts to better understand how the human immune system responds to the virus and protects people against it. Now, a research team -- led by Johns Hopkins Medicine and in collaboration with ImmunoScape, a U.S.-Singapore biotechnology company -- has published one of the most comprehensive characterizations to date of a critical contributor to that protection: the response of immune system cells called T lymphocytes (more commonly known as T cells) in people who have recovered from SARS-CoV-2 infection.
The researchers, whose findings were posted online Jan. 11, 2021, in The Journal of Clinical Investigation, say that better defining which T cells interact with which specific portions of the SARS-CoV-2 virus -- as well as how those interactions can provide long-lasting immunity against COVID-19 -- may help spur development of the next generation of vaccines.
"We already knew that plasma from convalescent patients with COVID-19 -- those who have recovered from a SARS-CoV-2 infection -- can contain antibodies that neutralize the virus, which can then be used to help other patients with active infection," says study senior author Thomas Quinn, M.D., professor of medicine at the Johns Hopkins University School of Medicine and National Institutes of Health distinguished investigator at the National Institute of Allergy and Infectious Diseases. "Our study was designed to assess which T cells react to specific proteins of SARS-CoV-2, how they might complement neutralizing antibodies in recovery from infection and what can be done to optimize the process for long-term protection."
The T cells of interest to Quinn and his colleagues are known as CD8+ T cells, also called cytotoxic or killer T cells for their ability to eliminate foreign invaders such as bacteria and viruses from the body. To analyze them, the researchers collected blood samples from 30 convalescent patients who had recovered from mild cases of COVID-19. The six human leukocyte antigens (HLAs, as they are more commonly known, are cell-surface proteins that regulate the immune system and are part of each person's genetic profile) of the donors studied, Quinn says, are representative of some 73% of the continental U.S. population, meaning the study results have broad significance.
The samples were taken from 26 to 62 days after the donors stopped having COVID-19 symptoms, so that "their immune response would be fully matured in response to the virus and have primed certain CD8+ T cells against it," says Quinn. The Johns Hopkins Medicine researchers measured the level of neutralizing antibodies in the donors at various times post-recovery and stored samples for deeper analysis.
That assessment occurred when the donor samples were sent to ImmunoScape for the difficult task of identifying which T cells had responded to SARS-CoV-2. More specifically, the company's deep immune cell profiling method could show toward which virus proteins the T cells directed that response -- data that could provide valuable insight into the T cells' functional properties.
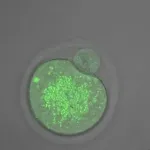
In a first-of-its-kind analysis, the ImmunoScape team used its highly sensitive HLA-SARS-CoV-2 tetramers -- laboratory-produced proteins that bind exclusively to their T cell targets -- to tag and identify the types of virus-recognizing CD8+ T cells. The samples were probed with 408 SARS-CoV-2 epitopes -- proteins that may elicit an immune response -- from the spikes on the virus surface, from the virus capsule and from nonstructural proteins inside the virus. The researchers then looked to see which T cells matched up with which epitopes.
"We found that 52 of the 408 epitopes were recognized by the T cells from the convalescent donors, with 18 of these epitope matchings previously unreported," says study co-author Aaron Tobian, M.D., Ph.D., director of the transfusion medicine division and professor of pathology at the Johns Hopkins University School of Medicine. "Of these, 23% were derived from spike proteins -- the types targeted by the currently available COVID-19 vaccines -- while 14% were from capsule proteins and 63% were from nonstructural proteins that normally would not elicit an immune response."
Looking at the specific types of CD8+ T cells present at different times following recovery from COVID-19, the researchers found that as the levels of neutralizing antibodies increased in the convalescent plasma, so did the number of memory CD8+ T cells that recognized SARS-CoV-2 epitopes.
"That's good because those are the T cells you want to be primed in case you are exposed to SARS-CoV-2 a second time as they 'remember' the first infection and quickly direct the immune system to fight the virus before it takes root again," says Quinn.
Characterizing the CD8+ T cells in blood samples from convalescent patients that are specific to SARS-CoV-2 and, more importantly, specific to which viral epitopes, is an important achievement, Tobian adds.
"With this knowledge, we will be better equipped to design COVID-19 vaccines that produce a strong immune response and likely provide years of defense against SARS-CoV-2," he says.
Quinn and Tobian are available for interviews.
JOHNS HOPKINS MEDICINE RESEARCHER PART OF TEAM THAT QUANTIFIED 'PANDEMIC FATIGUE'
Media Contact:
Danny Jacobs,
djacob41@jhmi.edu
Anecdotal evidence of "pandemic fatigue" -- defined by the World Health Organization as "a lack of motivation to follow recommended COVID-19 protection behaviors" -- has been reported and shared almost as long as physical distancing guidelines have been around to fight the spread of the disease. Now, a research team, including a Johns Hopkins medical student, has the data to prove it.
The researchers analyzed almost nine months of survey responses to the University of Southern California's Understanding America Study, during which, twice each month, nearly 8,000 people across the United States were asked if they were practicing nonpharmaceutical interventions (NPIs), including physical distancing, frequent handwashing and wearing a mask.
The researchers used the data to develop a national NPI adherence index, detailed in a research letter published Jan. 22, 2021, in the Journal of the American Medical Association. The index, they report, started at 70 (out of 100, which would be total adherence) in early April 2020, dropped and plateaued in the high 50s in June, and increased slightly to 60 by Thanksgiving. The decrease was consistent across every region in the country.
"The plateau we see for overall NPI adherence in the results likely reflects some stability in the risk perception of different activities," says study lead author Matthew Crane, a second-year medical student at the Johns Hopkins University School of Medicine. "It's good to see adherence isn't continuing to drop at the initial rate because that would be terrible. But it's also disconcerting that protective behaviors overall have become relatively stable no matter what the national state of COVID-19 prevalence is. Given new, more transmissible variants of the virus that are arising globally, we really might need greater adherence to keep people safe."
The NPIs that had the largest decreases were remaining at home except for essential activities and exercise (79.6% of respondents did so in April 2020 compared with 41.1% by November), having no close contact with non-household members (63.5% decreased to 37.8%), not having visitors at their homes (80.3% decreased to 57.6%) and avoiding eating at restaurants (87.3% decreased to 65.8%).
"I was surprised [NPI adherence] wasn't more responsive to surges in COVID-19 cases," Crane says. "I thought it would fluctuate based on headlines and public health advisories."
The biggest increase was in mask wearing, which went from 39.2% to 88.6%. But Crane notes the survey asks if respondents have done or not done a specific action in the last seven days. That means a person might have worn a mask because it was required to visit a grocery store or another public space but was still opposed in principle to the rule.
"It might not be an endorsement of mask wearing," Crane says.
Crane hopes to continue to track NPI adherence and break down the survey data further, providing more insight for public health professionals to create targeted messaging to change behaviors.
"Until vaccines are very widely distributed, these protective behaviors will be the cornerstone of our national response. It's really what is going to get us through this, the NPIs," he says.
Crane is available for interviews.
MACHINE LEARNING TOOL GIVES EARLY WARNING OF CARDIAC ISSUES FOR PATIENTS WITH COVID-19
Media Contact:
Danny Jacobs,
djacob41@jhmi.edu
A team of Johns Hopkins University biomedical engineers and Johns Hopkins Medicine heart specialists have developed an algorithm that warns doctors several hours before patients hospitalized with COVID-19 experience cardiac arrest or blood clots.
The COVID-HEART predictor can forecast cardiac arrest for patients who have COVID-19 with a median early warning time of 18 hours, and it can predict blood clots three days in advance. It was developed with data from 2,178 patients treated at the five hospitals in the Johns Hopkins Health System between March 1 and Sept. 27, 2020.
"It's an early warning system to predict in real time these two outcomes in hospitalized COVID patients," said study senior author Natalia Trayanova, M.S., Ph.D., the Murray B. Sachs Professor of Biomedical Engineering and Medicine at the Johns Hopkins University School of Medicine. "The continuously updating predictor can help hospitals allocate the appropriate resources and proper interventions to attain the best outcomes for patients."
The paper was posted online Jan. 10, 2021, on the preprint website MedRxiv where scientists have been sharing urgent research related to COVID-19 throughout the pandemic. Trayanova's lab began the research in April 2020 with one of the first grants awarded from the National Science Foundation's Rapid Response Research effort.
Julie Shade, the study's lead author and a doctoral student in biomedical engineering at The Johns Hopkins University, built the machine-learning algorithm with more than 100 clinical data points, demographic information and laboratory results obtained from the JH-CROWN registry that Johns Hopkins established to collect COVID-19 data from every patient in the hospital system. Shade added other variables that she found reported by doctors on Twitter and from other preprint papers.
For example, the team did not anticipate that electrocardiogram (ECG) data would play a critical role in the prediction of blood clotting. But once it was added, the ECG data became one of the most accurate indicators for the condition, Trayanova said.
The researchers' next step is to develop the best method for setting up the technology in hospitals to aid in the care of patients with COVID-19.
Trayanova is available for interviews.
STUDY SHOWS PANDEMIC STRESS AFFECTS HOW PARENTS FEED THEIR CHILDREN
Media Contact:
Waun'Shae Blount,
wblount1@jhmi.edu
The COVID-19 pandemic has dramatically affected the lives of families everywhere. Household routines have changed, with families forced to spend more time than usual at home. School-aged children may have to prepare their own snacks and meals in between virtual classes, and parents might have less time to cook family meals because of their work-from-home schedules. Also, some parents have lost income, reducing family food budgets and changing the ability to afford healthy foods.
Johns Hopkins Medicine researchers surveyed families across the United States to learn how stress related to the pandemic is affecting the ways parents feed their children and in turn, what the children are eating.
A report on the findings was posted online as part of the journal Appetite's January 2021 special issue about COVID-19 impacts on food intake, appetite and weight status.
"Providing healthy meals and snacks to our kids can be a challenge even when we're not experiencing a pandemic," says study senior author Susan Carnell, Ph.D., associate professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine. "The pandemic has massively disrupted families and caused a lot of stress, and this has naturally affected interactions around food."
In the Johns Hopkins Medicine study, 318 parents of children ages 2-12 answered survey questions about interactions with their children regarding meals and snacks, and their youngsters' diets during the pandemic. During the survey, parents were asked about stress related to the COVID-19 pandemic, pre-COVID-19 stress, financial stress (e.g. food insecurity), their feeding practices as parents and how frequently children ate snacks.
The results showed that parents who reported higher levels of stress due to the pandemic also were more likely to use food to manage children's emotions and behaviors. For example, they might offer less nutritious food and snacks, such as cookies, as rewards. These findings are consistent with those of previous research studies showing that parental stress levels and a family's inadequate access to food impact the behaviors of parents when feeding their kids. COVID-19-specific stress also was linked to children eating more sweet and savory snacks throughout the day.
However, other results suggest positive effects of pandemic disruption. For example, the researchers say that 75% of families reported their children had regular breakfast, lunch and dinner times, and less consistent snack times. Lower reported stress also was associated with consistent mealtimes and routines, and positive interactions regarding food, such as parents eating or engaging with their children around mealtimes. This, the researchers say, likely reflects the effects of parents and children spending more time at home and having more chances to interact regarding food.
"The pandemic seems to have produced both negative and positive impacts on food parenting practices," says study lead author Elena Jansen, Ph.D., a postdoctoral fellow in psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine. "We look forward to learning how new routines will become habitual as the pandemic progresses."
To help ensure healthier children during the COVID-19 pandemic and beyond, the researchers recommend that parents follow proven practices, such as establishing regular meal times, involving children in meal preparation, arranging to eat together as a family without television and other distractions, modeling healthy eating habits for children, and being responsive to the hunger and fullness levels of their children when offering food.
The researchers say their ongoing research across socioeconomically diverse families will investigate how parent-child mealtime interactions and child snack intake evolve as the pandemic continues and eventually resolves.
Carnell and Jansen are available for interviews.
INFORMATION: