Details on the findings of this study are found in the article "Second window ICG predicts gross-total resection and progression-free survival during brain metastasis surgery," published today in the Journal of Neurosurgery (https://thejns.org/doi/10.3171/2020.8.JNS201810).
Background
The most common brain tumors are metastatic lesions, primarily those arising from cancers of the lung, breast, and colon, and from melanoma. These lesions pose increased challenges to the cancer patient, including neurological dysfunction and pain. Suggested treatments for metastatic lesions include surgery, stereotactic radiosurgery, and radiation therapy.
In the study described in this paper, the focus was on surgical removal of the metastatic lesion. Surgery can rapidly restore patients' neurological function and reduce the chance of local recurrence.
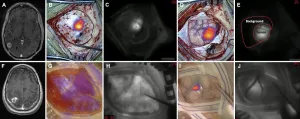
The aim of gross-total resection is complete removal of the pathological lesion. To accomplish this, the surgeon has to be able to see the tumor in its entirety and be able to remove all of it. Various preoperative and intraoperative imaging techniques have been developed over the years to aid in gross-total resection, including fluorescence-guided surgery. During this surgery, a fluorescent dye is applied to the area of resection to highlight the tumor. With the aid of a near-infrared (NIR) camera system, the surgeon can see the tumor glow, making it easier to differentiate the lesion from healthy brain tissue than using normal white light.
Indocyanine green (ICG) is a fluorescent dye used in medical diagnostics. Administered intravenously, ICG often is used to measure blood flow and organ function. ICG has a short half-life and is eliminated from the body fairly quickly. Despite the short half-life, recent studies have shown significant accumulation and a longer retention time for this dye in intracranial tumors than is found in adjacent normal brain parenchyma.
Taking advantage of the long retention of ICG in tumor tissues, the authors used what they call the second window ICG (SWIG) technique, in which a high dose of ICG is administered intravenously 24 hours before surgery. The dye leaks into the tumor, where it is retained, while over this time period normal tissues clear the dye from the rest of the body. In previous studies, the authors found this technique to be an effective way to highlight cranial tumors, including metastatic lesions, which have not proved to be easy to enhance using other fluorescent compounds.
The Present Study
In the present study, the authors' goals were to evaluate the effectiveness of using SWIG at drug concentrations of 5 mg/kg and 2.5 mg/kg (higher than the FDA-approved limit of 2 mg/kg) to identify brain metastases and predict patients' clinical outcomes.
Patients underwent surgery with SWIG between October 2014 and May 2019; clinical outcomes up to April 2020 were reviewed. Forty-seven patients (34 women and 13 men) harboring 51 metastatic lesions were included in the study analyses; 26 patients received 5-mg/kg ICG infusions and 21 received 2.5-mg/kg ICG infusions.
In the operating room, NIR imaging with SWIG was performed four times: 1) following removal of the skull bone but before opening of the dura mater ("dura view"); 2) after durotomy ("cortex view"); 3) once the gross tumor was fully exposed ("tumor view"); and 4) at the end of surgery and before closing ("final view"). The resulting NIR images were analyzed to quantify ICG fluorescence by calculating signal-to-background ratios.
All 51 metastatic lesions displayed NIR fluorescence following SWIG administration. The authors found that an ICG dose of 5 mg/kg was significantly more effective at defining tumors in the dura view than a dose of 2.5 mg/kg (92% vs. 53% of tumors, respectively). Once the dura had been removed and the cortex view reached, however, both doses of ICG were highly effective at delineating tumors (96% of tumors for the 5-mg/kg dose and 93% for the 2.5-mg/kg dose).
At tumor view, the tumor's full shape fluoresced with respect to surrounding brain tissue. At final view, after the tumor had been removed, the surgeon could assess the site of resection to see whether there was NIR fluorescence in the area of the tumor margins. Such a finding can have a direct effect on the prediction of progression-free survival.
The intensity of fluorescence varied depending on how deep the metastatic lesion was situated, with a lower intensity demonstrated in tumors located more than 10 mm deep. The intensity of fluorescence also differed according to the type of metastasis. Metastases from the lung, breast, and colon showed comparable fluorescence strength, whereas metastases from melanoma displayed a dimmer fluorescence. The authors hypothesize that this difference may be due to the quality of melanin pigment in the lesion to block light penetration.
Postoperative gadolinium-enhanced MRI is considered the gold standard for detecting residual tumors after surgery. The authors found that at final view, NIR with SWIG was as good as or better than postoperative MRI at visualizing residual lesions. In addition, the authors found that the absence of residual NIR fluorescence in the site of resection proved to be a better predictor for gross-total resection, a reduced recurrence rate, and a better progression-free survival than findings on postoperative MRI.
When asked about the article, Dr. John Y. K. Lee responded,
"ICG is an old drug, but scientists continue to find new uses for this fluorophore. The normal, intact blood-brain barrier prevents extravasation of ICG into the normal brain, and thus the enhanced permeability and retention of ICG inside brain metastasis provides the neurosurgeon with exquisite optical contrast, thus aiding the surgeon in rapid identification of the tumor. In this study, we were impressed that our technique -- second window ICG -- allows the surgeon to bring MRI-like imaging to the operating room, allowing us to predict the postoperative MRI result. Indeed, complete resection of the ICG-fluorescence was correlated with improved progression-free survival, thus allowing the surgeon to be sure that their job was performed appropriately.
INFORMATION:
Article: Teng CW, Cho SS, Singh Y, De Ravin E, Somers K, Buch L, Brem S, Singhal S, Delikatny EJ, Lee JYK: Second window ICG predicts gross-total resection and progression-free survival during brain metastasis surgery. Journal of Neurosurgery, published ahead of print March 2, 2021. DOI: 10.3171/2020.8.JNS201810.
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
For additional information, please contact: Ms. Jo Ann M. Eliason, Communications Manager, Journal of Neurosurgery Publishing Group, One Morton Drive, Suite 200, Charlottesville, VA 22903. Email: jaeliason@thejns.org; Phone: 434-982-1209.
For 77 years, the Journal of Neurosurgery has been recognized by neurosurgeons and other medical specialists the world over for its authoritative clinical articles, cutting-edge laboratory research papers, renowned case reports, expert technical notes, and more. Each article is rigorously peer reviewed. The Journal of Neurosurgery is one of six journals published by the JNS Publishing Group, the scholarly journal division of the American Association of Neurological Surgeons. Other peer-reviewed journals published by the JNS Publishing Group include Journal of Neurosurgery: Spine, Journal of Neurosurgery: Pediatrics, Journal of Neurosurgery: Case Lessons, Neurosurgical Focus, and Neurosurgical Focus: Video. All six journals can be accessed at http://www.thejns.org.
Founded in 1931 as the Harvey Cushing Society, the American Association of Neurological Surgeons (AANS) is a scientific and educational association with more than 10,000 members worldwide. The AANS is dedicated to advancing the specialty of neurological surgery in order to provide the highest quality of neurosurgical care to the public. All active members of the AANS are certified by the American Board of Neurological Surgery, the Royal College of Physicians and Surgeons (Neurosurgery) of Canada, or the Mexican Council of Neurological Surgery, AC. Neurological surgery is the medical specialty concerned with the prevention, diagnosis, treatment, and rehabilitation of disorders that affect the entire nervous system including the brain, spinal column, spinal cord, and peripheral nerves. For more information, visit http://www.AANS.org.