Hospitals and LTCF are hotspots for pathogen transmission. The frequency and nature of contacts between patients and staff have been shown to play an important role in the transmission of pathogens such as methicillin-resistant Staphylococcus aureus (MRSA). In this study, the authors combined mathematical modelling and detailed data on close-proximity interactions (CPI) in healthcare settings to investigate to which extent knowledge of the contact network can help implement effective interventions reducing the incidence of MRSA colonisation.
The model was constructed using data collected over 3 months in a French LTCF at Berck-sur-Mer on the northern coast of France - a long-term rehabilitation hospital (average patient stay 3 months) composed of 151 patients and 236 staff, who were all followed up for Methicillin-resistant Staphylococcus aureus (MRSA) colonisation and tracked for CPIs using sensors* (over 2.5 million CPIs recorded). On average, 5% of patients and staff were newly colonised with MRSA each week across the 3-month study.
Being colonised with MRSA means a person carries the bacteria in heir nose or skin, but they are not sick with a MRSA infection. But colonisation is important because individuals are most likely to be infected (and made ill) by the S aureus they are colonised with. So, individuals colonised by MRSA are more likely to then be infected by that MRSA, which is then hard to treat with antibiotics. Dr Leclerc explains: “By preventing colonisation we reduce the risk of infection. Basically, it is best to prevent the fire from even starting in the first place, instead of having to stop it later!”
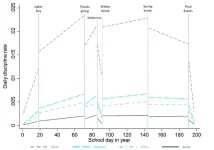
Using an extensive simulation study, the authors examined the potential impact on MRSA colonisation incidence of three interventions. Firstly, staff reallocation, defined as the random attribution of a reduced number of patients to each staff member whilst maintaining global care needs, thereby reducing the number of unique contacts per staff. Secondly, reinforced contact precautions, which could include improved hand hygiene compliance or glove wearing, thereby reducing patient-to-staff and staff-to-patient transmission. Thirdly, vaccination partially protecting those vaccinated against transmission from any other individual. The authors say: “We considered that interventions cannot be feasibly applied to the whole population, and thus we need to investigate who should be targeted as a priority.”
Simulation results showed that the intervention effect can be optimised by targeting “supercontactor” individuals. This includes both frequency-based supercontactors (with highest number of unique contacts), or duration-based supercontactors (with longest cumulative time spent in contact). In this study, supercontactors were mostly composed of nurses, and also patients with neurological disorders, typically those with conditions such as Alzheimer’s disease and Parkinson’s disease in neurological support wards, who, while less mobile than other patients, require more care (and thus more nurse / staff contacts).
The authors found that, while full staff reallocation can reduce colonisation incidence by up to 40%, reallocating only the 180 nurses (who are part of the 236 staff) is sufficient to obtain a 30% reduction. Interestingly, reinforced contact precautions targeting only the 180 nurses was shown by the model to be more effective than even reallocation of all staff - reducing colonisation incidence by up to 45%.
For an equal number of individuals targeted, reinforced contact precautions and vaccination can be further optimised by targeting supercontactors instead of randomly selecting nurses. In an example targeting a fixed number of 60 individuals, the authors find that the highest reduction was achieved by targeting either duration-based patient supercontactors, or frequency-based staff supercontactors. Overall, the most efficient strategy in this example was to vaccinate duration-based patient supercontactors (the patients with neurological conditions described above), which the modelling showed would reduce colonisation incidence by 23%.
The authors conclude: “Our analysis demonstrates the value of combining data collection in healthcare settings and modelling to inform intervention implementation. Identifying and targeting supercontactors was found to be key to implement optimised interventions against the transmission of infectious diseases in long-term care facilities. Because both staff and patients can be supercontactors, including patients in prevention interventions may be key in some healthcare institutions.”
Dr Leclerc adds: "While this study focused on MRSA, staff-patient contact networks in hospitals and other long-term care facilities also play a key role in the transmission of other diseases such as COVID-19 and influenza. Therefore, identifying supercontactors in different healthcare settings would substantially improve interventions to stop the spread of infectious diseases. To clarify this, we plan to repeat this work with other pathogens, in different healthcare institutions."
Dr Quentin Leclerc, Epidemiology and Modelling of Antibacterial Escape, Institut Pasteur, Paris, France & Laboratoire Modélisation, Épidémiologie et Surveillance des Risques Sanitaires, Conservatoire National des Arts et Métiers, Paris, France. T) +33 6 02 48 37 02 E) quentin.leclerc@pasteur.fr
Alternative contact Tony Kirby in the ECCMID Media Centre. T) +44 7834 385827 E) tony.kirby@tonykirby.com
This press release is based on abstract 1615 at the European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) annual meeting. The material has been peer reviewed by the congress selection committee. The research represents ongoing work and has been not yet been submitted to a medical journal for publication.
The authors declare no conflicts of interest.
For full abstract click here
For full poster click here
A study describing the data collection in this research has been published in the journal Scientific Reports: https://www.nature.com/articles/s41598-018-20008-w
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking
(grant agreement 101034420). This JU receives support from EU's Horizon 2020 research and
innovation program and EFPIA.
END