A pioneering drug for a rare kidney disease prevents organ failure and significantly improves the outcome for patients, new research has confirmed.
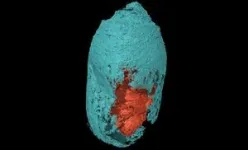
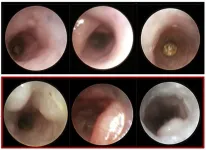
Atypical Haemolytic Uraemic Syndrome (aHUS) is a genetic life-threatening condition caused by a defect in the immune system which leads to kidney failure.
Newcastle University, UK, carried out clinical trials into the drug, eculizumab, which eventually led to the NHS approving the treatment for use in patients from 2015.
Now, a study by Newcastle experts, published in Blood, revealed that eculizumab prevents 86% of patients going into kidney failure which highlights the importance of the use of the medication.
Life-changing treatment
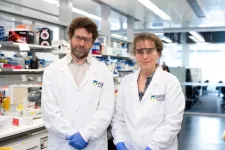
Professor David Kavanagh, from Newcastle University, who led the study, said: “Our study confirms the effectiveness of eculizumab in preventing kidney failure for those with aHUS.
“It further strengthens the importance of patients receiving early treatment as it’s lifesaving and helps significantly improve quality of life without the need for dialysis or a kidney transplant.
“Two decades ago, we began researching aHUS and it’s wonderful to see that our efforts have benefitted those with the illness with the NHS approving the drug all those years ago.”
In the largest study of its kind, which was funded by Kidney Research UK and the Medical Research Council, more than 2,000 aHUS patients between 1995 and 2019 were analysed.
A total of 244 were given eculizumab and responded very well to the treatment. However, a small proportion did not with 14% of patients still requiring long-term dialysis.
For some of those who did not benefit, a new genetic cause for aHUS was identified which allowed the drug to be stopped to avoid the potential side effects of ineffective treatment.
Dr. Vicky Brocklebank, from Newcastle University, said: “This study is a wonderful example of the benefits of close collaboration between patients, clinicians, researchers, and charities.
“Our pioneering research has allowed for genetically targeted treatments to improve patient outcomes and revolutionise the way the condition is managed.”
It is estimated that 20-30 new patients are diagnosed with the condition each year.
NHS approval
Eculizumab costs £328,000 per year per adult patient and is given intravenously every two weeks. It was recommended for use on the NHS by the National Institute for Health and Clinical Excellence (NICE) eight years ago.
When the drug was approved, NHS England commissioned the National Renal Complement Therapeutics Centre, a collaboration between Newcastle University and Newcastle upon Tyne Hospitals NHS Foundation Trust, to run the highly specialised aHUS service.
Professor James Palmer, National Medical Director for Specialised Services at NHS England, said: “These important findings provide renewed evidence that eculizumab is helping people to live longer without kidney failure, and could help enable doctors to identify those who are unlikely to benefit from the drug and could be spared the side effects.
“Collaborative research projects like this are helping to drive real progress for NHS patients with the support of a nationally commissioned service that provides both comprehensive clinical advice and a national patient registry, and it’s fantastic to see the results, which will help save and improve patients’ lives.”
Further research by the Newcastle team will now focus on finding a cure for the small proportion of patients who do not respond to eculizumab.
Dr. Aisling McMahon, executive director of research and policy at Kidney Research UK, said: “This work by David, Vicky and the Newcastle team is a really important example of how, with collaboration between several partners, laboratory research can lead to clinical benefits for patients.
“We are delighted to have been a significant partner in this research and look forward to future projects supporting patients with aHUS.”
Newcastle University and Newcastle Hospitals are both part of Newcastle Health Innovation Partners (NHIP). NHIP is one of eight prestigious Academic Health Science Centres (AHSCs) across the UK, bringing together partners to deliver excellence in research, health education and patient care.
Reference: Atypical haemolytic uraemic syndrome in the era of terminal complement inhibition - An observational cohort study. Vicky Brocklebank et al. Blood. DOI: 10.1182/blood.2022018833
Patient Case study
Chloe Pratt thought her chances of ever living a normal life, let alone starting a family, had been dashed when she was diagnosed with aHUS last year.
The HR assistant’s diagnosis came out of the blue as she was the first in her family to have presented with the disease after becoming seriously ill and being admitted to intensive care.
Within days of being diagnosed, she was given eculizumab and is doing so well on the treatment that she has regained hope for a future she once feared might be out of reach.
Had Chloe not been given the treatment she would have been on permanent dialysis, and this makes it less likely to become pregnant as well as more likely to have complications.
Chloe, 25, of Darlington, said: “I’d never heard of aHUS, so it was quite overwhelming to be told that I had a life-threating illness and would need eculizumab.
“I was extremely tired, and I was just not feeling myself, but it wasn’t until my eyes went yellow that I went to seek medical advice, leading to my shock diagnosis.
“Since I have been taking eculizumab I feel much better, and I am getting back to myself again. I can’t imagine not being on this treatment, it has prevented kidney failure and it has saved my life.”
Reflecting on her future, Chloe added: “I’m now really excited about the prospect of living a normal life and even hope one day to be able to start a family.
“After my diagnosis, I feared that this dream would not be possible, but thanks to eculizumab, I see a brighter path ahead.”
At least nine different genes have been identified to be associated with aHUS. Several members of Chloe’s family were genetically tested for the condition and do have the affected genes, putting them at risk of developing the disease in the future.
Chloe said: “It’s fantastic that the research into aHUS and eculizumab has been led in Newcastle and I feel very lucky that I have been able to benefit from this.”
Ends
END