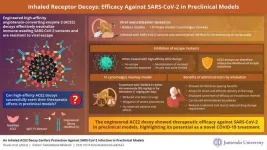
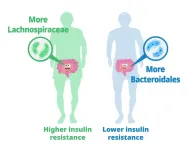
The surface protein of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), known as the spike protein, is critical for infecting host cells. The spike protein facilitates the infection process by binding to angiotensin-converting enzyme 2 (ACE2) receptors on the surface of airway epithelial cells, initiating the virus entry into the cells. By engineering an ACE2 receptor to increase the affinity to the spike protein, researchers demonstrated a novel method to neutralize the virus effectively. The engineered ACE2 (3N39v4-Fc) acts as a decoy by binding to the viral spike protein, thus preventing the binding of viruses to the ACE2 receptor on the cell surface. This inhibition by the ACE2 decoy is detrimental to SARS-CoV-2.
The study was carried out by a team of researchers led by Professor Toru Okamoto from the Department of Microbiology at Juntendo University. While the team, including Prof. Okamoto, Dr. Atsushi Hoshino from the Department of Cardiovascular Medicine at Kyoto Prefectural University of Medicine, and Prof. Junichi Takagi from the Laboratory of Protein Synthesis and Expression at Osaka University demonstrated that 3N39v4-Fc had a 100-times higher binding affinity to the spike protein compared to unmodified (wild-type) ACE2. This highlighted the potency of 3N39v4-Fc to prevent the emergence of resistant virus and the efficacy in rodent models in 2021 and 2022.
In the latest study published in the journal Science Translational Medicine, the team demonstrated the potency of the engineered ACE2 receptor decoy (3N39v4-Fc) against the Omicron variants, including BA.2.12.1, BA.2.75, and the currently spreading XBB and BQ.1. While several groups are working on the development of an ACE2 decoy, the team, for the very first time, reported a therapeutic effect of the 3N39v4-Fc in a preclinical model using cynomolgus monkeys. The team investigated several effects in the model, including the antiviral effect, changes in CT images in the chest, inflammation, pharmacokinetics of the 3N39v4-Fc, and safety. These findings of the study contribute to further evaluation in human trials.
First, the team tested the effectiveness of the 3N39v4-Fc in preventing the emergence of escape mutants, 3N39v4-Fc-resistant viruses that evade the ACE2 receptor decoys. Although the team's earlier study demonstrated the ability of an engineered ACE2 decoy to prevent the emergence of escape mutants, in the latest study, the team validated and confirmed their results using advanced techniques. Their experiments revealed that the 3N39v4-Fc reduced the possibility of the escape mutants more efficiently than wild-type ACE2, demonstrating a minimum risk of the emergence of escape mutants by high-affinization!
Further, the team tested the feasibility of the 3N39v4-Fc administration via the inhalation route, as compared with the administration via the intravenous injection route used in the team's earlier study. Through advanced imaging techniques based on positron emission tomography (PET) imaging and zirconium (Zr)-labeling, the team found that the distribution and clearance patterns within the body differed between inhalation and intravenous administration route in rodents. Intravenous administration resulted in a predominant accumulation of 3N39v4-Fc in the liver, whereas inhalation led to uptake predominantly in the lungs. Remarkably, inhalation administration demonstrated a significant dose-sparing benefit of up to 20-fold compared to conventional intravenous administration. “This comparison holds immense significance, as it achieves equivalent therapeutic results with just a twentieth of the intravenous dose, potentially leading to substantial cost reduction in treatment against respiratory infections,” explains Prof. Okamoto.
Again, to verify the potential efficacy of these results for humans, the researchers conducted experiments on cynomolgus monkeys infected with the Delta variant of SARS-CoV-2. The effect of 3N39v4-Fc was tested by both intravenous and inhalation routes. The treatment led to a reduction in lung abnormalities and a substantial reduction in infectious virus levels, showing its potential as a therapeutic option.
“Our successful treatment of SARS-CoV-2-infected cynomolgus monkeys emphasizes the efficacy and safety of this novel drug. The exceptional efficacy via inhalation administration of the decoys presents a groundbreaking approach to reduce the strain on healthcare systems as it enables patients to self-administer the drug,” says Prof. Okamoto.
In conclusion, the engineered ACE2 decoy exhibits potent neutralizing activity against SARS-CoV-2 variants, and the remarkable efficacy in monkeys highlights its potential for application in the treatment of humans.
Reference
Authors
Emiko Urano1, Yumi Itoh2,3, Tatsuya Suzuki2,3, Takanori Sasaki4, Jun-ichi Kishikawa5, Kanako Akamatsu6, Yusuke Higuchi7, Yusuke Sakai8, Tomotaka Okamura1, Shuya Mitoma9, Fuminori Sugihara10, Akira Takada2, Mari Kimura2, Shuto Nakao2, Mika Hirose5, Tadahiro Sasaki11, Ritsuko Koketsu11, Shunya Tsuji12, Shota Yanagida13, Tatsuo Shioda11,14, Eiji Hara12,14, Satoaki Matoba7, Yoshiharu Matsuura14, Yasunari Kanda13, Hisashi Arase14,15,16, Masato Okada6,14,15,17, Junichi Takagi14,18, Takayuki Kato5,14,16, Atsushi Hoshino7, Yasuhiro Yasutomi1,19, Akatsuki Saito9,20,21, Toru Okamoto2,3,14
Title of the original paper
An inhaled ACE2 decoy confers protection against SARS-CoV-2 infection in preclinical models
Journal
Science Translational Medicine
DOI
Affiliations
10.1126/scitranslmed.adi2623
1Laboratory of Immunoregulation and Vaccine Research, Tsukuba Primate Research Center, National Institutes of Biomedical Innovation, Health and Nutrition, Tsukuba, Japan.
2Institute for Advanced Co-Creation Studies, Research Institute for Microbial Diseases, Osaka University, Osaka, Japan.
3Department of Microbiology, Juntendo University School of Medicine, Japan
4Collaborative Research Center for Okayama Medical Innovation Center, Dentistry, and Pharmaceutical Sciences, Dentistry and Pharmaceutical Sciences, Okayama University Graduate School of Medicine, Okayama, Japan.
5Laboratory of CryoEM Structural Biology, Institute for Protein Research, Osaka University, Osaka, Japan.
6Department of Oncogene, Research Institute for Microbial Diseases, Osaka University, Osaka, Japan.
7Department of Cardiovascular Medicine, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, Kyoto, Japan.
8Department of Pathology, National Institute of Infectious Diseases, Tokyo, Japan.
9Department of Veterinary Science, Faculty of Agriculture, University of Miyazaki, Japan.
10Central Instrumentation Laboratory, Research Institute for Microbial Diseases, Osaka University, Japan.
11Department of Viral Infection, Research Institute for Microbial Diseases, Osaka University, Japan.
12Department of Molecular Microbiology, Research Institute for Microbial Diseases, Osaka University, Japan.
13Division of Pharmacology, National Institute of Health Sciences, Kanagawa, Japan.
14Center for Infectious Disease Education and Research, Osaka University, Japan.
15Department of Immunochemistry, Research Institute for Microbial Diseases, Osaka University, Japan.
16Center for Advanced Modalities and Drug Delivery System, Osaka University, Japan.
17Laboratory of Oncogene research, World Premier International Immunology Frontier Research Centre, Osaka University, Japan.
18Laboratory of Protein Synthesis and Expression, Institute for Protein Research, Osaka University, Japan.
19Department of Molecular and Experimental Medicine, Mie University Graduate School of Medicine, Japan.
20Center for Animal Disease Control, University of Miyazaki, Japan.
21Graduate School of Medicine and Veterinary Medicine, University of Miyazaki, Japan
Youtube Link
https://youtu.be/sgxH57cHIfI
END