Recent developments include a novel computational tool to detect single base pair DNA changes in single-cell sequencing data, a potential target to treat hypertension caused by drugs commonly used in organ transplants, further insights into the steps involved in genetic recombination, a novel treatment target for a subset of adenoid cystic carcinoma (ACC), a combination therapy that improves outcomes in certain patients with acute myeloid leukemia (AML), and a target for treating prolonged cytopenia in patients with relapsed/refractory large B cell lymphoma treated with chimeric antigen receptor (CAR) T cell therapy.
Read this press release in the MD Anderson Newsroom.
Novel computational tool enhances single-cell sequencing to uncover genetic variants
Single-nucleotide variants (SNVs) are changes at specific positions in a DNA sequence that can help classify and explain differences in disease susceptibility across populations. While single-cell sequencing provides valuable insights into cellular differences within diverse tissue samples, current tools are only able to detect a small amount of SNVs, limiting information on genetic ancestry. To help bridge this gap, researchers led by Ken Chen, Ph.D., developed a more sensitive computational tool, called Monopogen, that accurately detects SNVs from single-cell sequencing data. As a proof of concept, the researchers applied the tool to uncover genetic determinants of cardiac health, accurately determining ancestry and classifying differences among human populations. This tool can potentially be used to learn more about the genetic drivers of cellular processes and to identify risks of complex diseases in different populations, informing better prevention and treatment strategies. Learn more in Nature Biotechnology.
Researchers find potential target to treat hypertension caused by organ transplant drug
Calcineurin inhibitors (CNIs) are effective immunosuppressants used to minimize rejection of transplanted organs and tissues, but they can also cause persistent hypertension and other side effects. Calcineurin is abundantly present in the hypothalamus, which regulates blood pressure, and its inhibition leads to hyperactivity of excitatory NMDA receptors in the brain. However, long-term blockade of NMDA receptors also comes with negative side effects. To identify a better therapeutic strategy and provide insights into the impact of CNIs on NMDA receptor activity in the hypothalamus, researchers led by Hui-Lin Pan, M.D., Ph.D., examined the role of α2δ-1, a calcium channel subunit. The study showed that CNIs increase NMDA receptor trafficking and activity via interaction with α2δ-1 in the hypothalamus, reinforcing that this is the main driver of CNI-induced hypertension. The findings suggest that α2δ-1 is a viable therapeutic target meriting further research for treating CNI-induced hypertension. Learn more in Circulation Research.
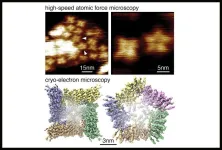
Study identifies novel intermediates involved in genetic crossovers in mammals
Genetic crossovers – the exchange of DNA between pairs of chromosomes from each parent – play a crucial role in accurate chromosome segregation during meiotic cell division. However, the mechanisms underlying the formation of these crossovers in mammals are poorly understood. To provide further insight into this process, researchers led by Francesca Cole, Ph.D., used genetic dissection to map the frequency and distribution of crossover points in mouse models. The researchers discovered two unique intermediate steps that occur prior to recombination. Additionally, they highlighted the DNA mismatch repair protein MLH3 as a pivotal structural component required to form the junctions involved in recombination. These findings help refine the current understanding of recombination in mammals, advancing knowledge of how genes are transferred during meiosis. Learn more in Molecular Cell.
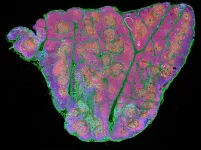
Spatial immunoprofiling uncovers new target for aggressive adenoid cystic carcinoma
There are currently no effective systemic therapies for metastatic adenoid cystic carcinoma (ACC), a rare cancer that forms in the salivary glands. A new study led by Renata Ferrarotto, M.D., and Luana Sousa, M.D., builds on previous findings in two major disease subtypes, including ACC-I, which is associated with poor patient prognosis. By exploring the tumor microenvironment, the researchers discovered that ACC-I tumors overexpressed the immune checkpoint protein B7-H4, resulting in an immune-excluded tumor microenvironment. In ACC-I lab models, treatment with an antibody-drug conjugate targeting B7-H4 led to a 90% complete response rate, highlighting B7-H4 as a potential therapeutic target. These results suggest further investigation of B7-H4 targeting agents is merited and underscore the need to develop biomarkers for individualized treatment in this diverse patient population. Learn more in Clinical Cancer Research.
Combination therapy is safe and improves responses in newly diagnosed AML
Young, fit patients with newly diagnosed acute myeloid leukemia (AML) usually receive cytarabine and anthracycline chemotherapy, with higher doses of cytarabine recently reported to improve outcomes. Adding the targeted therapy sorafenib to this combination has benefitted patients with FLT3-ITD-mutant AML. Based on these findings, researchers led by Tapan Kadia, M.D., studied the combination of cladribine, idarubicin and a higher dose of cytarabine (CLIA) in 65 younger patients with newly diagnosed AML and in 15 patients with AML arising from previously treated myelodysplastic syndrome or myeloproliferative disorder (ts-AML). Patients with FLT3-ITD mutated AML also received an added dose of sorafenib. With a median follow up of 76 months, the composite complete remission rate (CRc) among untreated patients was 83%, while the ts-AML cohort achieved a CRc of 27%. The CRc in patients with FLT3-ITD-mutant AML receiving CLIA plus sorafenib had a CR of 95% (81% of whom had no detectable minimal residual disease), with high rates of durable remission and had a five-year overall survival rate of 59%, meriting further study of this combination. Learn more in American Journal of Hematology.
Study identifies potential target for CAR T-associated prolonged cytopenia in patients with relapsed/refractory large B cell lymphoma
Autologous anti-CD19 chimeric antigen receptor (CAR) T cell therapy has proven highly effective for patients with relapsed/refractory large B-cell lymphoma. However, patients can experience a variety of side effects, such as cytokine release syndrome, neurotoxicity, and prolonged cytopenia (low blood cell counts). In a new study, researchers led by Paolo Strati, M.D., identified a potential target to treat cytopenia in these patients. Using single-cell RNA sequencing on bone marrow samples, the researchers discovered patients with prolonged cytopenia had significantly increased frequencies of clonally expanded cytotoxic T cells expressing genes connected with interferon (IFN) and cytokine signaling. IFN-gamma is known to decrease the ability of hematopoietic stem cells to produce blood cells, so this study suggests that agents targeting the IFN-gamma pathway merit further investigation for treating cytopenia in these patients. Learn more in Cell Reports Medicine.
In case you missed it
Read below to catch up on recent MD Anderson press releases.
Combining immunotherapy with KRAS inhibitor eliminates advanced KRAS-mutant pancreatic cancer in preclinical models MD Anderson receives nearly $4.9 million in CPRIT funding for cancer prevention programs and recruitment
– 30 –
END