“PTSD is a complex pathological condition. We had to extract information across multiple brain regions and molecular processes to capture the biological networks at play,” said first author Nikolaos P. Daskalakis, MD, PhD, director of the Neurogenomics and Translational Bioinformatics Laboratory at McLean Hospital, and an associate professor of psychiatry at Harvard Medical School.
Stress-related disorders develop over time, stemming from epigenetic modifications caused by the interplay between genetic susceptibility and traumatic stress exposure. Previous studies have uncovered hormonal, immune, methylomic (epigenetics) and transcriptomic (RNA) factors mostly in peripheral samples contributing to these diseases, but limited access to postmortem brain tissues from diseased PTSD patients has restricted characterization of brain-based molecular changes at the appropriate scale.
“Our primary goals for this study were to interpret and integrate differential gene and protein expression, epigenetic alterations and pathway activity across our postmortem brain cohorts in PTSD, depression and neurotypical controls,” said senior author Kerry Ressler, MD, PhD, chief scientific officer and director of Division of Depression and Anxiety Disorders and Neurobiology of Fear Laboratory at McLean Hospital, and a professor of psychiatry at Harvard Medical School. “We essentially combined circuit biology with powerful multi-omics tools to delve into the molecular pathology behind these disorders.”
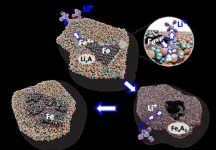
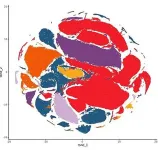
For this, the team analyzed multi-omic data from 231 PTSD, MDD and neurotypical control subjects, along with 114 individuals from replication cohorts for differences in three brain regions — the medial prefrontal cortex (mPFC), hippocampal dentate gyrus (DG) and central nucleus of the amygdala (CeA). They also performed single-nucleus RNA sequencing (snRNA-seq) of 118 PFC samples to study cell-type-specific patterns and evaluated blood-based proteins in more than 50,000 UK Biobank participants to isolate key biomarkers associated with stress-related disorders. Finally, the overlap of these key brain-based disease process genes was compared with genome-wide association studies (GWAS)-based risk genes to identify PTSD and MDD risk.
PTSD and MDD individuals both shared altered gene expression and exons in the mPFC, but differed in the localization of epigenetic changes. Further analysis revealed that history of childhood trauma and suicide were strong drivers of molecular variations in both disorders. The authors noted that MDD disease signals were more strongly associated with male-specific results, suggesting that sex differences may underlie disease risk.
Top disease-associated genes and pathways across regions, omics, and/or traits implicated biological processes in both neuronal and non-neuronal cells. These included molecular regulators and transcription factors, and pathways involved in immune function, metabolism, mitochondria function and stress hormone signaling.
“Understanding why some people develop PTSD and depression and others don’t is a major challenge,” said investigator Charles B. Nemeroff, M.D., PhD, chair of the Department of Psychiatry and Behavioral Sciences at Dell Medical School of UT Austin. “We found that the brains of people with these disorders have molecular differences, especially in the prefrontal cortex. These changes seem to affect things like our immune system, how our nerves work, and even how our stress hormones behave.”.
The genetic components of the work built on a study published last month by researchers including Ressler and Daskalakis in Nature Genetics, in which they identified 95 locations, or loci in the genome (including 80 new) associated with PTSD. Their multi-omic analyses found 43 potential causal genes for the disorder.
The researchers now could reveal only limited overlap between the top genes and those implicated in GWAS studies, underscoring the gap in current understanding between disease risk and underlying disease processes. In contrast, they discovered greater correlations between brain multi-omics and blood markers.
“Our findings support the development of brain-informed blood biomarkers for real-time profiling,” said Daskalakis.
Ressler added, “These biomarkers could help overcome current challenges in obtaining brain biopsies for advancing new treatments.”
Limitations of the study include the inherent biases in postmortem brain research, including population selection, clinical assessment, comorbidities, and end-of-life state. The authors also caution that they did not fully characterize all cell-subtypes and cell states, and that future studies are required to understand contrasting molecular signals across omics or brain regions.
The team plans on using this database as groundwork for future analysis of how genetic factors interact with environmental variables to create downstream disease effects.
“Learning more about the molecular basis of these conditions, PTSD and MDD, in the brain paves the way for discoveries that will lead to more effective therapeutic and diagnostic tools. This work was possible because of the brain donations to the Lieber Institute Brain Repository from families whose loved ones died of these conditions,” said Joel Kleinman, MD, PhD, associate director of Clinical Sciences at the Lieber Institute for Brain Development. “We hope our research will one day bring relief to individuals who struggle with these disorders and their loved ones.”
Authorship: Additional Mass General Brigham authors of the study from McLean Hospital include Artemis Iatrou, Chris Chatzinakos, Aarti Jajoo, Clara Snijders, Christopher P. DiPietro, Ioulia Tsatsani, Cameron D. Pernia, Marina Soliva-Estruch, Vincent L Holstein, Justina F. Lugenbühl, Mohammad S. E Sendi and Sabina Berretta.
Co-authors include Dennis Wylie, Chia-Yen Chen, Dhivya Arasappan, Rahul A. Bharadwaj, Leonardo Collado-Torres, Stefan Wuchty, Victor E. Alvarez, Eric B Dammer, Amy Deep-Soboslay, Duc M. Duong, Nick Eagles, Bertrand R. Huber, Louise Huuki, Μark W. Logue, Adam X. Maihofer, Mark W. Miller, Caroline M Nievergelt, Geo Pertea, Deanna Ross, Benjamin B. Sun, Ran Tao, James Tooke, Erika J. Wolf, Zane Zeier, PTSD Working Group of Psychiatric Genomics Consortium, Frances A. Champagne, Thomas Hyde, Nicholas T. Seyfried, Joo Heon Shin, Daniel R. Weinberger, Charles B. Nemeroff and Joel E. Kleinman.
Disclosures: Nikolaos P. Daskalakis is on the scientific advisory boards for BioVie Inc., Circular Genomics, Inc. and Feel Therapeutics, Inc.; Daniel R. Weinberger is on the advisory boards of Pasithea Therapeutics and Sage Therapeutics for unrelated work; Duc M. Duong is a cofounder of ARC Proteomics, and cofounder and paid consultant of Emtherapro Inc.; Chia-Yen Chen is an employee of Biogen Inc.; Mohammad S. E Sendi receives consulting fees for unrelated work from Niji Corp, Benjamin B. Sun is an employee and stockholder of Biogen Inc.; Kerry J. Ressler has received consulting income from Alkermes and sponsored research support from Brainsway and Takeda, and is on the scientific advisory boards for Janssen, Verily, and Resilience Therapeutics for unrelated work.
Funding: This work was supported by grants from NIMH, the Brain & Behavior Research Foundation, Stichting Universitas / the Bontius Foundation, Dutch Research Council (NWO) fund and McLean Hospital.
Paper cited: Daskalakis, Nikolaos P. et al. “Systems biology dissection of PTSD and MDD across brain regions, cell types, and blood” Science, DOI: 10.1126/science.adh3707
###
About McLean
McLean Hospital has a continuous commitment to put people first in patient care, innovation and discovery, and shared knowledge related to mental health. It is consistently named the #1 freestanding psychiatric hospital in the United States by U.S. News & World Report, and is #1 in America for psychiatric care in 2023-24. McLean Hospital is the largest psychiatric affiliate of Harvard Medical School and a member of Mass General Brigham. To stay up to date on McLean, follow us on Facebook, YouTube, and LinkedIn.
[JR1]URL at time of publication: http://www.science.org/doi/10.1126/science.adh3707
END