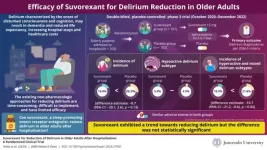
Delirium is a sudden onset and temporary state of disturbed consciousness or cognition, occurring due to underlying medical issues like fever or alcohol withdrawal. It is most common among older hospitalized adults aged 75 years or above, leading to increased risk of falls, dementia, low life expectancy, and high healthcare expenses.
Non-pharmacological approaches to prevent or reduce delirium are time-consuming, hard to implement, and partially effective. So, pharmacological interventions offer hope. Insomnia, a significant risk factor for delirium, could be alleviated with sleep-promoting medications. However, not all medications are suitable. Some may aggravate delirium. Interestingly, suvorexant (an orexin receptor antagonist) promotes sleep by blocking a neuropeptide called orexin that regulates wakefulness. This mechanism could prevent delirium, as shown by many studies.
Against this backdrop, a team of researchers involving Professor Kotaro Hatta from the Department of Psychiatry at Juntendo University Nerima Hospital in Tokyo, Japan, tested whether suvorexant can reduce delirium in older adults at high risk for delirium after hospitalization. The research team included Dr. Yasuhiro Kishi from Nippon Medical School Musashikosugi Hospital, Dr. Ken Wada from Hiroshima City Hiroshima Citizens Hospital, Dr. Takashi Takeuchi from Tokyo Medical and Dental University Hospital, Dr. Toshihiro Taira from Fukuyama City Hospital, Dr. Keiichi Uemura from Tonan Hospital, Dr. Asao Ogawa from National Cancer Center Hospital East, Ms. Kanae Takahashi, Ms. Asako Sato, Mr. Masayoshi Shirakawa and Dr. Ichiro Arano from MSD K.K., Tokyo, Japan, and Dr. W. Joseph Herring from Merck & Co., Inc., Rahway, NJ, USA. Their study was published in JAMA Network Open on August 16 2024.
Reflecting on the motivation behind the study, Prof. Hatta says, “While working as a psychiatric liaison at a general hospital, I was busy managing patients with delirium every day. So, when an orexin receptor antagonist became available, we decided to use this drug to target the sleep-wake cycle disturbances, a primary clinical manifestation of delirium.”
To this end, researchers conducted a double-blind, placebo-controlled, phase 3 randomized clinical trial across 50 Japanese hospitals from October 2020 to December 2022. The trial included 203 Japanese adults aged 65 to 90 years who were at high risk for delirium and hospitalized for sudden illness or scheduled surgery. Participants were randomly assigned to two groups, with 101 receiving suvorexant (15 mg) and 102 receiving a placebo each night for five to seven days. They were assessed daily for delirium based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria. Subtypes of delirium—namely hyperactive (marked by agitation, hallucination, and impulsivity), hypoactive (marked by drowsiness and apathy), and mixed (shifts between hyperactive and hypoactive delirium)—
were also recorded for those who exhibited delirium. Researchers then compared both groups to assess whether suvorexant made a difference.
Consistent with expectations, suvorexant showed a trend toward reducing delirium, with only 16.8% of participants exhibiting delirium compared to 26.5% in the placebo group. However, the difference was not statistically significant. Both groups also experienced similar adverse events, such as constipation and vomiting.
The incidence of hypoactive delirium was similar between the suvorexant (5.9%) and placebo groups (4.9%). However, in the post-hoc exploratory analysis, the incidence of hyperactive and mixed delirium was lower in the suvorexant group (10.9%) compared to placebo (21.6%). Delirium with a hyperactive component was considered since it interferes with surgery or treatment, making it burdensome for hospital staff.
As the results suggest, suvorexant may not have preventive effects on hypoactive delirium but could benefit hyperactive and mixed delirium.
Explaining the results, Prof. Hatta emphasizes, “The lack of significant reduction of delirium after taking suvorexant was surprising since previous studies reported positive findings. However, these studies did not distinguish between delirium subtypes except for one study that excluded hypoactive delirium due to its irrelevance in postoperative management and another that defined the primary outcome as delirium of any type. So, we believe that previous studies have focused more on hyperactive or mixed delirium and overlooked hypoactive delirium.”
Prof. Hatta says, “Addressing this issue can increase the life expectancy of older adults and reduce the burden on healthcare providers.”
Let us hope these insights pave the way for discovering more effective pharmacological interventions for preventing delirium.
Reference
Authors
Kotaro Hatta1, Yasuhiro Kishi2, Ken Wada3, Takashi Takeuchi4, Toshihiro Taira5, Keiichi Uemura6, Asao Ogawa7, Kanae Takahashi8, Asako Sato8, Masayoshi Shirakawa8, Ichiro Arano8, and W. Joseph Herring9
Title of original paper
Suvorexant for reduction of delirium in older adults after hospitalization: A randomized clinical trial
Journal
JAMA Network Open
DOI
10.1001/jamanetworkopen.2024.27691
Affiliations
1Department of Psychiatry, Juntendo University Nerima Hospital, Japan
2Department of Psychiatry, Nippon Medical School Musashikosugi Hospital, Japan
3Department of Psychiatry, Hiroshima City Hiroshima Citizens Hospital, Japan
4Department of Psychiatry, Tokyo Medical and Dental University Hospital, Japan
5Department of Psychiatry and Psycho-Oncology, Fukuyama City Hospital, Japan
6Department of Psychiatry and Palliative Care, Tonan Hospital, Japan
7Department of Psycho-Oncology, National Cancer Center Hospital East, Japan
8MSD K.K. (Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA), Tokyo, Japan
9Merck & Co., Inc., Rahway, NJ, USA
About Professor Kotaro Hatta
Dr. Kotaro Hatta is a Professor at the Department of Psychiatry, Juntendo University Nerima Hospital, Tokyo, Japan. He graduated from Kanazawa University School of Medicine, and obtained a doctorate in medical science at Kanazawa University. He has previously served at Tokyo Metropolitan Matsuzawa Hospital, Rudolf Magnus Institute, Utrecht University, the Netherlands, and Tokyo Metropolitan Bokuto Hospital. He is an active member of the medical community, having previously served as Director of the Japanese Society of General Hospital Psychiatry, and now serves as Vice-Chairman of the Japanese Association for Emergency Psychiatry. He specializes in emergency psychiatry, consultation-liaison psychiatry, and psychopharmacology, and he has published numerous papers, in renowned journals like The Lancet, JAMA, and JAMA Psychiatry.
END