(Press-News.org) Guideline highlights:
The American Heart Association and the American College of Cardiology joint guideline addressing cardiovascular evaluation and management of patients before, during and after noncardiac surgery reviews a decade of new evidence and provides updates since the last guideline in 2014.
The updates in the guideline are intended for patients scheduled for noncardiac surgery from preoperative evaluation through postoperative care and include appropriate use of cardiovascular testing and screening, management of cardiovascular conditions and risks, and recommendations for those taking sodium-glucose cotransporter-2 inhibitors (SGLT2-inhibitors) for Type 2 diabetes.
The guideline was developed in collaboration with and endorsed by the American College of Surgeons, the American Society of Nuclear Cardiology, the Heart Rhythm Society, the Society of Cardiovascular Anesthesiologists, the Society of Cardiovascular Computed Tomography, the Society of Cardiovascular Magnetic Resonance and the Society of Vascular Medicine.
Embargoed until 1:00 p.m. CT/2:00 p.m. ET Tuesday, Sept. 24, 2024
DALLAS and WASHINGTON, Sept. 24, 2024 — The 2024 guideline for cardiovascular management of adults undergoing noncardiac surgery reflects a decade of updates and new evidence since the guideline’s last release in 2014. It is published today in the American Heart Association’s flagship, peer-reviewed journal Circulation and simultaneously in JACC, the flagship journal of the American College of Cardiology.
The “2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery” presents the latest evidence for the appropriate assessment of cardiovascular disease risk for patients scheduled for noncardiac surgery and management of cardiovascular disease risk factors before, during and after noncardiac surgery. The recommendations address patient evaluations and assessments, use of cardiovascular testing and screening, and evidence-based management of cardiovascular conditions and risks before, during and after surgery in those patients.
“There is a wealth of new evidence about how best to evaluate and manage perioperative cardiovascular risk in patients undergoing noncardiac surgery,” said Chair of the guideline writing group Annemarie Thompson, M.D., M.B.A., FAHA, a professor of anesthesiology, medicine and population health sciences at Duke University Medical Center in Durham, North Carolina.
“Worldwide, there are approximately 300 million noncardiac surgeries each year, which underscores the need to summarize and interpret the evidence to assist clinicians in managing patients who present for surgery,” Thompson said. “This new guideline is a comprehensive review of the latest research to help inform clinicians who manage perioperative patients, with the ultimate goal of restoring health and minimizing cardiovascular complications.”
The guideline targets the many disciplines of health care professionals who care for people undergoing surgery that requires general or regional anesthesia and who have known or potential cardiovascular risk.
“From prior studies, conditions such as high blood pressure, Type 2 diabetes, age older than 55 in men and 65 in women, smoking and obesity are known risk factors that predispose patients to cardiovascular disease. Others have a family history of premature coronary artery disease, which can also put them at increased risk,” Thompson said. “This guideline is written with the understanding that these and other cardiovascular risk factors and conditions can contribute to negative surgical outcomes if they are unrecognized or not optimized before surgery.”
Perioperative Management of Cardiovascular Conditions
As in 2014, the 2024 guideline includes a perioperative algorithm to guide health care professionals in care decisions for patients with cardiovascular conditions having noncardiac surgery. The new guideline reviews blood pressure management before, during and after surgery, and highlights specific recommendations for patients with coronary artery disease, hypertrophic cardiomyopathy, valvular heart disease, pulmonary hypertension, obstructive sleep apnea and previous stroke.
Updated Screening Recommendations
The new guideline recommends that health care professionals be judicious and targeted about ordering screenings, such as stress testing, to determine cardiac risk prior to surgery.
The guideline also includes recommendations on using emergency-focused cardiac ultrasound for patients undergoing noncardiac surgery with unexplained hemodynamic instability (unstable blood pressure) if clinicians with expertise in cardiac ultrasound are readily available. Focused cardiac ultrasound has emerged as a screening option since the last guideline; it can be performed in the operating room during surgery to help determine if heart problems are causing unstable blood pressure.
Considerations for Medication Management
Newer medications for Type 2 diabetes, heart failure and obesity management have important perioperative implications, according to the 2024 guideline. SGLT2-inhibitors should be discontinued three to four days before surgery to minimize the risk of perioperative ketoacidosis, which is unbalanced pH levels in the blood that can negatively impact surgical outcomes.
Emerging data suggest that glucagon-like polypeptide-1 (GLP-1) agonists, medications that are used for managing type 2 diabetes and/or obesity, may cause delayed stomach emptying. In addition, nausea is a common side effect of GLP-1 agonists, and patients taking these medications may be at increased risk of pulmonary aspiration, or inhaling stomach content into their lungs, while under anesthesia. Other organizations have recommended to withhold these medications prior to noncardiac surgery (for one week for patients on weekly doses and for one day for patients taking daily doses) to reduce the risk of pulmonary aspiration during surgery; however, the need for discontinuation and timing are an emerging area of investigation.
For patients who are taking blood thinners, the new guideline recommends that in most cases it is safe to stop blood thinners several days before surgery, proceed to surgery and then start taking blood thinners again after surgery, most commonly after hospital discharge. Clinicians are encouraged to refer to the guideline for exceptions and modifications.
Additional Research Needs Identified
Myocardial injury after noncardiac surgery (MINS), or injury to the heart that occurs either during or shortly after noncardiac surgery, is diagnosed by elevated cardiac troponin levels after surgery. MINS occurs in about one in five noncardiac surgery patients. This newly identified condition is associated with worse short- and long-term outcomes for patients, yet little is known about what causes MINS, how to prevent it and how best to manage it. In patients who develop MINS, outpatient follow-up is recommended to counsel patients on how to reduce their heart disease risk factors.
The new guideline emphasizes the importance of paying attention to an irregular heart rhythm known as atrial fibrillation (AFib), which may occur during or after noncardiac surgery. Patients with newly diagnosed AFib have an increased risk of stroke, and guideline authors recommend closely following these patients after surgery to treat reversible causes of AFib and to consider the need for rhythm control and/or the use of blood thinners to prevent stroke. Ongoing studies are evaluating how to best manage AFib that occurs after surgery.
Thompson said, “The U.S. population is getting older and is living longer with chronic health conditions including chronic heart and vascular diseases. A multidisciplinary, team-based approach, including surgeons, primary care physicians, cardiologists, internal medicine doctors and other medical specialists, is needed to optimize care for patients with cardiovascular conditions and risk factors before, during and after surgery.”
This guideline was prepared by a volunteer writing group on behalf of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines, and developed with and endorsed by the American College of Surgeons, the American Society of Nuclear Cardiology, the Heart Rhythm Society, the Society of Cardiovascular Anesthesiologists, the Society of Cardiovascular Computed Tomography, the Society of Cardiovascular Magnetic Resonance and the Society of Vascular Medicine.
Co-authors are Co-Vice Chairs Kirsten E. Fleischmann, M.D., M.P.H., FACC, and Nathaniel R. Smilowitz, M.D., M.S., FACC; Lisa de las Fuentes, M.D., M.S., FAHA; Debabrata Mukherjee, M.D., M.S., FACC, FAHA, MSCAI; Niti R. Aggarwal, M.D., FACC, FASNC; Faraz S. Ahmad, M.D., M.S., FACC, FAHA; Robert B. Allen, J.D.; S. Elissa Altin, M.D., FACC, FSVMI; Andrew Auerbach, M.D., M.P.H.; Jeffrey S. Berger, M.D., M.S., FAHA, FACC; Benjamin Chow, M.D., Ph.D., FACC, FASNC, MSCCT; Habib A. Dakik, M.D., FACC; Eric L. Eisenstein, D.B.A.; Marie Gerhard-Herman, M.D., FACC, FAHA; Kamrouz Ghadimi, M.D., M.H.Sc., FAHA; Bessie Kachulis, M.D.; Jacinthe Leclerc, R.N., Ph.D., FAHA; Christopher S. Lee, Ph.D., R.N., FAHA Tracy E. Macaulay, Pharm.D., FACC; Gail Mates, B.S.; Geno J. Merli, M.D., FSVM; Purvi Parwani, M.B.B.S., M.P.H., FACC; Jeanne E. Poole, M.D., FACC, FHRS; Michael W. Rich, M.D., FACC; Kurt Ruetzler, M.D., Ph.D., FAHA; Steven C. Stain, M.D., FACS; BobbieJean Sweitzer, M.D.; Amy W. Talbot, M.P.H.; Saraschandra Vallabhajosyula, M.D., M.Sc., FAHA, FACC; John Whittle, M.D.; and Kim Allan Williams Sr., M.D., MACC, FAHA, MASNC. Authors’ disclosures are listed in the manuscript.
The Association receives funding primarily from individuals. Foundations and corporations (including pharmaceutical, device manufacturers and other companies) also make donations and fund specific Association programs and events. The Association has strict policies to prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers and health insurance providers, and the Association’s overall financial information are available here.
Additional Resources:
Available multimedia is on right column of release link http://newsroom.heart.org/news/new-guideline-details-how-to-manage-cvd-risk-before-during-after-noncardiac-surgery?preview=f943e617dd92b78df4cf9db5034188e6
After September 24, 2024, view the manuscript in Circulation and JACC.
AHA health information: What is Cardiovascular Disease?
AHA news release: Analysis found weight-loss surgery may help people with obesity manage high blood pressure (Sept. 2024)
AHA news release: Position of stroke patient’s head before surgery may improve neurological function (Feb. 2024)
AHA news release: New technologies and medications that can prevent, reduce CVD top 2023 scientific research (Dec. 2023)
AHA Scientific Statement: Do you really need that test? New statement highlights need to reduce “low-value” heart care (Feb. 2022)
AHA/ACC Joint Guideline: 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery (Aug. 2014)
Follow AHA/ASA news on X @HeartNews
Follow news from the AHA’s flagship journal Circulation @CircAHA
ACC.org Guideline Hub (after embargo – 2 p.m. ET, September 24, 2024)
JACC.org Guideline Hub (after embargo – 2 p.m. ET, September 24, 2024)
ACC 2024 Perioperative Guideline-at-a-Glance (after embargo – 2 p.m. ET, September 24, 2024)
###
About the American Heart Association
The American Heart Association is a relentless force for a world of longer, healthier lives. We are dedicated to ensuring equitable health in all communities. Through collaboration with numerous organizations, and powered by millions of volunteers, we fund innovative research, advocate for the public’s health and share lifesaving resources. The Dallas-based organization has been a leading source of health information for a century. During 2024 - our Centennial year - we celebrate our rich 100-year history and accomplishments. As we forge ahead into our second century of bold discovery and impact, our vision is to advance health and hope for everyone, everywhere. Connect with us on heart.org, Facebook, X or by calling 1-800-AHA-USA1.
About the American College of Cardiology
The American College of Cardiology (ACC) is the global leader in transforming cardiovascular care and improving heart health for all. As the preeminent source of professional medical education for the entire cardiovascular care team since 1949, ACC credentials cardiovascular professionals in over 140 countries who meet stringent qualifications and leads in the formation of health policy, standards and guidelines. Through its world-renowned family of JACC Journals, NCDR registries, ACC Accreditation Services, global network of Member Sections, CardioSmart patient resources and more, the College is committed to ensuring a world where science, knowledge and innovation optimize patient care and outcomes. Learn more at www.ACC.org or follow @ACCinTouch.
END
New guideline details how to manage CVD risk before, during & after noncardiac surgery
Expanded definition of cardiovascular risk related to noncardiac surgery timing and risk, new ways to avoid unnecessary and costly screening, and recommendations for managing patients taking SGLT2-inhibitors are among the updates in the new 2024 joint gui
2024-09-24
ELSE PRESS RELEASES FROM THIS DATE:
Silvia Cavagnero to receive 2025 Emily M. Gray Award
2024-09-24
ROCKVILLE, MD – The Biophysical Society is pleased to announce that Silvia Cavagnero, PhD, of the University of Wisconsin-Madison, has been named the recipient of the 2025 Emily M. Gray Award. Cavagnero will be honored at the Society’s 69th Annual Meeting, being held in Los Angeles, California from February 15-19, 2025.
Cavagnero is being honored for developing courses, innovating instructional methods, mentoring students at all levels, and promoting diversity in biophysics.
“Silvia is an accomplished biophysicist and a born educator,” ...
European Society of Endocrinology expands journal portfolio with the launch of Environmental Endocrinology and Obesity and Endocrinology
2024-09-24
The European Society of Endocrinology (ESE) is delighted to announce the launch of two new multidisciplinary, open-access journals, Environmental Endocrinology and Obesity and Endocrinology. The Journals will be published by Oxford University Press, with the launch issues scheduled for Q2 2025. Submissions are now being welcomed via the Journals' websites.
Environmental Endocrinology will publish high-quality clinical, translational, and basic research on all aspects of environmental impacts on hormone systems in humans and living systems, incorporating the One Health perspective. The Journal will welcome submissions from a broad range ...
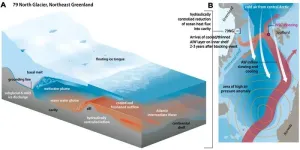
Atmospheric blocking slows ocean-driven melting of Greenland’s largest glacier tongue
2024-09-24
Northeast Greenland is home to the 79° N Glacier – the country’s largest floating glacier tongue, but also one seriously threatened by global warming: warm water from the Atlantic is melting it from below. Experts from the Alfred Wegener Institute have however now determined that the temperature of the water flowing into the glacier cavern declined from 2018 to 2021, even though the ocean has steadily warmed in the region over the past several decades. This could be due to temporarily changed atmospheric circulation patterns. ...
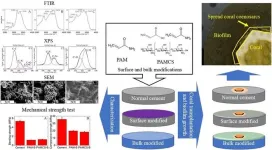
Improved cement to protect the living treasures of our coastlines
2024-09-24
WASHINGTON, Sept. 24, 2024 – Coastlines are vital to our world’s ecology and economy. Coastal ecosystems help maintain biodiversity, provide natural barriers against erosion, storms, and flooding, and act as large carbon sinks to reduce greenhouse gases. Sustainable fisheries and seaside tourist venues support local economies.
Natural coastlines, including coral reefs, marshes, and mangroves, are complete and stable, capable of self-regulation and restoration. That is, unless human interventions, such as urbanization, overdevelopment, pollution, and human-made erosion, make these areas vulnerable to devastation.
Artificial coastlines, ...
Absolute and functional iron deficiency in the US
2024-09-24
About The Study: The findings of this study suggest that absolute and functional iron deficiency affect a large proportion of American adults even in the absence of anemia, heart failure, or chronic kidney disease. Further research on the role of functional iron deficiency in adverse health outcomes and on iron deficiency screening strategies is needed.
Corresponding author: To contact the corresponding author, Leo F. Buckley, Pharm.D., M.P.H., email lfbuckley@bwh.harvard.edu.
To access the embargoed ...
Rural-urban disparities in hospital services and outcomes for children with medical complexity
2024-09-24
About The Study: Rural-residing children with medical complexity were significantly more likely to present to hospitals without dedicated pediatric services in this cohort study. These findings suggest that efforts are justified to ensure that all hospital types are prepared to care for children with medical complexity.
Corresponding author: To contact the corresponding author, JoAnna K. Leyenaar, M.D., Ph.D., M.P.H., email joanna.k.leyenaar@hitchcock.org.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi: 10.1001/jamanetworkopen.2024.35187)
Editor’s Note: Please ...
Fewer than half of US jails provide life-saving medications for opioid use disorder
2024-09-24
A new look into addiction treatment availability in the U.S. criminal justice system reveals that fewer than half (43.8%) of 1,028 jails surveyed across the nation offered any form of medication for opioid use disorder, and only 12.8% made these available to anyone with the disorder. With two-thirds of people who are incarcerated in U.S. jails experiencing a substance use disorder – in many cases, an opioid use disorder – the failure to make these medications widely available in criminal justice settings represents a significant missed opportunity to provide life-saving treatments in an environment where people in need of care can be easily reached.
The study, published ...
Voice-activated cognitive behavioral therapy for insomnia
2024-09-24
About The Study: This randomized clinical trial of an in-home, voice-activated cognitive behavioral therapy for insomnia program among breast cancer survivors found that the intervention improved insomnia symptoms. Future studies may explore how this program can be taken to scale and integrated into ambulatory care.
Corresponding author: To contact the corresponding author, Hannah Arem, Ph.D., email Hannah.Arem@medstar.net.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi: ...
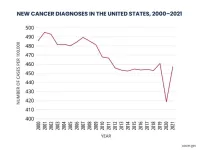
New cancer diagnoses did not rebound as expected following pandemic
2024-09-24
What: Cancer incidence trends in 2021 largely returned to what they were before the COVID-19 pandemic, according to a study by researchers at the National Institutes of Health (NIH). However, there was little evidence of a rebound in incidence that would account for the decline in diagnoses in 2020, when screening and other medical care was disrupted. One exception was breast cancer, where the researchers did see an uptick in diagnoses of advanced-stage disease in 2021. The study appears Sept. 24, 2024, in the Journal of the National Cancer Institute.
A previous study showed that new cancer diagnoses fell abruptly ...
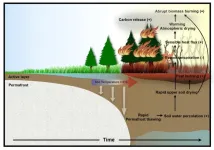
Abrupt intensification of northern wildfires due to future permafrost thawing
2024-09-24
A study, published in the journal Nature Communications by an international team of climate scientists and permafrost experts shows that, according to new climate computer model simulations, global warming will accelerate permafrost thawing and as a result lead to an abrupt intensification of wildfires in the Subarctic and Arctic regions of northern Canada and Siberia.
Recent observational trends suggest that warm and unusually dry conditions have already intensified wildfires in the Arctic region. To understand ...
LAST 30 PRESS RELEASES:
Novel camel antimicrobial peptides show promise against drug-resistant bacteria
Scientists discover why we know when to stop scratching an itch
A hidden reason inner ear cells die – and what it means for preventing hearing loss
Researchers discover how tuberculosis bacteria use a “stealth” mechanism to evade the immune system
New microscopy technique lets scientists see cells in unprecedented detail and color
Sometimes less is more: Scientists rethink how to pack medicine into tiny delivery capsules
Scientists build low-cost microscope to study living cells in zero gravity
The Biophysical Journal names Denis V. Titov the 2025 Paper of the Year-Early Career Investigator awardee
Scientists show how your body senses cold—and why menthol feels cool
Scientists deliver new molecule for getting DNA into cells
Study reveals insights about brain regions linked to OCD, informing potential treatments
Does ocean saltiness influence El Niño?
2026 Young Investigators: ONR celebrates new talent tackling warfighter challenges
Genetics help explain who gets the ‘telltale tingle’ from music, art and literature
Many Americans misunderstand medical aid in dying laws
Researchers publish landmark infectious disease study in ‘Science’
New NSF award supports innovative role-playing game approach to strengthening research security in academia
Kumar named to ACMA Emerging Leaders Program for 2026
AI language models could transform aquatic environmental risk assessment
New isotope tools reveal hidden pathways reshaping the global nitrogen cycle
Study reveals how antibiotic structure controls removal from water using biochar
Why chronic pain lasts longer in women: Immune cells offer clues
Toxic exposure creates epigenetic disease risk over 20 generations
More time spent on social media linked to steroid use intentions among boys and men
New study suggests a “kick it while it’s down” approach to cancer treatment could improve cure rates
Milken Institute, Ann Theodore Foundation launch new grant to support clinical trial for potential sarcoidosis treatment
New strategies boost effectiveness of CAR-NK therapy against cancer
Study: Adolescent cannabis use linked to doubling risk of psychotic and bipolar disorders
Invisible harms: drug-related deaths spike after hurricanes and tropical storms
Adolescent cannabis use and risk of psychotic, bipolar, depressive, and anxiety disorders
[Press-News.org] New guideline details how to manage CVD risk before, during & after noncardiac surgeryExpanded definition of cardiovascular risk related to noncardiac surgery timing and risk, new ways to avoid unnecessary and costly screening, and recommendations for managing patients taking SGLT2-inhibitors are among the updates in the new 2024 joint gui