(Press-News.org) Breast cancer survivors with a family history of the disease, including those who carry BRCA1 and BRCA2 gene mutations, gained more weight over the course of four years than cancer-free women -- especially if they were treated with chemotherapy, according to a prospective study by Johns Hopkins Kimmel Cancer Center researchers.
Data from earlier studies suggest that breast cancer survivors who gain weight may have a higher risk of having their cancer return, the researchers say, noting that gains of 11 pounds or more are also associated with a higher risk of developing cardiovascular disease.
For the study, the researchers reviewed a baseline questionnaire and a follow-up one completed four years later by 303 breast cancer survivors and 307 cancer-free women enrolled in an ongoing and long-term study at the Kimmel Cancer Center of women with a family history of breast or ovarian cancer. Study participants completed a baseline and at least one follow-up questionnaire between 2005 and 2013, and one-quarter of the subjects were premenopausal.
In the four-year span, survivors gained significantly more weight -- 3.6 pounds on average -- than cancer-free women. Among 180 survivors diagnosed with cancer during the last five years of the study period, 37 (21 percent) gained at least 11 pounds over a four-year period compared with 35 of 307 (11 percent) of their cancer-free peers. The weight change findings remained the same after accounting for other factors associated with weight gain, such as increasing age, transition to menopause and level of physical activity, the researchers say.
"Our study suggests that chemotherapy may be one of the factors contributing to weight gain among survivors," says Kala Visvanathan, M.B.B.S., M.H.S., an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health and director of the Clinical Cancer Genetics and Prevention Service at the Kimmel Cancer Center. Women who completed chemotherapy within five years of the study were 2.1 times as likely as cancer-free women to have gained at least 11 pounds during the study.
"There is limited data on weight change in breast cancer survivors, including those at higher risk for the disease compared to the general population," Visvanathan says. "A lot of studies have focused on breast cancer survivors alone, so we don't get a sense of whether women without cancer gain more or less weight, or whether the gain is due to the cancer or the treatment."
Results of the study by Visvanathan and her colleagues appear online in the July 15 issue of Cancer Epidemiology, Biomarkers & Prevention.
Using information from study subjects' answers in detailed questionnaires, along with their medical records, the scientists controlled for such factors as age, menopausal status, physical activity, the presence of cancer-linked mutations in the BRCA genes, and weight at the start of the study when they compared gains in survivors and cancer-free women.
The researchers say they also found a high prevalence of overweight women among the group of 303 breast cancer survivors and 307 cancer-free women with a family history or inherited predisposition for breast cancer, including those who carry BRCA1 or BRCA2 gene mutations, with 46.9 percent of survivors and 55.1 percent of cancer-free women who were overweight or obese.
In addition, breast cancer survivors diagnosed within five years before their baseline weight measurement and who had invasive disease and cancer cells lacking receptors for estrogen gained an average of 7.26 pounds more than cancer-free women.
Statin users among breast cancer survivors treated with chemotherapy also gained more weight -- an average of 10 pounds more -- than cancer-free women who used statins, as well as survivors and cancer-free women who did not use the cholesterol-blocking drug.
"Above and beyond age and menopausal status, there seems to be a weight gain associated with treatment of cancer, particularly in women having chemotherapy and those diagnosed with estrogen receptor-negative, invasive cancers," says Amy Gross, M.H.S., a doctoral candidate in epidemiology at the Bloomberg School of Public Health.
The Johns Hopkins study adds to an emerging body of evidence that chemotherapy can lead to weight gain in cancer survivors, Visvanathan noted, but it's not clear why the treatment has this effect. Some scientists suggest that chemotherapy increases inflammation and insulin resistance, disrupting metabolism and producing weight gain. Patients treated with chemotherapy may also be less physically active and prone to weight gain as a result.
"We're looking at biomarkers in urine and blood in our survivors and in women who are cancer-free to look for the biochemical changes that may be related to this higher weight gain," Visvanathan says.
The researchers plan to continue following the full study group every three to four years to determine how the women's weight changes over a longer period of time.
Noting the limits of the study and the need for longer follow-up, Visvanathan cautions that "we're not yet suggesting any weight gain intervention at the time of chemotherapy."
"But we are suggesting that oncologists, internists or anyone treating breast cancer survivors, including those with a family history of the disease, could help them monitor their weight over the long term," she adds.
The scientists note that the majority of subjects in the current study are Caucasian, which limits their ability to apply their findings to women of other ethnic backgrounds. The study's reliance on self-reported weight also can be subject to bias or error, but the scientists found a high degree of similarity between self-reported and measured weight among a subgroup of the study participants.
INFORMATION:
Funding for the study was provided by the Breast Cancer Research Foundation and the National Institutes of Health's National Cancer Institute (T32 CA009314, P50CA098252, P30CA006973).
Other Johns Hopkins scientists contributing to the research include Betty J. May, Jennifer E. Axilbund, Deborah K. Armstrong and Richard B.S. Roden.
Media Contacts:
Valerie Mehl, 443-375-1991, mehlva@jhmi.edu
Amy Mone, 410-614-2915, amone@jhmi.edu
TORONTO, ON - If it seems like you're pulling more bass than trout out of Ontario's lakes this summer, you probably are.
Blame it on the ripple effect of climate change and warming temperatures. Birds migrate earlier, flowers bloom faster, and fish move to newly warmed waters putting local species at risk.
To mitigate the trend and support conservation efforts, scientists at the University of Toronto (U of T) are sharing a way to predict which plants or animals may be vulnerable to the arrival of a new species.
The researchers looked specifically at the impact of ...
Taking a combination of antidepressants and common painkillers is associated with an increased risk of bleeding soon after starting treatment, finds a study published in The BMJ this week.
The researchers say their results may have been affected by other unmeasured or unknown factors and should be interpreted with caution. However, they suggest special attention is needed when patients use both these classes of drugs together.
Depression produces the greatest decrement in health of all common chronic conditions and depression in older people is an important public ...
Women should be able to treat cystitis themselves with antibiotics without a prescription, says a general practitioner in The BMJ this week.
Dr Kyle Knox says this would save three million scarce GP appointments a year.
Acute uncomplicated urinary tract infections (AUUTIs) such as cystitis are the most common bacterial infections in women. Cystitis affects around half of women at least once in their lifetime and is coded as the reason for 1% of the 300 million GP consultations held annually in the UK.
Management of cystitis is straightforward - a short course of ...
Should doctors recommend homeopathy? Two experts debate the issue in The BMJ this week.
Peter Fisher, Director of Research at the Royal London Hospital for Integrated Medicine, says that of all the major forms of complementary medicine, homeopathy is the most misunderstood.
He questions the methods used to review the evidence for homeopathy. For example, in a recent report by the Australian National Health and Medical Research Council which stated that "there are no health conditions for which there is reliable evidence that homeopathy is effective."
"The fact that ...
Standardised mortality ratios (SMRs) for hospitals do not provide an accurate picture of how many deaths could have been avoided, according to a new study by researchers at the London School of Hygiene & Tropical Medicine and Imperial College London published in the BMJ.
The authors say the widely used hospital-wide standardised mortality ratios, such as HSMR (Hospital Standardised Mortality Ratio) and SHMI (Summary Hospital level Mortality Indicator), should not be used to benchmark hospitals' quality of care.
Hospital-wide SMRs compare the number of deaths in a hospital ...
The first comprehensive genome analyses of 7 melon varieties was completed by a research team led by Josep Casacuberta, Jordi Garcia-Mas and Sebastian Ramos-Onsins, providing breeders new knowledge important for understanding phenotypic variability and helping increasing plant quality yields by selective breeding. The findings were published in the advanced online edition of Molecular Biology and Evolution.
The researchers sought to bridge the gap between expanding the genetic knowledge of melons and understanding important traits such as flavor, size and water use.
The ...
Disruptions in a key brain region can explain the varied outcomes after a traumatic brain injury (TBI) in children and adolescents, according to research published July 15 in The Journal of Neuroscience. Post-injury outcomes vary widely, and injury severity can only explain some of this variance. Combining data from brain imaging and recording, researchers at the University of Southern California and UCLA found that disruptions in the structure and function of a brain region called the corpus callosum could explain the variance in cognitive outcomes.
TBI is the leading ...
Why do some youngsters bounce back quickly from a traumatic brain injury, while others suffer devastating side effects for years?
New UCLA/USC research suggests that damage to the fatty sheaths around the brain's nerve fibers--not injury severity-- may explain the difference. Published in the July 15 edition of the Journal of Neuroscience, the finding identifies possible biomarkers that physicians could use to predict higher-risk patients who require closer monitoring.
The study is the first to combine imaging scans with recording of the brain's electrical activity ...
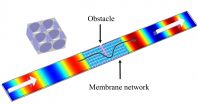
WASHINGTON, DC, July 14, 2015 -- When a sound wave hits an obstacle and is scattered, the signal may be lost or degraded. But what if you could guide the signal around that obstacle, as if the interfering barrier didn't even exist? Recently, researchers at Nanjing University in China created a material from polyethylene membranes that does exactly that.
Their final product, described this week in the Journal of Applied Physics, from AIP Publishing, was an acoustical "metamaterial" with an effective density near zero (DNZ). This work could help to endow a transmission ...
A quick biological test may be able to identify children who have literacy challenges or learning disabilities long before they learn to read, according to new research from Northwestern University.
The study, publishing in the Open Access journal PLOS Biology on July 14th, centers on the child's ability to decipher speech -- specifically consonants -- in a chaotic, noisy environment. Preliterate children whose brains inefficiently process speech against a background of noise are more likely than their peers to have trouble with reading and language development when ...