(Press-News.org) LEBANON, NH - Some melanoma patients respond very well to immunotherapy, experiencing profound and durable tumor regression. A fraction of these patients will also develop autoimmunity against their normal melanocytes--the cells that give rise to melanoma--a phenomenon called vitiligo. Melanoma survivors with vitiligo have long been recognized as a special group with an outstanding prognosis, and a strong response of immune system cells called T cells.
Immunotherapy researchers at Dartmouth's and Dartmouth-Hitchcock's Norris Cotton Cancer Center (NCCC) led by Mary Jo Turk, PhD, and surgical oncologist Christina Angeles, MD (now of University of Michigan), have discovered how a subset of T cells known as memory T cells are generated in melanoma survivors with vitiligo and able to function for years after a tumor is gone.
"We are trying to understand how immune responses against cancer can persist over long periods of time in patients who have excellent responses to immunotherapy," says Turk. "Our study was aimed at discovering where T cells go, what they do and how long they last in these patients. Some T cells last a short time, but others, known as memory T cells, can last for years. The goal of this work was to understand how memory T cells are generated in these patients."
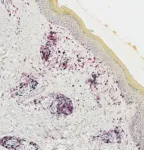
Turk's and Angeles' study found that T cells that enter melanoma tumors also have a tendency to enter a patient's vitiligo-affected skin; that skin accumulates a more focused repertoire of tumor-related T cells than does blood; and that T cells in melanoma tumors are genetically and molecularly very similar to those in vitiligo-affected skin. With these findings, the research team then identified a new subset of "resident memory" (TRM) cells that localize to patient skin and tumor and make high levels of the cytokine interferon gamma. TRM-IFNγ cells have a unique gene expression profile, or "signature," found in melanoma tumors from patients who have survived longer than those who don't have the signature. Turk and Angeles found that T cells that infiltrate tumors have matching clonal partners, or daughter cells, that persist in patient skin and blood up to nine years later.
The team's findings, entitled "Resident and circulating memory T cells persist for years in melanoma patients with durable responses to immunotherapy," are newly published in Nature Cancer. No prior study has demonstrated cellular evidence of such long-lived immunity to cancer. The extensive collaboration between scientists, surgeons, and oncologists required harvesting tumors, blood, and skin from melanoma patients over a period of several years. Patient specimens were analyzed using state-of-the-art technologies called single cell RNA sequencing and T cell receptor sequencing.
These studies were done with a subset of T cells called cytotoxic or "CD8" T cells. Turk and Angeles next want to understand if similar features are seen in patient-helper or "CD4" T cells, and if similar immunity is generated in patients with skin inflammation aside from vitiligo, such as rash. The team will also investigate how different types of immunotherapy affect the new cell population that they discovered.
"Finding that T cells can persist for years throughout skin and blood and understanding what defines such durable immune responses in melanoma patients will lead to better design of therapies to achieve such responses," says Turk.
INFORMATION:
Co-leading this work was Christina Angeles, MD, FACS, who designed and led clinical aspects of the study while at NCCC and serves as co-corresponding author on the paper. Angeles is now a surgical oncologist at Rogel Cancer Center, University of Michigan.
Mary Jo Turk, PhD, is the Co-Director of the Immunology and Cancer Immunotherapy Research Program at Dartmouth's and Dartmouth-Hitchcock's Norris-Cotton Cancer Center and the O. Ross McIntyre, MD, Endowed Professor and Professor of Microbiology and Immunology at the Geisel School of Medicine at Dartmouth. Her laboratory's immunotherapy research focuses on generating durable memory T cell responses for long-lived immunity to cancer.
About Norris Cotton Cancer Center
Norris Cotton Cancer Center, located on the campus of Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, NH, combines advanced cancer research at Dartmouth College's Geisel School of Medicine in Hanover, NH with the highest level of high-quality, innovative, personalized, and compassionate patient-centered cancer care at DHMC, as well as at regional, multi-disciplinary locations and partner hospitals throughout NH and VT. NCCC is one of only 51 centers nationwide to earn the National Cancer Institute's prestigious "Comprehensive Cancer Center" designation, the result of an outstanding collaboration between DHMC, New Hampshire's only academic medical center, and Dartmouth College. Now entering its fifth decade, NCCC remains committed to excellence, outreach and education, and strives to prevent and cure cancer, enhance survivorship and to promote cancer health equity through its pioneering interdisciplinary research. Each year the NCCC schedules 61,000 appointments seeing nearly 4,000 newly diagnosed patients, and currently offers its patients more than 100 active clinical trials.
About Dartmouth-Hitchcock Health
Dartmouth-Hitchcock Health (D-HH), New Hampshire's only academic health system and the state's largest private employer, serves a population of 1.9 million across northern New England. D-H provides access to more than 2,000 providers in almost every area of medicine, delivering care at its flagship hospital, Dartmouth-Hitchcock Medical Center (DHMC) in Lebanon, NH. DHMC was named again in 2020 as the #1 hospital in New Hampshire by U.S. News & World Report, and recognized for high performance in 9 clinical specialties and procedures. Dartmouth-Hitchcock also includes the Norris Cotton Cancer Center, one of only 51 NCI-designated Comprehensive Cancer Centers in the nation; the Children's Hospital at Dartmouth-Hitchcock, the state's only children's hospital; affiliated member hospitals in Lebanon, Keene, and New London, NH, and Windsor, VT, and Visiting Nurse and Hospice for Vermont and New Hampshire; and 24 Dartmouth-Hitchcock clinics that provide ambulatory services across New Hampshire and Vermont. The D-H system trains nearly 400 residents and fellows annually, and performs world-class research, in partnership with the Geisel School of Medicine at Dartmouth and the White River Junction VA Medical Center in White River Junction, VT.
About Geisel School of Medicine at Dartmouth
Founded in 1797, the Geisel School of Medicine at Dartmouth strives to improve the lives of the communities it serves through excellence in learning, discovery, and healing. The Geisel School of Medicine is renowned for its leadership in medical education, healthcare policy and delivery science, biomedical research, global health, and in creating innovations that improve lives worldwide. As one of America's leading medical schools, Dartmouth's Geisel School of Medicine is committed to training new generations of diverse leaders who will help solve our most vexing challenges in healthcare.
The ocean is dynamic in nature, playing a crucial role as a planetary thermostat that buffer global warming. However, in response to climate change, the ocean has generally become stabler over the past 50 years. Six times stabler, in fact, than previously estimated--as shown by a new study that researchers from the CNRS, Sorbonne University, and IFREMER have conducted within the scope of an international collaboration.* Warming waters, melting glaciers, and disrupted precipitation patterns have created an ocean surface layer cut off from the depths. Just as oil and ...
Training babies' brains and bodies might delay the onset of Rett syndrome, a devastating neurological disorder that affects about 1 in 10,000 girls worldwide.
In experiments with mice that replicate the genetic disorder, scientists discovered that intense behavioral training before symptoms develop staves off both memory loss and motor control decline. Compared to untrained mice, those trained early in life were up to five times better at performing tasks that tested their coordination or their ability to learn, Howard Hughes Medical Institute Investigator Huda Zoghbi and her colleagues report March 24, 2021, in the journal Nature.
Those data, from animals whose symptoms closely mimic the human disease, offers a clear rationale for genetically screening newborns for Rett syndrome, ...
New York, NY (March 24, 2021) -- Immunotherapy is not only significantly less effective in liver cancer patients who previously had a liver disease called non-alcoholic steatohepatitis (NASH), but actually appears to fuel tumor growth, according to a Mount Sinai study published in Nature in March. NASH affects as many as 40 million people worldwide and is associated with obesity and diabetes.
The researchers led a large international collaboration to investigate immunotherapy's effect on hepatocellular carcinoma (HCC), a deadly liver cancer, caused by NASH. They conducted a meta-analysis ...
New scientific findings bring hope that early training during the presymptomatic phase could help individuals with Rett syndrome, a neurodevelopmental disorder, retain specific motor and memory skills and delay the onset of the condition. Researchers at Baylor College of Medicine and the Jan and Dan Duncan Neurological Research Institute at Texas Children's Hospital reported in the journal Nature that, in a mouse model of Rett syndrome, intensive training beginning before symptoms appear dramatically improved the performance of specific motor and memory tasks and substantially delayed the appearance of symptoms.
The researchers propose that newborn genetic testing for Rett syndrome, followed by prompt intensive training in the skills that will be affected, such ...
Immunotherapy using checkpoint inhibitors is effective in around a quarter of patients with liver cancer. However, to date, physicians have been unable to predict which patients would benefit from this type of treatment and which would not. Researchers from the German Cancer Research Center have now discovered that liver cancer caused by chronic inflammatory fatty liver disease does not respond to this treatment. On the contrary: in an experimental model, this type of immunotherapy actually promoted the development of liver cancer, as now reported in the journal Nature.
Liver cancer is the sixth most common type of cancer in the world, ...
The heart of any computer, its central processing unit, is built using semiconductor technology, which is capable of putting billions of transistors onto a single chip. Now, researchers from the group of Menno Veldhorst at QuTech, a collaboration between TU Delft and TNO, have shown that this technology can be used to build a two-dimensional array of qubits to function as a quantum processor. Their work, a crucial milestone for scalable quantum technology, was published today in Nature.
Quantum computers have the potential to solve problems that are impossible to address with classical computers. Whereas current ...
HOUSTON ? Overcoming previous technical challenges with single-cell DNA (scDNA) sequencing, a group led by researchers at The University of Texas MD Anderson Cancer Center has developed a novel method for scDNA sequencing at single-molecule resolution. This technique revealed for the first time that triple-negative breast cancers undergo continued genetic copy number changes after an initial burst of chromosome instability.
The findings, published today in Nature, offer an accurate and efficient new approach for sequencing hundreds of individual cancer cells while also providing novel insights into cancer evolution. These insights may explain why treatments are ...
Joint press release by the German Cancer Research Center, University Medicine Mannheim, Heidelberg University Hospital, and the National Center for Tumor Diseases (NCT) Heidelberg
Tumor vaccines can help the body fight cancer. Mutations in the tumor genome often lead to protein changes that are typical of cancer. A vaccine can alert the patients' immune system to these mutated proteins. For the first time, physicians and cancer researchers from Heidelberg and Mannheim have now carried out a clinical trial to test a mutation-specific vaccine against malignant brain tumors. The vaccine proved to be safe and triggered the desired immune response in the tumor tissue, as the team now reports in the journal Nature.
Diffuse ...
Researchers have developed experimental flu shots that protect animals from a wide variety of seasonal and pandemic influenza strains. The vaccine product is currently being advanced toward clinical testing. If proven safe and effective, these next-generation influenza vaccines may replace current seasonal options by providing protection against many more strains that current vaccines do not adequately cover.
A study detailing how the new flu vaccines were designed and how they protect mice, ferrets, and nonhuman primates appears in the March 24 edition of the journal Nature. This work was led by researchers at the University of Washington School of Medicine and the Vaccine
Research Center part of the National Institute of Allergy ...
Many children of low-income families across the country do not have access to quality health care. Lack of health care can have a domino effect, affecting educational outcomes in the classroom.
School-based telehealth could offer a sustainable and effective solution, according to a new report in the Journal for Nurse Practitioners by Kathryn King Cristaldi, M.D., the medical director of the school-based telehealth program, and Kelli Garber, the lead advanced practice provider and clinical integration specialist for the program.
The program through the MUSC Health Center for Telehealth has effectively served over 70 schools across the state of South Carolina. Evaluating a child at school via telehealth ...