(Press-News.org)
The first prospective study comparing outcomes in patients with pituitary apoplexy—sudden bleeding or death of a pituitary tumor—found that patients managed medically fared as well as those treated surgically in the majority of cases. The multicenter international study, led by Cedars-Sinai investigators, was presented today at the American Association of Neurological Surgeons Scientific Meeting in Los Angeles.
“This is the best data to date on the question of surgery versus medical management in patients with this rare but serious condition,” said Adam Mamelak, MD, co-director of the Pituitary Center and director of the Functional Neurosurgery Program at Cedars-Sinai and lead author of the study. “It demonstrates in a prospective, controlled way what previous studies had begun to suggest, namely that pituitary apoplexy is very rarely a surgical emergency.”
The pituitary gland, located at the base of the brain, controls the function of several hormone-producing glands. Pituitary apoplexy occurs when a benign tumor in the pituitary gland area begins to bleed or dies, causing the tumor to grow and press on the surrounding brain tissues. This, in turn, causes symptoms such as severe headache, fatigue, confusion, and vision problems including vision loss. Most commonly, these tumors are undetected prior to the apoplexy event.
To relieve the pressure on brain tissues and the symptoms of apoplexy, patients can either have the tumor surgically removed or be treated with medications to relieve pain and other symptoms while they wait for it to naturally shrink over time. In both cases, patients generally also need hormone replacement therapy, Mamelak said.
Pituitary apoplexy has long been considered an emergency requiring rapid surgical treatment to achieve best results. Small retrospective studies, where investigators look back at previously collected data, have suggested that pituitary apoplexy patients have equally good outcomes with medical management, but these observations have failed to significantly change clinical practice.
“While we've seen a growing trend toward clinicians being a little more comfortable with medical management of pituitary apoplexy, in general, most patients still end up getting surgery,” Mamelak said. “Those small retrospective studies really didn’t move the needle that much.”
To provide a more solid basis for clinical decision making, Mamelak and fellow investigators from the Department of Neurosurgery and the Pituitary Center at Cedars-Sinai—as well as colleagues from 11 other medical centers in North America, Japan, South Korea and Europe—developed the Pituitary Apoplexy Surgical Timing & Outcomes Registry (PASTOR).
The registry enrolled 97 patients with pituitary apoplexy at the time of diagnosis and compared outcomes for the 67 patients who had surgery with those for the 30 patients whose symptoms were medically managed. This type of prospective registry allows investigators to draw stronger conclusions because data collection is the same for all participants.
Investigators found that:
Length of hospital stay was the same for patients who had surgery as for those who did not.
Patients who had surgery experienced the same outcomes whether they had surgery right away or days after the onset of symptoms.
There were no statistically significant differences in hormone function, vision or quality of life between the two groups of patients three and six months after treatment.
Mamelak noted that patients experiencing more severe vision symptoms were more likely to have surgery than those experiencing milder symptoms, but that surgery didn’t necessarily lead to better outcomes.
“Cedars-Sinai and the other sites taking part in this study all have expert pituitary neurosurgery and endocrinology teams, which could help account for the positive outcomes experienced by surgical patients,” said Keith L. Black, MD, chair of the Department of Neurosurgery and the Ruth and Lawrence Harvey Chair in Neuroscience at Cedars-Sinai. “A wealth of solid research tells us that outcomes from pituitary surgery are directly tied to surgical experience.”
Mamelak said that further research specifically looking at outcomes for people with visual field deficits would be needed to determine whether surgery is best in those cases. Meanwhile, the current findings could especially benefit medical centers that do not have the expertise to surgically treat pituitary tumors.
“These findings take some of the urgency out of managing these cases,” Mamelak said. “Clinicians at these centers now know that they can safely manage these patients medically and transfer them when it’s reasonable and available, or allow patients to forgo surgery entirely if they are comfortable with that.”
Also at the conference:
David Skaggs, MD, executive vice chair of the Department of Orthopaedics at Cedars-Sinai and director of Pediatric Orthopaedics at Cedars-Sinai Guerin Children’s, can discuss the future of pediatric spine surgery.
Wouter Schievink, MD, director of the Microvascular Neurosurgery Program at Cedars-Sinai, can discuss diagnosis and management of headache in patients with spontaneous intracranial hypotension, in which the pressure of cerebrospinal fluid inside the skull is lower than normal.
Chirag Patil, MD, director of the Center for Neurosurgical Outcomes Research at Cedars-Sinai, can discuss outcomes and mortality in older patients who undergo surgical evacuation of subdural hematoma, where a blood clot places pressure on the brain. END
The American Association for the Advancement of Science’s (AAAS) inaugural Mani L. Bhaumik Breakthrough of the Year Award — focused on standout contributors to NASA’s James Webb Space Telescope (JWST) — honors three individuals who supported vast swaths of the JWST community over decades and whose persistence amid multiple setbacks ensured the mission’s completion.
The award recognizes Major General Charles Frank Bolden Jr., USMC (Ret), a former administrator of the National Aeronautics and Space Administration (NASA); John Mather, senior project scientist of the JWST since 1995; and Bill Ochs, JWST project manager from 2011 through the telescope’s ...
Study’s findings suggest that maintaining normal vitamin D levels may benefit patients.
New research indicates that for patients with advanced skin cancer, it may be important to maintain normal vitamin D levels when receiving immunotherapy medications called immune checkpoint inhibitors. The findings are published by Wiley online in CANCER, a peer-reviewed journal of the American Cancer Society.
Vitamin D has many effects on the body, including regulation of the immune system. To see whether levels of vitamin D might impact the effectiveness of immune checkpoint inhibitors, investigators analyzed the blood of 200 patients with advanced melanoma both before and every 12 weeks ...
Despite the promise of new medications that promote cancer cell death in people with acute myeloid leukemia, leukemic cells often adopt features that let them evade the drugs’ effects within a year.
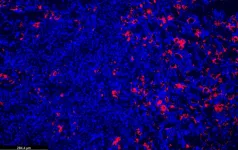
Now, new research using human tissue samples and mouse models has found that resistance of leukemia cells to a widely prescribed drug called venetoclax occurs because of a rapid increase in the breakdown and turnover of mitochondria, structures inside the cell that help power its functions. In addition to their role in producing energy, mitochondria also tell cells to die under certain adverse conditions.
This process of “programmed cell ...
A new study by researchers at Uppsala University and Uppsala University Hospital shows that men who have a neurodevelopmental disorder, such as autism and ADHD, also have a slightly increased risk of testicular cancer, or seminoma. This is the first study to show such a link, with the results to be published in the British Journal of Cancer.
Testicular cancer is the most common form of cancer in young men, and its underlying causes are still largely unknown.
“As testicular cancer can be surgically removed, thus curing the disease, it is important to seek care in time if you feel a lump in your testicle,” notes Ingrid ...
For children under age 18 years, a single computed tomography (CT) scan is not associated with an increased risk of brain tumours, leukemia or lymphoma, but exposure to 4 or more scans before adulthood more than doubles the risk, according to new research https://www.cmaj.ca/lookup/doi/10.1503/cmaj.221303 in CMAJ (Canadian Medical Association Journal).
Computed tomography in children has increased worldwide in recent decades, but there is conflicting evidence about the risks of cancer from these ...
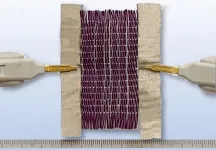
A new smart material developed by researchers at the University of Waterloo is activated by both heat and electricity, making it the first ever to respond to two different stimuli.
The unique design paves the way for a wide variety of potential applications, including clothing that warms up while you walk from the car to the office in winter and vehicle bumpers that return to their original shape after a collision.
Inexpensively made with polymer nano-composite fibres from recycled plastic, the programmable fabric can change its colour and shape when stimuli are applied.
“As a wearable material alone, it has almost infinite potential ...
A major international trial has concluded that, where possible, surgeons should replace the removed section of the skull following surgery to treat a form of brain haemorrhage. This approach will save patients from having to undergo skull reconstruction further down the line.
The RESCUE-ASDH trial, funded by the UK’s National Institute for Health and Care Research (NIHR), involved 40 centres in 11 countries and involved 450 patients. The results of the trial are published today in the New England Journal of Medicine and are announced at the annual meeting of the American Association of Neurological ...
If more people have access to health insurance, we have to be sure the death rates of those with certain chronic conditions are decreasing.
This is one of the statements Gregory Peck, an acute care surgeon and associate professor at Rutgers Robert Wood Johnson Medical School, will be researching on behalf of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) at the National Institutes of Health.
Funded by NIH grants totaling more than $1 million through a recent two-year award from the New Jersey Alliance for Clinical and Translational Science (NJ ACTS), a Rutgers hub of the National Center for Advancing ...
A discovery about gene variants of an inflammation ‘brake’ brings scientists a step closer to personalised treatment for patients at risk of kidney disease and kidney failure.
Researchers at the Garvan Institute of Medical Research, University of New South Wales, Sydney and Westmead Hospital, found that common genetic variants of TNFAIP3, which increase inflammation in the body, can paradoxically protect the kidneys from damage in the short term.
“We wanted to investigate whether inherited differences in how people regulate inflammation could lead to better or worse kidney health outcomes,” says Professor Shane ...
Just over a century has passed since the discovery of insulin, a time period during which the therapeutic powers of the hormone have broadened and refined. Insulin is an essential treatment for type 1 diabetes and often for type 2 diabetes, as well. Roughly 8.4 million Americans use insulin, according to the American Diabetes Association.
One hundred years of research have greatly advanced medical and biochemical understanding of how insulin works and what happens when it is lacking, but the reverse, how potentially fatal insulin hyper-responsiveness is prevented, has remained a persistent mystery.
In a new study, published in the April 20, 2023 online edition ...