“We hope that this proof-of-concept study is the first of many applications of engineered plasma B cells, and eventually will lead to a single-shot therapeutic,” says senior study author Richard James (@ScienceRicker) of the Seattle Children’s Research Institute. “Because engineered plasma B cells can live for a very long time, greater than 10 years, they could be used as a long-term source of many biologic drugs.”
Immunotherapies that recruit cytotoxic T cells to kill cancer cells, such as bispecific antibodies, have contributed to improved survival rates for patients with B cell acute lymphoblastic leukemia (B-ALL). Blinatumomab is a bispecific antibody that received FDA approval in 2014 for the treatment of patients with relapsed/refractory B-ALL, but a limitation of blinatumomab is that it requires continuous high-dose intravenous infusions to maintain activity. This intensive regimen poses challenges for patients because frequent bag changes prove inconvenient, and the use of ports increases the risk of infection.
“Bispecific non-immunoglobulin therapies pose stability challenges in patients, necessitating three courses of 20-day steady-state infusion,” James says. “Enhanced drug delivery methods for bispecific antibodies like blinatumomab could improve patient adherence and bolster treatment efficacy.”
“We think that the first application of engineered plasma B cells will be to produce drugs that are difficult for patients to use,” James says. “In this study, we wanted to demonstrate proof of concept and efficacy for engineered B cell therapies.”
Toward that goal, James and his team developed a gene-editing strategy for the generation of ePCs that produce large quantities of bispecifics to target B-ALL or acute myeloid leukemia. The combined findings demonstrated that ePCs secreting bispecifics can promote T cell-driven killing of primary human cells and human leukemic cell lines.
“One challenge we encountered was that the bispecific antibody used for killing tumor cells can also bind the engineered plasma B cells because they express the same target protein,” James says. “To overcome this challenge, we deleted the protein target of the antibody, CD19, when we were making the engineered cells. We were surprised that deletion of CD19 did not hinder manufacturing of engineered plasma B cells.”
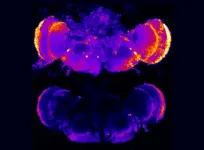
In addition, the researchers discovered that plasma cells secreting anti-CD19 bispecific antibodies elicited antitumor activity, as demonstrated with acute lymphoblastic leukemia patient-derived xenografts in immunodeficient mice co-engrafted with autologous T cells. Notably, the steady-state concentration of anti-CD19 bispecifics in serum one month after cell delivery and tumor eradication was comparable to that observed in patients treated with continuous infusion of blinatumomab.
Based on the results, the researchers propose that ePC strategies could increase the functional half-life of bispecifics in patients with acute leukemias and other diseases where treatment half-life is limiting or where plasma cell local delivery could enhance therapeutic efficacy.
The results suggest that prolonged clinically relevant levels of bispecific and perhaps other biologics can be achieved via a single administration of ePCs. The robust levels of bispecific achieved by ePCs compare favorably to those observed by other bispecific-secreting cell products, including macrophages and T cells. According to the authors, these findings support further development of ePCs for use as a durable delivery system for the treatment of acute leukemias and potentially other cancers.
“We created engineered plasma B cells capable of continuously producing bispecific antibodies throughout the treatment period after only one injection,” James says. “These cells effectively eliminated tumors to a comparable extent as the clinical drug. The key takeaway is that engineered plasma B cells can provide long-lasting drug production in vivo.”
However, ePC bispecifics should be carefully evaluated for several possible toxicities if used clinically. Persistent on-target, off-tumor toxicity to normal bystander B cells is common in patients receiving B cell-targeted therapeutics. “In addition, for treatment of a B cell malignancy, it may be difficult to engineer a patient’s own B cells to be used as the therapy because there is a risk that some of the B cells will be cancerous,” James says. “We did not test whether we can use a different person’s B cells to produce the bispecific antibody. Studies using such allogeneic products will likely need to be done before this specific therapy can be used to treat B cell cancers.”
As noted by the authors, further studies in humanized mice and non-human primates are warranted to fully understand the activity, longevity, and tissue localization of ePCs. “In the short term, we plan to test whether engineered plasma B cells that produce bispecific antibodies are effective in other B cell-mediated diseases, including autoimmunity. These tests will initially be conducted in animal models. Additionally, we are developing engineered plasma B cells to produce other therapeutic drugs, such as those needed in protein deficiency diseases such as hemophilia. Finally, we are exploring additional applications of engineered B cells, including modifying other immune cells to either enhance or suppress the immune system.”
###
Some of the authors have an equity ownership position in Be Biopharma Incorporated, are employees and shareholders of Be Biopharma Incorporated, and/or have filed a provisional patent application covering applications of binders secreted from B cells and plasma cells. Please see the paper text for more information.
Molecular Therapy, Hill et al. “Human plasma cells engineered to secrete bispecifics drive effective in vivo leukemia killing” https://www.cell.com/molecular-therapy/fulltext/S1525-0016(24)00386-1
Molecular Therapy (@MolTherapy), published by Cell Press for the American Society of Gene & Cell Therapy, is a monthly journal for international research on the development of molecular and cellular therapeutics to correct genetic and acquired diseases, including but not limited to research on gene transfer and editing, vector development and design, stem cell manipulation, vaccine development, pre-clinical target validation, safety/efficacy studies, and clinical trials. To receive Cell Press media alerts, contact press@cell.com.
END