(Press-News.org) KEY TAKEAWAYS
After implementing a new hospice transition program, 210 out of 388 patients (54.1 percent) at Brigham and Women’s Hospital transitioned to hospice from the emergency department (ED) within 96 hours, compared to 61 of 270 patients (22.1 percent) in the control period.
Across all groups, the presence of a Medical Order for Life-Sustaining Treatment plan (MOLST), was independently associated with hospice transition.
These findings suggest that hospice transition programs can help improve use of hospice for patients presenting at the ED near the end of life who would benefit from hospice care.
For patients who are in the final stages of both gradual and sudden terminal illnesses, hospice care can provide safe, comfortable, and dignified care at the end of life. However, many patients, especially those with complex diseases and treatments, may end up in an emergency department and either die there or die shortly after being admitted into inpatient care at a hospital, despite their goals of care being better aligned with hospice care. Researchers from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, have designed and implemented a new program to streamline the process of transitioning patients from the emergency department into hospice care.
In a test population that included 270 patients, 54.1 percent transitioned to hospice within 96 hours of arriving in the Emergency Department, compared to 22.1 percent in the control group of patients before the new program started in 2021. The findings suggest that such programs may help adult patients who present to the ED near the end of life avoid delayed or missed transitions to hospice care. Results are published in JAMA Network Open.
“When patients come to an emergency department near end of life, the default is typically to admit them to the hospital, engage them in conversations about goals and end-of-life care and potentially move them into hospice care. However, this lengthy progress can take longer than the patient has left to live,” said first author Christopher Baugh, MD, MBA, an emergency physician in the Department of Emergency Medicine at the Brigham. “This program helps us identify patients who may be eligible for hospice as quickly as possible while they are still in the ED and reduce the time it takes to get them into hospice care.”
To identify patients who may be hospice eligible, the researchers implemented an artificial intelligence algorithm that analyzes electronic health record data as it is recorded by ED staff. This, along with dedicated care management and emergency department rounds to evaluate patients in person, flags potential candidates for the transition program. These candidates, instead of being admitted as an inpatient to the hospital, were placed under an outpatient observation status, where the final decision was ultimately made by the patient and their family or caregivers, guided by a multidisciplinary team of an ED care facilitator in consultation with the Brigham’s palliative care team and specialists such as oncologists or neurosurgeons as needed. Hospice teams were then available with 1-2 hours to start providing care.
“Identifying hospice candidates quickly after ED arrival mostly falls on the shoulders of ED clinicians, so our goal with the program is to make this process as simple and efficient as possible,” said Baugh. “With our approach, we’re able to mobilize the hospice transition within one to two days most times, which is must faster than would be possible if the patient was admitted directly into inpatient care.”
While this new process helped transition a greater number of patients into hospice, the researchers emphasize that the program on its own is not enough to fully address the challenges that come with aligning care with patients end-of-life goals and helping patients die with dignity. The findings also revealed that having a Medical Order for Life-Sustaining Treatment (MOLST) plan, a legal document that codifies a patient’s goals for end-of-life care, was associated with successfully transitioning to hospice in both the test and control groups.
On the provider side, the program also introduced biannual virtual education on the benefits of the program and the need for timely hospice transitions. This training will continue to be provided to emergency clinicians, including nurses, physicians’ assistants and trainees in addition to doctors themselves.
“It’s been incredibly moving to witness the care delivered by our multi-disciplinary program, and the impact on patients and families,” said senior author Mallika L. Mendu, MD, MBA, vice president of clinical operations and care continuum at the Brigham. “As a result of this program, patients and families are receiving meaningful support at a critical point in their lives, which can have a long-lasting impact on bereaved loved ones. Importantly, the program facilitates timely transition to hospice care as early as when they present to the ED, which is crucial during this current period of capacity crisis, in which patients have experienced delays in receiving care.”
Authorship: In addition to Baugh and Mendu, BWH authors include Kei Ouchi, Jason K. Bowman, Ayal A. Aizer, Alexander W. Zirulnik, Martha Wadleigh, Richard E. Leiter Bradley J. Molyneaux, Panupong Hansrivijit Kate Lally, Melissa Littlefield Alexei M. Wagner, Katherine H. Walker, Hojjat Salmasian, Kourosh Ravvaz, Karen Lewis Brownell, Matthew P. Vitale, Frantzie C. Firmin, James A. Tulsky, Soumi Ray, LynneM. O’Mara, and Elizabeth M. Rickerson. Additional authors include Angela Wise, Paula Remón Baranda, Andrea McCabe, Jada A. Devlin, Nelia Jain and Jane deLima Thomas.
Disclosures: Aizer reported receiving grants from Varian and NH TherAguix; and personal fees from Seagen and Novartis outside the submitted work. Leiter reported receiving royalties from UpToDate for a chapter on ethical considerations for pain management in end-of-life care, outside the submitted work. Molyneaux reported serving on the clinical trial scientific advisory board for Biogen outside the submitted work. No other disclosures were reported.
Funding: The researchers did not receive external funding for this research.
Papers cited: Baugh, C. et al. “A Hospice Transitions Program for Patients in the Emergency Department JAMA Network Open. DOI:10.1001/jamanetworkopen.2024.20695
END
Brigham study finds new program streamlined hospice transitions from the emergency department
Researchers found that a new program more than doubled hospice transitions for patients at end of life, increasing transitions within 96 hours of ED arrival to 54.1 percent
2024-07-08
ELSE PRESS RELEASES FROM THIS DATE:
Diet quality among children
2024-07-08
About The Study: Although total dietary quality scores among U.S. children improved overall during 2005-2020, the increase remained suboptimal: lower than 5 points, a significant threshold for children in this analysis of changes in diet quality.
Corresponding Author: To contact the corresponding author, Yongjun Zhang, Ph.D., M.D., email zhangyongjun@sjtu.edu.cn.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamapediatrics.2024.1880)
Editor’s Note: Please see the article for additional information, ...
Acceptability of hospital-at-home care and capacity for caregiver burden
2024-07-08
About The Study: Survey respondents reported substantial acceptability of hospital-at-home care, which did not vary across sociodemographics, health insurance coverage, health status, prior hospitalizations, or telehealth use. Approximately half of respondents agreed that hospital-at-home care was effective, safe, and convenient. Most indicated capacity to perform many caregiver tasks.
Corresponding Author: To contact the corresponding author, Melissa A. Frasco, Ph.D., email mfrasco@usc.edu.
To access the embargoed ...
Semaglutide vs tirzepatide for weight loss in adults with overweight or obesity
2024-07-08
About The Study: In this population of adults with overweight or obesity, use of tirzepatide was associated with significantly greater weight loss than semaglutide. Future study is needed to understand differences in other important outcomes.
Corresponding Author: To contact the corresponding author, Nicholas L. Stucky, M.D., email nicholass@truveta.com.
To access the embargoed study: Visit our For The Media website at this link https://media.jamanetwork.com/
(doi:10.1001/jamainternmed.2024.2525)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflict of interest ...
AJPH study shows that permit to purchase laws are a promising avenue to reduce suicides in young adults
2024-07-08
In 2020, suicide ranked as the third leading cause of death for adults aged 18 to 20 years in the United States. Firearms were implicated in approximately half of these cases, and by 2017, they had surpassed motor vehicles as the leading cause of death in this age group. While ongoing debates on gun violence and mental health have increased public support for restricted firearm access, not much is known about the impact of gun control policies on young adults.
To fill this knowledge gap, a recent study published in the August issue of the American Journal of Public Health on July 03, ...
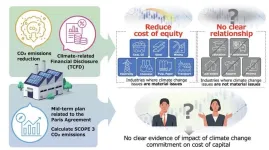
Companies that mitigate climate change reduce their cost of capital
2024-07-08
Fukuoka, Japan —The climate crisis is hitting home with more frequent extreme weather events. Companies, particularly those in high-emission industries, are major contributors to global carbon emissions, therefore making them key players in the fight against climate change. Recognizing this responsibility, many businesses are now taking proactive measures to reduce their carbon footprint, by reducing carbon emissions and transparently sharing their environmental strategies and data.
The Task Force on Climate-Related Financial Disclosures ...
Case Western Reserve University receives $1.5M grant from Foundation Fighting Blindness to test possible new treatment for inherited retinal disease
2024-07-08
CLEVELAND—There’s only one U.S. Food and Drug Administration-approved therapy for an inherited retinal disease, and dozens of retinitis pigmentosa (RP) genes for which no therapy is available.
With a new three-year, $1.5 million grant from the Foundation Fighting Blindness, Shigemi Matsuyama, an associate professor of ophthalmology and visual sciences at the Case Western Reserve University School of Medicine, will test a possible breakthrough drug that can be taken by mouth—one that may address many RP disease manifestations, regardless of the underlying genetic mutation.
“We believe it can serve as the basis of an oral medicine to prevent blindness in RP ...
How to stop cancer cachexia? Start at the top
2024-07-08
Cancer is insidious. Throughout tumor progression, the disease hijacks otherwise healthy biological processes—like the body’s immune response—to grow and spread. When tumors elevate levels of an immune system molecule called Interleukin-6 (IL-6), it can cause severe brain dysfunction. In about 50%-80% of cancer patients, this leads to a lethal wasting disease called cachexia. “It’s a very severe syndrome,” says Cold Spring Harbor Laboratory (CSHL) Professor Bo Li.
“Most people with cancer die of cachexia instead of cancer. And once the patient enters this stage, there’s ...
Pulsed field ablation procedures found safe and effective for atrial fibrillation patients
2024-07-08
Pulsed field ablation (PFA) is safe for treating patients with common types of atrial fibrillation (AF), according to the largest study of its kind on this new technology, led by the Icahn School of Medicine at Mount Sinai.
The “MANIFEST-17K” international study is the first to show important safety outcomes in a large patient population, including no significant risk of esophageal damage, with PFA. PFA is the latest ablation modality approved by the Food and Drug Administration that can be used to restore a regular heartbeat. The findings, published July 8 in Nature Medicine, could lead to more frequent use of PFA instead of conventional therapies to manage AF patients.
“MANIEFST-17K ...
Why some abusive bosses get a pass from their employees
2024-07-08
COLUMBUS, Ohio – Why do employees sometimes accept working for an abusive boss?
A new study suggests that when a leader is seen as a high performer, employees are more likely to label abuse as just “tough love.”
Results showed that workers were less likely to show hostility to abusive bosses when the leader’s performance was high, and employees were even likely to think their career could be boosted by a successful – if abusive – boss.
The findings suggest that employees may be reluctant to call a successful boss abusive – ...
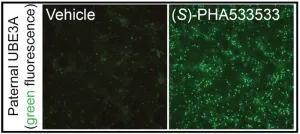
UNC researchers identify potential treatment for Angelman syndrome
2024-07-08
CHAPEL HILL, N.C. – Angelman syndrome is a rare genetic disorder caused by mutations in the maternally-inherited UBE3A gene and characterized by poor muscle control, limited speech, epilepsy, and intellectual disabilities. Though there isn't a cure for the condition, new research at the UNC School of Medicine is setting the stage for one.
Ben Philpot, PhD, the Kenan Distinguished Professor of Cell Biology and Physiology at the UNC School of Medicine and associate director of the UNC Neuroscience Center, and his lab have identified a small molecule that could be safe, non-invasively delivered, and capable of ...
LAST 30 PRESS RELEASES:
Low-intensity treadmill exercise preconditioning mitigates post-stroke injury in mouse models
How moss helped solve a grave-robbing mystery
How much sleep do teens get? Six-seven hours.
Patients regain weight rapidly after stopping weight loss drugs – but still keep off a quarter of weight lost
GLP-1 diabetes drugs linked to reduced risk of addiction and substance-related death
Councils face industry legal threats for campaigns warning against wood burning stoves
GLP-1 medications get at the heart of addiction: study
Global trauma study highlights shared learning as interest in whole blood resurges
Almost a third of Gen Z men agree a wife should obey her husband
Trapping light on thermal photodetectors shatters speed records
New review highlights the future of tubular solid oxide fuel cells for clean energy systems
Pig farm ammonia pollution may indirectly accelerate climate warming, new study finds
Modified biochar helps compost retain nitrogen and build richer soil organic matter
First gene regulation clinical trials for epilepsy show promising results
Life-changing drug identified for children with rare epilepsy
Husker researchers collaborate to explore fear of spiders
Mayo Clinic researchers discover hidden brain map that may improve epilepsy care
NYCST announces Round 2 Awards for space technology projects
How the Dobbs decision and abortion restrictions changed where medical students apply to residency programs
Microwave frying can help lower oil content for healthier French fries
In MS, wearable sensors may help identify people at risk of worsening disability
Study: Football associated with nearly one in five brain injuries in youth sports
Machine-learning immune-system analysis study may hold clues to personalized medicine
A promising potential therapeutic strategy for Rett syndrome
How time changes impact public sentiment in the U.S.
Analysis of charred food in pot reveals that prehistoric Europeans had surprisingly complex cuisines
As a whole, LGB+ workers in the NHS do not experience pay gaps compared to their heterosexual colleagues
How cocaine rewires the brain to drive relapse
Mosquito monitoring through sound - implications for AI species recognition
UCLA researchers engineer CAR-T cells to target hard-to-treat solid tumors
[Press-News.org] Brigham study finds new program streamlined hospice transitions from the emergency departmentResearchers found that a new program more than doubled hospice transitions for patients at end of life, increasing transitions within 96 hours of ED arrival to 54.1 percent