Maintaining good health and well-being is crucial for how well patients respond to cancer treatments. Unfortunately, cachexia, or involuntary weight loss, is a major concern for many individuals with advanced cancer. A new study from Japan has revealed that lower cachexia rates, particularly with prevalence less than 40–50%, are linked to shorter overall survival (OS) rates. The study also showed that the diagnostic criteria used for cachexia detection can affect the reported cachexia prevalence.
People with advanced heart disease or cancer often face serious health challenges. Cachexia, an involuntary loss of weight, affects about 11% to 71% of cancer patients. This condition can disrupt essential chemotherapy, lower quality of life, and reduce overall survival (OS)—the length of time that cancer patients live after being diagnosed or starting treatment. Cachexia leads to a continuous loss of muscle mass, with or without fat loss, which cannot be remedied by conventional nutritional support, creating ongoing difficulties with daily activities. Various diagnostic methods exist for cachexia detection, each predicting different survival outcomes. However, the lack of a consistent diagnostic approach creates challenges for the assessment of cachexia prevalence and its actual impact on survival rates.
To bridge this gap, Mr. Tomoya Takaoka, a registered dietician at the Division of Clinical Nutrition at Shinshu University Hospital, Japan, collaborated with Dr. Daiki Watanabe, Assistant Professor at Waseda University, and Dr. Akinori Yaegashi, Assistant Professor at Hokkaido Bunkyo University. Their findings were made available online on August 8, 2024, and published in Volume 15, Issue 9 of the journal Advances in Nutrition on September 1, 2024.
They aimed to understand the impact of cachexia diagnosis on OS in cancer patients. The lead author, Takaoka, explains, “If prevalence and OS are affected by differences in diagnostic criteria for cachexia, we consider this to be an obstacle to adapting research findings to clinical practice.”
The research team conducted a systematic review of studies published in PubMed and Web of Science, estimating the prevalence of cachexia among cancer patients based on data from 125 articles published across 16 countries. This trial was registered at PROSPERO (CRD42023435474), a database for systematic reviews, to ensure transparency and adherence to research standards. They found that cachexia affected about 52% of patients in North America and Europe and approximately 29% in Asia. Overall, the global prevalence of cachexia in cancer patients was 33%. However, this rate varied significantly, ranging from approximately 13% to 56%, depending on the specific diagnostic criteria used.
The Fearon 2011 criteria (developed by the European Palliative Care Research Collaborative) are the most widely used for diagnosing cachexia, while the Evans 2008 criteria are less frequently employed. Cachexia prevalence is significantly higher with the Fearon criteria than with the Evans criteria. It is less common when factors like reduced energy intake, loss of appetite, inflammation, low muscle strength, or fatigue are included. “Sorting out the impact of different diagnostic criteria would allow us to select individuals with possible cachexia from a large population or to identify those with cachexia who are at high risk of death, leading to appropriate treatment,” explains Takaoka.
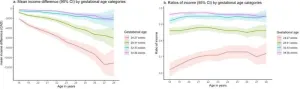
What was the impact of the different diagnostic criteria for cancer cachexia on patient outcomes? The team addressed this question through a meta-analysis exploring how cachexia diagnosis affected OS in cancer patients. They found that the OS varied depending on the prevalence of cachexia. Cachexia was linked to a higher risk of death compared to patients without cachexia, which varied in the definitive criteria used (the Fearon 2011 criteria had a lower hazard ratio for OS than the other criteria). The results showed that the risk of death was significantly higher when the prevalence of cachexia was low but plateaued at 40% to 50%. Generally, a higher cachexia risk is associated with poor survival in cancer patients, meaning that as the risk of cachexia rises, the survival chances decline.
Highlighting the important findings of their study, Takaoka emphasizes, “The definitive criteria for cachexia should match the goal of diagnosis. When the goal is to screen individuals at risk of cachexia, the broader, high-prevalence criteria are best suited. Conversely, when the goal is to identify a high-risk population for treatment, the stricter, low-prevalence criteria are more specific. In clinical practice, this measure can help identify patients needing intensive treatment of cachexia, including dietary changes and medication.”
Overall, this study highlights the importance of understanding the relationship between diagnostic criteria and patient survival. We hope this paves the way for improved treatment guidelines for cachexia in cancer patients to enhance response to therapies and OS.
###
About Shinshu University
Shinshu University is a national university founded in 1949 and located nestling under the Japanese Alps in Nagano known for its stunning natural landscapes. Our motto, "Powered by Nature - strengthening our network with society and applying nature to create innovative solutions for a better tomorrow" reflects the mission of fostering promising creative professionals and deepening the collaborative relationship with local communities, which leads to our contribution to regional development by innovation in various fields. We are working on providing solutions for building a sustainable society through interdisciplinary research fields: Material science (carbon, fiber and composites), biomedical science (for intractable diseases and preventive medicine) and mountain science, and aiming to boost research and innovation capability through collaborative projects with distinguished researchers from the world. For more information, visit https://www.shinshu-u.ac.jp/english/ or follow us on X (Twitter) @ShinshuUni for our latest news.
END