Under strict embargo: 16:00hrs GMT Wednesday 12 February 2025
Peer reviewed
Experimental study
Animals, people and cells
Researchers from the Francis Crick Institute have found that some particularly aggressive lung cancer cells can develop their own electric network, like that seen in the body’s nervous system.
This unique property could make them less dependent on the environment surrounding the tumour and even spread more easily.
Small cell lung cancer (SCLC) is one of the hardest types of cancer to treat and has often already spread by the time people are diagnosed. It mainly arises from neuroendocrine (NE) cells, which help regulate air and blood flow in the lungs.
In research published today in Nature, the team at the Crick looked for electrical activity in human and mouse SCLC samples, aiming to determine whether such activity may underpin the aggressiveness of this cancer type.
Using neuroscience techniques, they found that the SCLC cells had gone ‘off grid’. They were able to generate their own electrical activity, building their own electrical network within the tumour, and becoming independent of the body’s main electrical supply, including the nerves surrounding the tumour.
Keeping cancer cells fueled
Because firing electrical signals requires a lot of energy, the researchers investigated how this energy was being generated.
Over time, the team noted important changes in gene expression as the cancer progressed, resulting in some cells losing their NE identity and becoming non-neuroendocrine (non-NE) cancer cells.
They also observed that together, these cancer cells collaborated to promote tumour development. Genes enabling the electrical communication were switched on in the NE cells, and genes relating to producing a supportive environment were switched on in the non-NE cells.
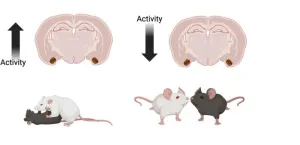
The researchers saw that the NE and non-NE cells were exhibiting a similar relationship to that of neurons and astroglia – the electrical brain cells and the neighbouring housekeeping cells that support them. Like processes seen in the brain, the non-NE cells were shuttling lactate, an alternative and efficient energy source for NE cells, to help power their electrical activity. Blocking the lactate pump decreased the electrical activity of NE cells, showing that this relationship is important for the tumour to support itself.
Electrical activity leads to aggression
Despite having the same cancer-causing changes in their DNA, the researchers saw in mice that the non-NE cells did not spread and start tumours elsewhere in the body. So, to determine the impact of electrical activity in the NE cells, the team used a toxin from puffer fish called tetrodotoxin (TTX), which suppresses electrical activity. They observed that TTX did not kill NE cells in a dish, but reduced their potential to form tumours long-term, with no effect on non-NE cells.
Finally, the team looked at molecular markers of increased electrical activity in a cohort of people with SCLC, finding that these markers were elevated in the cancer cells compared to adjacent healthy cells. They also observed that as the cancer progressed, non-NE cells showed markers suggesting they were increasingly pumping out lactate. These changes in the fueling pattern of NE cells is distinct from most other cancer types that can’t build their own electrical network.
Together, these results suggest that that the electrical activity of the NE cells is driving the tumour’s ability to grow and spread, a major cause of cancer death in patients.
Paola Peinado Fernandez, Postdoctoral Fellow and co-lead author on the study, said: “Our work shows that NE cells in SCLC have the ability to go ‘off-grid’, starting to generate their own electrical supply, and also being fueled by supportive non-NE cells rather than the energy sources used by most other cells.
“We’ve identified a feature which makes these types of cancers more aggressive and harder to treat. We think that this acquired autonomy of cancer cells might free them from the dependency of their environment.”
Leanne Li, Head of the Cancer-Neuroscience Laboratory at the Crick, said: “We knew that some cancer cells can mimic neural behaviour, but we didn’t know how developing an independent electrical network might impact the development of disease. By combining neuroscience and cancer research techniques, we’ve been able to look at this disease from a different perspective.
“There’s still a long way to go to understand the biological impact of this electrical activity and the specific disease mechanisms that make the tumour more aggressive and harder to treat. But we hope that in understanding the way these cancer cells are fueled, we can also expose vulnerabilities that could be targeted with future treatments.”
The next steps for the research team are to study the impact of electrical activity in other types of cancers and investigate whether targeting this property in small cell lung cancer could reveal new treatment options.
-ENDS-
For further information, contact: press@crick.ac.uk or +44 (0)20 3796 5252
Notes to Editors
Reference: Peinado, P., Stazi, M., Ballabio, C. et al. (2025). Intrinsic electrical activity drives small cell lung cancer progression. Nature. 10.1038/s41586-024-08575-7.
The Francis Crick Institute is a biomedical discovery institute with the mission of understanding the fundamental biology underlying health and disease. Its work helps improve our understanding of why disease develops which promotes discoveries into new ways to prevent, diagnose and treat disease.
An independent organisation, its founding partners are the Medical Research Council (MRC), Cancer Research UK, Wellcome, UCL (University College London), Imperial College London and King’s College London.
The Crick was formed in 2015, and in 2016 it moved into a brand new state-of-the-art building in central London which brings together 1500 scientists and support staff working collaboratively across disciplines, making it the biggest biomedical research facility under a single roof in Europe.
http://crick.ac.uk/
END