Editorial
War Takes a Toll on Family Doctors Trying to Care for Patients
Background: This issue of Annals of Family Medicine includes four articles discussing the impact of the Israeli/Palestinian conflict on family doctors and patients in the region. These articles offer perspectives from academic family doctors who have firsthand experience living and working in the region to reveal the complexity and impact of this conflict.
Editorial Stance: The decision to publish these articles was based on the idea that it is important to remember, support, and give voice to health care professionals and their patients who are living and working under horrifying conditions.
Why It Matters: Family doctors in conflict zones face extraordinary challenges while providing care in an environment shaped by violence and uncertainty. These articles look at how war affects both patients and health care workers, showing that beyond political issues, real people—including clinicians trying to care for their communities and patients trying to manage their symptoms—are enduring the consequences.
The Human Face of War
Caroline R. Richardson, MD, Editor in Chief
Annals of Family Medicine
The Warren Alpert Medical School, Brown University, Providence, RI
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Research Brief
Study Reveals Impact of Trauma on Health Care Professionals in Israel Following 2023 Terror Attack
Background and Goal: The October 7, 2023, terrorist attack in southern Israel forced the evacuation of countless individuals, placing intense demands on health care personnel. Primary care clinicians, who are at the forefront of treating severely traumatized evacuees, are often exposed to secondary trauma, which can affect their mental health and job performance. This study investigated the levels of burnout, well-being, and resilience among health care staff working in primary care clinics in Israel during the aftermath of the attack.
Study Approach: This cross-sectional study was conducted from October 15th to November 20th, 2023. Electronic questionnaires were distributed to 600 medical professionals, including family physicians, nurses, medical secretaries, and social workers from urban and rural clinics serving both Jewish and Arab sectors. The questionnaire included demographic questions and two validated questionnaires measuring burnout and positive mental health.
Results: A total of 129 health care professionals completed the survey, 78% of whom were female. The average age was 49 years, most were family physicians (68%), Israeli-born (82%), secular (78%), and Jewish (90%).
The study results indicate that health care professionals experienced a sense of significance and self-efficacy in treating evacuees, which positively contributed to their well-being. However, prolonged daily exposure, spanning over a month, to traumatized patients led to increased levels of depersonalization among the professionals. Health care professionals with more professional experience had better well-being scores and lower levels of mental exhaustion. Older health care workers experienced lower levels of emotional detachment from their work. Males reported higher levels of well-being than females. Why It Matters: The well-being of health care personnel is critical to maintaining the quality of care provided to trauma survivors.
The 2023 Terror Attack on Southern Israel: Well-Being and Burnout Among Health Care Personnel Treating Traumatized Evacuees
Dikla Agur Cohen, MD, MSc
Merav Sudarsky, MD
Department of Family Medicine, Ruth and Baruch Rappaport Faculty of Medicine, Technion - Israel Institute of Technology, Haifa, Israel
The Family Medicine Department, Clalit Health Services, Haifa and Western Galilee District, Israel
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
______________________________________________________________________
Essay
Physicians and Health Care Providers Struggle to Provide Care Amidst War in the Palestinian Territories
Background: The ongoing military occupation of the West Bank and Gaza since 1967 has created a fragmented health care system in the Occupied Territories of Palestine, exacerbated by the current war in Gaza. Family physicians and other clinicians face numerous challenges, including the lack of coordination between health institutions, disruptions in health care, threats of violence, scarce resources, and limited access to specialized care. In this essay, a family physician and her team in the southern West Bank describe their and other physicians’ challenges in the Occupied Territories of Palestine during the uncertainty of war.
Key Argument: With the Gaza War, physicians in the West Bank are grappling with severe disruptions in access to health centers due to checkpoints and road closures. Physicians also face the constant risk of violence and hospital raids that interrupt patient care. Witnessing the ongoing trauma to their patients and their own families carries a profound emotional toll. Despite these difficulties, physicians remain dedicated, even while facing burnout and emotional exhaustion.
Why It Matters: The personal accounts of physicians in the Occupied Territories of Palestine reveal the profound impact of occupation war on both clinicians and patients.
“We Haven’t Even Started Crying Yet:” Caring for the Family Under Occupation and War in the Occupied Palestinian Territories
Therese Zink, MD, MPH, et al
Family Medicine, Alpert School of Medicine, Brown University, Providence, Rhode Island
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
______________________________________________________________________
Essay
Healing In Conflict: Israeli Family Physician Shares Frontline Experiences of Care
Background: On October 7, 2023, Israel experienced a devastating attack when over 1,200 Israelis, including Jews, Christians, and Muslims, were killed or taken hostage by Hamas terrorists. Family doctors were suddenly responsible for treating patients amid ongoing rocket attacks and a heightened sense of insecurity, while entire communities faced displacement and psychological trauma. The author reflects on her experience providing care to displaced patients from diverse backgrounds at a temporary primary care clinic near the Dead Sea a week after the attack.
Key Argument: This essay highlights the significant burden placed on family doctors during wartime. These physicians treated injured patients, provided trauma-informed care, and offered emotional support in a time of extreme fear and uncertainty. The sorrow the author encountered in her volunteering experience served as a reminder of the parallel suffering endured by civilians in Gaza.
Why It Matters: This essay sheds light on the complex realities physicians face when caring for patients in wartime, demonstrating how they continue to deliver compassionate care despite immense challenges.
Healing Amidst Conflict: The Perspective of an Israeli Family Physician During Wartime
Dikla Agur Cohen, MD, MSc
Department of Family Medicine, Ruth and Baruch Rappaport Faculty of Medicine, Technion - Israel Institute of Technology, Haifa, Israel
The Family Medicine Department, Clalit Health Services, Haifa and Western Galilee District, Israel
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Special Report
Trauma Care and Mental Health Interventions Training Help Family Physicians Prepare for Times of War
Background and Goal: In wars and conflict, family physicians are frequently called on to serve in expanded roles and are witnesses to the enormous mental and physical suffering of individuals, families, communities, and populations. This special report examines the role of family physicians in the Israel–Hamas conflict and other current wars to inform future practices in family medicine.
Key Insights: Family physicians must share timely, accurate information with colleagues on all sides of the conflict while acknowledging the narratives of patients and other health care workers to foster understanding and reconciliation. Family physicians are urged to prepare for wartime service through expanded training in trauma care and mental health interventions, research, and social action to help shape policies that improve health outcomes during and after conflicts.
Why It Matters: This report highlights the need for family physicians to be prepared to handle both the immediate and long-term effects of war, including physical injuries, psychological trauma, and the disruption of health care systems.
Family Medicine in Times of War
Jeffrey M. Borkan, MD, PhD
Department of Family Medicine, The Warren Alpert Medical School of Brown University, Providence, Rhode Island
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Original Research
Within-Group Physician Visits Reduce Emergency Department Use Compared to Walk-In Clinic Visits
Background and Goal: Walk-in clinics offer a solution to patients’ difficulties booking same-day or next-day appointments with their regular family physician by providing care without an appointment. However, these clinics often disrupt continuity of care. This study compared the outcomes of patients who visited a physician from their own family physician group during after-hours versus those who visited an out-of-group walk-in clinic physician.
Study Approach: This retrospective study used claims data from Ontario, Canada, to compare patients who visited a physician within their family physician group for after-hours care with those who visited out-of-group walk-in clinics. Researchers examined emergency department visits within seven days of these appointments and other outcomes like follow-up visits with their regular physician. Patients in each group were matched to ensure comparable characteristics for analysis.
Main Results: The study identified 607,166 individuals who had their visit with a within-group physician during after-hours or on weekends, and 1,094,215 individuals who had their visit with an out-of-group walk-in clinic physician. After matching, there were 506,033 individuals in each group.
Patients who saw a within-group family physician after hours were 10% less likely to visit the emergency department within seven days than those who saw an out-of-group walk-in clinic physician. This difference was most evident in patients living in large urban areas and among children and adolescents. Those who saw a physician within their group were more likely to follow up with their own family physician or another doctor from their group the following week. Why It Matters: The findings suggest that maintaining continuity of care with a physician within their own family physician group, even for after-hours visits, can reduce unnecessary emergency department visits and may help improve patient outcomes and reduce health care costs.
Health Care Utilization After a Visit to a Within-Group Family Physician vs a Walk- In Clinic Physician
Lauren Lapointe-Shaw, MD, PhD, et al
Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada
Institute of Health Policy, Management and Evaluation, Department of Medicine, University of Toronto, Toronto, Ontario, Canada
Women's College Institute for Health System Solutions and Virtual Care, Women's College Hospital, Toronto, Ontario, Canada
Division of General Internal Medicine and Geriatrics, University Health Network and Sinai Health System, Toronto, Ontario, Canada
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
Visual Abstract
_____________________________________________________________________________________
Original Research
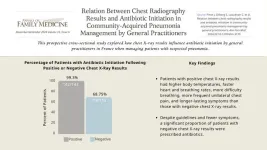
Antibiotics Initiated for Suspected Community-Acquired Pneumonia Even When Chest Radiography Results are Negative
Background and Goal: This study explored how chest X-ray results influence antibiotic initiation by general practitioners in France when managing patients with suspected pneumonia.
Study Approach: A prospective cross-sectional study was conducted with adult patients with suspected pneumonia who received chest X-rays as part of their evaluation. To analyze factors associated with antibiotic initiation, patients’ characteristics were compared at inclusion and at 28 days between patients with positive chest X-rays (indicating pneumonia) and patients with negative chest X-ray results.
Main Results: The sample included 259 adult patients. The median age was 58 years, 120 (46.3%) were male, 249 (96.1%) had not received antibiotics prior to inclusion, and 69 (26.7%) had at least one risk factor for pneumococcal disease.
Most of the general practitioners who included patients were women (55.2 %; n = 153), with a median age of 39 years. 76.1% (n = 210) were general practitioner trainers. 55.6% of patients (144 out of 259) had positive chest X-ray results. Patients with positive chest X-ray results had higher body temperature, faster heart rate, faster breathing rate, more difficulty breathing, and more frequent unilateral chest pain than patients with negative X-ray results, and their symptoms lasted for a longer time. 99.3% of patients with positive chest X-ray results received antibiotics. Despite fewer symptoms and negative chest X-ray results, a significant portion (68.75%) of patients with negative chest X-ray results were prescribed antibiotics (79/115 patients). Why It Matters: The findings of this study show that many general practitioners prescribe antibiotics for suspected community-acquired pneumonia even when chest X-ray results are negative, highlighting a gap between guidelines and actual practice.
Relationship Between Chest Radiography Results and Antibiotic Initiation in Community-Acquired Pneumonia Management by General Practitioners
Juliette Pinot, MD, et al
Université Paris Cité and Université Sorbonne Paris Nord, INSERM, IAME, Paris, France
Université Paris Cité, Department of General Practice, Paris, France
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
Visual Abstract
_____________________________________________________________________________________
Original Research
Restrictive Abortion Laws Weaken Training Confidence Among Family Medicine Professionals
Background and Goal: The 2022 Supreme Court decision in Dobbs v. Jackson Women’s Health Organization removed federal protections for abortion, allowing individual states to establish their own laws. This study evaluated perceived impacts of state abortion legislation on clinical practice and medical education regarding reproductive health care within the discipline of family medicine.
Study Approach: The study utilized data from a national survey conducted by the Council of Academic Family Medicine, a joint initiative of four major academic family medicine organizations to support the leadership, research and education of the discipline. The survey measured changes in clinical practice, legal concerns, patient-clinician trust, and medical training since the Dobbs decision.
Main Results: Data from 1,196 respondents were analyzed.
Of the 1,196 respondents, 49.7% reported working in states with very restrictive or restrictive abortion policies. Among the 991 respondents with clinical responsibilities, significant differences were observed in counseling practices, clinical decision making, worry about legal risks, and trust in patients’ self-reported reproductive medical history compared to peers in unrestricted states. Perceived trust from patients toward clinicians remained unchanged. Respondents in states with restrictive abortion policies also reported significantly reduced confidence in resident training programs and a decrease in program desirability. Why It Matters: The findings highlight that restrictive state abortion laws are already influencing how family medicine clinicians practice and how they train future health care professionals. Without clear guidelines, clinicians face legal uncertainties, which may affect their ability to provide comprehensive reproductive care.
Impact of State Abortion Policies on Family Medicine Practice and Training and Training After Dobbs v Jackson Women’s Health Organization
Karen L. Roper, PhD, et al
Department of Family and Community Medicine, University of Kentucky, Lexington, Kentucky
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
Visual Abstract
___________________________________________________________________________________
Original Research
Collaborative, Trauma-Informed Care Improves Depression Outcomes in Primary Care
Background and Goal: Depression is a major public health issue in Chile, affecting women at twice the rate of men. Many patients experience complex forms of depression that are linked to trauma and other challenges, which standard treatments often fail to address. This study aimed to assess whether a collaborative, trauma-informed care model could improve outcomes for patients with depression compared to usual treatment in primary care clinics in Chile.
Study Approach: The study was a cluster randomized controlled trial conducted with 16 primary care teams in the Maule Region, Chile, from August 2021 to June 2023. A total of 214 adult patients between 18 and 70 years old with diagnosed depression were recruited and monitored over a six-month period, with evaluations at three and six months. Collaborative, trauma-informed care model teams consisted of a physician, a psychologist, and a social worker, all trained in trauma-informed care and in managing difficult-to-treat depression.
Main Results: 214 patients were recruited, 85% women, with 61.2% having 4 or more adverse childhood experiences.
Depression scores dropped significantly in both groups, but the collaborative trauma-informed care model group saw a greater reduction—from 17.1 to 8.9—compared to the usual treatment group, which improved from 17.3 to 12.2. At six months, 62 out of 115 patients (54%) in the collaborative trauma-informed care model group showed remission, compared to 34 out of 99 patients (34%) in the usual treatment group. Patients in the collaborative trauma-informed care model group had higher treatment compliance. Both the collaborative trauma-informed care model and usual treatment groups showed improvements in anxiety, social functioning, and emotional regulation, with no significant differences between groups in these areas. Why It Matters: This study demonstrates the effectiveness of integrating trauma-informed care into a collaborative care model for treating complex forms of depression, particularly those complicated by past trauma, in primary care.
Effectiveness of Collaborative, Trauma-Informed Care on Depression Outcomes in Primary Care: A Cluster Randomized Control Trial in Chile
Verónica G. Vitriol, MD, Mg, et al
University of Talca Medical School, Talca, Chile
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
Visual Abstract
______________________________________________________________________________
Original Research
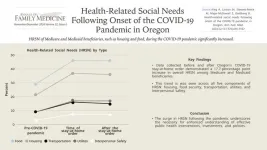
COVID-19 Stay-at-Home Order Increased Reporting of Food, Housing, and Other Health-Related Social Needs in Oregon
Background and Goal: Efforts to address the health-related social needs (HRSN) of Medicare and Medicaid beneficiaries, such as housing and food, during the COVID-19 pandemic were insufficient. This research examined HRSN data from the Accountable Health Communities (AHC) study collected in Oregon to understand changes in HRSN for Medicare and Medicaid beneficiaries at the onset and during the first two years of the pandemic.
Study Approach: The study sample included 21,522 Medicare and Medicaid beneficiaries screened for overall health-related social needs between May 13, 2019 and December 24, 2021. An interrupted time series analysis was used to analyze both the immediate effects and the long-term trend changes in Medicare and Medicaid beneficiary-reported HRSN following Oregon’s stay-at-home order.
Main Results: A total of 21,522 unique Medicare and Medicaid beneficiaries participated in AHC in Oregon between May 13, 2019 and December 24, 2021: 8,234 before the March 23, 2020 stay-at-home order, and 13,288 following the order.
There was an abrupt 17.7 percentage point increase in overall health-related social needs around March 23, 2020 (onset of stay-at-home order) which did not significantly decline during the study period. The percentage of beneficiaries reporting food, housing, and interpersonal safety needs increased by 16.5, 15.9, and 4.4 percentage points, respectively, with no significant decline during the study period. The percentage of beneficiaries reporting transportation and utility needs increased by 7.5 and 7.2 percentage points, respectively, but decreased significantly after the start of the pandemic. Why It Matters: The jump in the number of people reporting health-related social needs following the start of the pandemic and the persistence of needs, particularly in housing, point to a need for increased understanding of which public health and health care interventions, investments, and policies effectively address health-related social needs.
Health-Related Social Needs Following Onset of the COVID-19 Pandemic in Oregon
Anne King, MBA, et al
Oregon Rural Practice-based Research Network, Oregon Health & Science University, Portland, Oregon
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
Visual Abstract
_____________________________________________________________________________________
Original Research
Fear of Positive Results and Stigma Hinder HIV Self-Testing, While Routine Use and Protecting Loved Ones Motivates University Students
Background and Goal: Despite efforts to increase HIV testing and treatment, traditional services have not effectively reached marginalized communities. HIV self testing (HIVST) offers a discreet and accessible alternative, potentially improving testing rates among at-risk populations, including university students in Kenya. This study assessed the awareness and acceptance of HIVST among undergraduate students.
Study Approach: This cross-sectional analytical study employed a multi-stage cluster
sampling technique among undergraduate students aged 18-21 years at Kenyatta University. Clusters from various academic departments were randomly selected, and individual students were chosen for participation until the desired sample size of 398 participants was reached. Data were collected through questionnaires administered by trained enumerators.
Main Results: Participants’ age averaged 21.1 years, with a majority being single, female, and full-time students.
Substantial HIV knowledge was observed, and nearly half were aware of pre-exposure prophylaxis (47.7%).
The majority of students have tested for HIV (65.3%), with a majority not using a self test kit (75.6%).
Only 24.4% of students used a self test kit.
45.4% of students said they would prefer to use a self test kit rather than go to a facility.
Fear of positive results and stigma were primary barriers for self testing, while motivations for self testing included routine use and protecting loved ones.
Media exposure, especially the "Chukua Selfie" campaign, correlated with higher HIVST usage.
Why It Matters: Participants' substantial knowledge of HIV contrasts with findings from other regions, underscoring the need for targeted education and safe sex promotion. Addressing fear and stigma through comprehensive interventions is essential for improving HIVST uptake.
Exploring HIV Self-Testing: Barriers and Facilitators Among Undergraduate Students in Nairobi, Kenya
Nicholas Kyalo Muendo, MBChB, MSc, MMed, et al
Department of Family Medicine, Kenyatta University, Nairobi, Kenya
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
Visual Abstract
_____________________________________________________________________________________
Research Brief
Direct Primary Care Practices More Common in Rural Regions
Background and Goal: Direct primary care (DPC) is a model where patients pay a membership fee to a physician who provides your primary care, bypassing insurance. This study explored how often health professional shortage areas overlap with DPC practices across the U.S.
Study Approach: The researchers collected data on DPC practices from public sources and compared their locations to health professional shortage areas in the U.S. They also compared DPC practices to insurance-based primary care physicians to see if there were differences in where they were located. Analyses were stratified by degree of rurality and health professional shortage area priority need scores.
Main Results: As of the date of download, there were 3,935 population-based health professional shortage areas in the U.S. Over 2,100 DPC practices were identified.
44% of Direct Primary Care (DPC) practices were located in health professional shortage areas, slightly lower than the 47% of insurance-based primary care physicians in health professional shortage areas.
DPC practices were more often found in low- and medium-priority need areas within health professional shortage areas (45% in low-need, 47% in medium-need). In contrast, 20% of insurance-based primary care physicians were in high-priority need areas, compared to 14% of DPCs.
25% of DPCs in Health Professional Shortage Areas were located in rural areas, and 22% were in partially rural areas. Insurance-based primary care physicians were more concentrated in non-rural areas (63% of insurance-based primary care physicians versus 53% of DPCs).
Why It Matters: These findings suggest that, while DPCs do not currently serve the most underserved populations overall, their success in rural areas—traditionally a challenging environment for primary care—indicates that this model could be scalable in other underserved regions.
Are Direct Primary Care Practices Located in Health Professional Shortage Areas?
Neal D. Goldstein, PhD, MBI, et al
Department of Epidemiology & Biostatistics, Drexel University Dornsife School of Public Health, Philadelphia, Pennsylvania
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_________________________________________________________________________________
Methodology
Adapted Nominal Group Technique Effectively Builds Consensus on Health Care Priorities for Older Adults
Background and Goal: The participatory research approach is an important tool of family medicine and primary health care research. However, standard consensus methods like the Delphi and nominal group techniques can be time consuming and may not represent a broad range of opinions. To address these issues, researchers developed an adapted nominal group technique (aNGT) to efficiently build consensus among stakeholders with diverse perspectives.
Approach: This study focused on shaping care trajectories for adults aged 65 and older, aiming to prioritize key domains and identify new care indicators. Researchers used four main strategies: (1) recruiting four diverse stakeholder groups (older adults, clinicians, managers, and decision makers); (2) using remote tools to maximize participation; (3) adding a pre-elicitation activity so participants could individually review study materials and rank domains before group discussions; and (4) tailoring discussions to each group’s needs, including scheduling meetings around lunch for clinicians and avoiding jargon.
Main Results: Of 28 participants who completed the questionnaire, 20 joined a group discussion. Through the pre-elicitation activity and one round of discussions, participants reached a consensus on prioritizing “symptoms, functioning, and quality of care.” Tailored discussions and remote tools were the most effective strategies.
Why It Matters: By addressing traditional consensus-building challenges, the aNGT fosters inclusivity, efficiency, and relevance, making it a valuable approach for research that informs care standards.
Building Timely Consensus Among Diverse Stakeholders: An Adapted Nominal Group Technique
Deniz Cetin-Sahin, MD, PhD, et al
Lady Davis Institute for Medical Research at the Jewish General Hospital, Montreal, Quebec, Canada
Department of Family Medicine, McGill University, Montreal, Quebec, Canada
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Special Report
New Report Looks at Strategies for Primary Care Professionals to Combat Diabetes
Background and Goal: Diabetes is a growing public health issue in the U.S., affecting 38.4 million people and placing a significant burden on primary care services. Primary care professionals play a key role in managing this complex, chronic condition. This report explores strategies to improve diabetes care.
Key Insights: Team-based care models have been effective in improving diabetes care. However, current payment structures do not sufficiently reimburse non-physician health care professionals, limiting the success of these models. Reforming payment systems to support all care team members, emphasizing preventive care, and improving access to primary care among racial and ethnic minorities is necessary to address health disparities.
Why It Matters: This report highlights the need for national policy changes to support primary care teams, including workforce expansion, team-based care approaches, and payment reform.
Diabetes Management: A Case Study to Drive National Policy Change in Primary Care Settings
Lisa Murdock, et al
American Diabetes Association, Arlington, Virginia
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
____________________________________________________________________________________
Special Report
Primary Care Settings Face Barriers to Screening For Early Detection of Cognitive Impairment
Background and Goal: Early detection of cognitive impairment is essential for improving patient outcomes, but primary care settings face significant challenges in screening. This special report summarizes key points and gaps in knowledge about methods for detecting cognitive impairment in primary care clinics.
Key Insights: The report highlights the importance of addressing the rising incidence of cognitive impairment as the population ages, particularly with new treatments for early Alzheimer’s disease now available. It advocates for creative solutions to manage the increased workload, such as partnering with community health workers and leveraging telehealth. The report emphasizes the importance of developing cognitive care plans, especially for vulnerable populations, and outlines the need for clear roles between primary care physicians and specialists in managing cognitive disorders.
Why It Matters: By removing barriers to screening and promoting collaboration between primary care and specialists, more patients can be identified earlier and receive the care they need.
Improving Early Detection of Cognitive Impairment in Older Adults in Primary Care
Clinics: Recommendations From an Interdisciplinary Geriatrics Summit
Robin C. Hilsabeck, PhD, et al
National Academy of Neuropsychology, Denver, Colorado
The University of Texas at Austin Dell Medical School, Austin, Texas
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Theory
Unhurried Conversations: A Must Have For Patient-Centered Care
Background and Theory Overview: The theory behind “unhurried conversations” in health care emphasizes the importance of slowing down medical interactions to enable patient care. The approach identifies behaviors that patients and clinicians could enact within the context of the health care system in which they meet to “deepen” the interaction so that participants can work together to advance the patient’s situation.
What is New: This article identifies and elaborates on ten observable and key micro-level patient-clinician communication practices that support unhurried conversations and outlines specific strategies for clinicians and patients to adopt. The article also provides guidance on how health systems can enable unhurried conversations by adjusting workflows and rethinking productivity metrics to prioritize patient-centered care.
Why It Matters: By adopting unhurried conversations, clinicians can improve the quality of the care they give and their relationships with patients in achieving care that fits.
Unhurried Conversations in Health Care Are More Important Than Ever: Identifying Key Communication Practices for Careful and Kind Care
Victor M. Montori, MD, et al
Knowledge & Evaluation Research Unit, Mayo Clinic, Rochester, Minnesota
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Innovations in Primary Care
New Process Shortens Wait Times for Diagnosis and Treatment for ADHD and Other Psychiatric Conditions
A suburban family medicine residency clinic implemented an innovative approach to reduce behavioral health clinic wait times for adult ADHD diagnosis and treatment.During their first visit, patients completed self-administered screening tools for ADHD and potential co-occurring conditions such as depression, anxiety, and substance abuse. If ADHD was suspected, patients reviewed a diagnostic interview tool (DIVA-5) at home and returned for a second visit where clinicians confirmed the ADHD diagnosis if applicable, and offered treatment, including medication initiation.
The new process decreased wait times for diagnosis and treatment by 46-96% compared to behavioral health referrals, significantly improving care access and patient satisfaction and increased the clinic’s ability to manage complex psychiatric conditions with a low-cost and adaptable solution.
Adult ADHD Diagnosis in a Family Medicine Clinic
Deborah M. Mullen, PhD, et al
The University of Tennessee at Chattanooga, Chattanooga, Tennessee
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Essay
PACE Program and Team-Based Care Fill Gaps in Treating Patient With Complex Medical Conditions and Intellectual Disabilities
Background: The essay focuses on the care of a 70-year-old patient, Ervin, who has complex medical conditions and intellectual disabilities, in a Program of All-Inclusive Care for the Elderly (PACE) setting. The essay discusses the challenges of providing ethical medical and supportive care to individuals like Ervin, who often face complicated health and social issues.
Key Argument: Ervin’s story reveals significant challenges in the U.S. health care system, including gaps in social safety nets and ethical questions around caring for patients with reduced decision-making capacity. Programs like PACE address some of these gaps through more personalized, team-based care.
Why It Matters: This essay stresses the importance of integrating medical care with social support to improve outcomes and build stronger connections between patients with complex medical and social needs and their care teams.
Learning From Ervin’s Care: Ethics, Health Care Finance, and Human Connection
Amy C. Denham, MD, MPH
University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, North Carolina
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
_____________________________________________________________________________________
Innovations in Primary Care
Single-Visit First-Trimester Care With Point-of-Care Ultrasound Cuts Emergency Visits by 81% for Non-Miscarrying Patients
The Bethesda Family Medicine Clinic in St. Paul, Minnesota, established a bi-monthly Early Pregnancy Dating & Risk Assessment Clinic in September 2022. The clinic introduced an integrated approach, combining point-of-care ultrasound with immediate, multidisciplinary first-trimester care. This integration allowed the clinic to quickly identify high-risk cases and offer timely intervention for issues such as miscarriage or abnormal pregnancies, reducing emergency visits, urgent clinic appointments, and first-trimester phone inquiries by 81% for non-miscarrying patients. Clinic implementation led to more timely diagnosis of abnormal pregnancies and improved education and support for all patients, including those who experience miscarriage.
Enhancing First Trimester Obstetrical Care: The Addition of Point-of-Care Ultrasound
Allison Newman, MD, et al
Woodwinds Hospital Family Medicine Residency Program, Department of Family Medicine and Community Health, University of Minnesota Medical School, St. Paul, Minnesota
PRE-EMBARGO LINK (Link expires at 5 p.m. ET November 25, 2024)
PERMANENT LINK
________________________________________________________________________
END