“This therapy is the first to deliver mRNA-based treatments inside the eye,” said co-corresponding author of the study Leo A. Kim, MD, PhD, the Monte J. Wallace Ophthalmology Chair in Retina at Massachusetts Eye and Ear. “We were pleasantly surprised that we could even use this approach inside the eye without causing excessive inflammation. We hope that these early findings can usher in new treatment options for PVR and other eye diseases.”
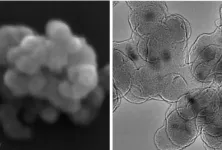
PVR is scar tissue that forms inside the eye, commonly after eye trauma, that can contract and detach the retina. This pathologic scar tissue response, rather than the eye injury itself, is what can lead to blindness.
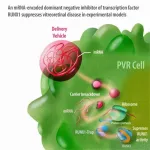
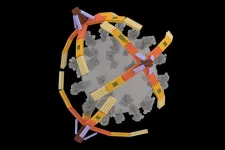
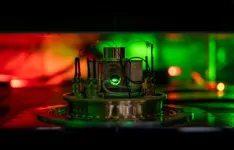
In the new paper, the researchers detail preclinical studies using mRNA as a therapeutic in the eye. Messenger RNA, or mRNA, is an essential part of every single cell in the body. Cells copy the code of genes into pieces of RNA and these RNAs act as messengers that ferry the genetic codes to the ribosomes, which use it to create proteins. Strands of mRNA can code for any protein — even ones not in the cell’s genome. When introduced into cells, the cellular machinery turns these mRNAs into proteins. Proteins make up the structure of the cell and help it carry out its functions. They can also turn other genes on or off.
In the new study, the research team used cell-based, tissue-based, and preclinical models of proliferative vitreoretinopathy and abnormal blood vessel growth to show that mRNA-based therapeutics can be used safely in the eye.
The researchers developed and studied the efficacy of various mRNAs encoding for proteins related to the scar tissue formation to see which might be useful as a therapeutic. To develop a treatment for PVR, the researchers targeted a protein called RUNX1 that regulates the expression of a gene that turns eye cells into scar tissue. Earlier in their careers, Kim and study co-corresponding author Joseph Arboleda-Velasquez, MD, PhD, discovered that RUNX1 was involved in two processes seen in several retinal diseases: the formation of abnormal blood vessels, called aberrant angiogenesis, and scar tissue, or fibrosis. In PVR and other diseases, the gene that RUNX1 regulates is overexpressed in the eye, causing scar tissue and abnormal blood vessels to grow.
The investigators initially believed that targeting RUNX1 was the best approach, but current technologies were limited. mRNA is primarily used to increase protein expression, whereas the issue in PVR was excessive RUNX1. A key insight for developing this new experimental therapy was the idea of creating a molecule that would trap RUNX1 and inhibit its function—a strategy known as a dominant-negative inhibitor in biology. These dominant negative molecules are powerful and their effects cannot be easily compensated by cells.
They settled on an mRNA called RUNX1-Trap, which keeps RUNX1 in a cell’s cytoplasm, preventing it from entering the nucleus and turning on the gene that turns the cells into scar tissue. They saw that in patient-derived cells in a lab culture, in an animal model, and in patient tissues in the lab, treating the cells with this mRNA helped stop the development of scar tissue and abnormal blood vessels.
The researchers consider this study a proof of concept that suggests that the mRNA approach may be useful for PVR and other eye diseases. The study’s limitations include that the experiments were in cellular and preclinical models. This approach has not been tested in human subjects. The technology itself may have some limitations as mRNA doesn’t remain in the cell very long making proteins. Thus, the researchers don’t know how long the effects of one treatment may last or whether a patient may require multiple doses over weeks or months for the treatment to effectively prevent PVR.
The researchers are now looking at ways to extend the half-life of the mRNA so that it can last longer and to determine the optimal timing of the treatment to ensure the mRNA gets in the eye at the right time. Since RUNX1 is active in other diseases, the researchers also hope to apply their mRNA system and RUNX1-Trap therapy to treat other retinal conditions like wet age-related macular degeneration and diabetic retinopathy.
“We believe targeting RUNX1 could lead to new therapies for sight-threatening conditions,” said Arboleda- Velasquez, an associate scientist at Mass Eye and Ear. “The same idea of making dominant negative molecules produced using mRNA could result in the generation of potentially effective treatments for other conditions, greatly expanding the potential uses for mRNA,” added Arboleda- Velasquez.
Study co-first author William P. Miller, PhD, a postdoctoral fellow in the Department of Ophthalmology at Mass Eye and Ear and Harvard Medical School, noted, “This work is the result of substantial effort put forth by our team, encompassing multiple experts across several different fields. It demonstrates novel applications of mRNA technology in ophthalmology and has implications for other aspects of medicine as well.”
Authorship: Kim is a co-corresponding author with Arboleda-Velasquez and Fabio Montrasio (CureVac). Other Mass Eye and Ear co-authors include Michael O’Hare, William P. Miller, Said Arevalo-Alquichire, Dhanesh Amarnani, Evhy Apryani, Paula Perez-Corredor, Claudia Marino, Daisy Y. Shu, Timothy E. Vanderleest, Andres Muriel-Torres, Harper B. Gordon, Audrey L. Gunawan, Bryan A. Kaplan, Karim W. Barake, Romy P. Bejjani, Tri Huu Doan, Rose Lin, Santiago Delgado-Tirado, Lucia Gonzalez-Buendia, Elizabeth Rossin, Guannan Zhao, and Dean Eliott. Additional co-authors at CureVac include Christine Weinl-Tenbruck, Frédéric Chevessier-Tünnesen, and Joanna Rejman.
Disclosures: The company CureVac sponsored this research. Kim and Arboleda-Velasquez are co-inventors on various patents and patent applications covering the use of RUNX1 inhibitors and mRNA in the treatment of proliferative vitreoretinopathy and conditions associated with epithelial to mesenchymal transition.
Funding: This study was funded by a sponsored research agreement from CureVac. Kim has funding from Michel Plantevin and the Monte J. Wallace Ophthalmology Chair in Retina.
Paper cited: O’hare, M. et al. “mRNA-encoded RUNX1-Trap: a RUNX1 inhibitor with potent antiproliferative effects” Science Translational Medicine. DOI: 10.1126/scitranslmed.adh0994
###
About Mass Eye and Ear
Massachusetts Eye and Ear, founded in 1824, is an international center for treatment and research and a teaching hospital of Harvard Medical School. A member of Mass General Brigham, Mass Eye and Ear specializes in ophthalmology (eye care) and otolaryngology–head and neck surgery (ear, nose and throat care). Mass Eye and Ear clinicians provide care ranging from the routine to the very complex. Also home to the world's largest community of hearing and vision researchers, Mass Eye and Ear scientists are driven by a mission to discover the basic biology underlying conditions affecting the eyes, ears, nose, throat, head and neck and to develop new treatments and cures. In the 2024–2025 “Best Hospitals Survey,” U.S. News & World Report ranked Mass Eye and Ear #4 in the nation for eye care and #6 for ear, nose and throat care. For more information about life-changing care and research at Mass Eye and Ear, visit our blog, Focus, and follow us on Instagram, Twitter and Facebook.
END